J Korean Med Assoc.
2014 Jun;57(6):500-507. 10.5124/jkma.2014.57.6.500.
Perioperative nutritional therapy for surgical patients
- Affiliations
-
- 1Department of Surgery, Dongtan Sacred Heart Hospital, Hallym University College of Medicine, Hwaseong, Korea. shin519@hallym.or.kr
- KMID: 1958087
- DOI: http://doi.org/10.5124/jkma.2014.57.6.500
Abstract
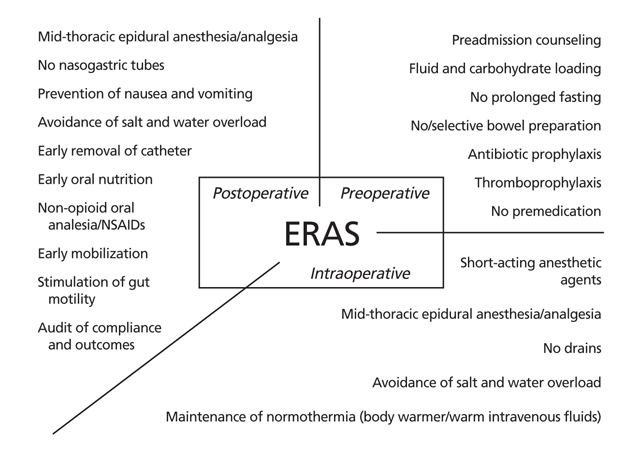
- Malnutrition of hospitalized patients is a prevailing issue, especially in the perioperative period. As the elderly population increases progressively, surgeons should become more alert to preventing the risk of iatrogenic malnutrition. The consequences of malnutrition, such as delayed wound healing, exposure to infection, pressure sores, gastrointestinal bacterial overgrowth, and compromised immunity can be prevented or attenuated by vigorous nutritional support. Enhanced recovery after surgery is a multimodal perioperative care pathway designed to achieve early recovery for patients undergoing major surgery, in which nutritional intervention is the most important and integral part. Preoperative nutritional assessment, intraoperative considerations against postoperative nutritional problems, and an appropriate postoperative nutritional supply will result in better outcomes of surgery, and, in turn, in reduced postoperative complications, shorter hospital stays, and decreased medical costs. Though enteral nutrition is preferable over parenteral nutrition, parenteral nutrition should be supplemented selectively in those for whom enteral nutrition will inevitably be inadequate.
MeSH Terms
Figure
Cited by 1 articles
-
Nutritional therapy uptodate
Dongwoo Shin
J Korean Med Assoc. 2014;57(6):488-490. doi: 10.5124/jkma.2014.57.6.488.
Reference
-
1. Bruun LI, Bosaeus I, Bergstad I, Nygaard K. Prevalence of malnutrition in surgical patients: evaluation of nutritional support and documentation. Clin Nutr. 1999; 18:141–147.
Article2. Drover JW, Cahill NE, Kutsogiannis J, Pagliarello G, Wischmeyer P, Wang M, Day AG, Heyland DK. Nutrition therapy for the critically ill surgical patient: we need to do better. JPEN J Parenter Enteral Nutr. 2010; 34:644–652.
Article3. Santos JI. Nutrition, infection, and immunocompetence. Infect Dis Clin North Am. 1994; 8:243–267.
Article4. Mainous MR, Deitch EA. Nutrition and infection. Surg Clin North Am. 1994; 74:659–676.
Article5. Haydock DA, Hill GL. Impaired wound healing in surgical patients with varying degrees of malnutrition. JPEN J Parenter Enteral Nutr. 1986; 10:550–554.
Article6. Albina JE. Nutrition and wound healing. JPEN J Parenter Enteral Nutr. 1994; 18:367–376.
Article7. Kehlet H, Wilmore DW. Fast-track surgery. Br J Surg. 2005; 92:3–4.
Article8. Fearon KC, Ljungqvist O, Von Meyenfeldt M, Revhaug A, Dejong CH, Lassen K, Nygren J, Hausel J, Soop M, Andersen J, Kehlet H. Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr. 2005; 24:466–477.
Article9. Varadhan KK, Lobo DN, Ljungqvist O. Enhanced recovery after surgery: the future of improving surgical care. Crit Care Clin. 2010; 26:527–547.
Article10. Awad S, Varadhan KK, Ljungqvist O, Lobo DN. A meta-analysis of randomised controlled trials on preoperative oral carbohydrate treatment in elective surgery. Clin Nutr. 2013; 32:34–44.
Article11. Brady M, Kinn S, Ness V, O'Rourke K, Randhawa N, Stuart P. Preoperative fasting for preventing perioperative complications in children. Cochrane Database Syst Rev. 2009; (4):CD005285.
Article12. Brady M, Kinn S, Stuart P. Preoperative fasting for adults to prevent perioperative complications. Cochrane Database Syst Rev. 2003; (4):CD004423.
Article13. Cao F, Li J, Li F. Mechanical bowel preparation for elective colorectal surgery: updated systematic review and meta-analysis. Int J Colorectal Dis. 2012; 27:803–810.
Article14. Jorgensen H, Wetterslev J, Moiniche S, Dahl JB. Epidural local anaesthetics versus opioid-based analgesic regimens on postoperative gastrointestinal paralysis, PONV and pain after abdominal surgery. Cochrane Database Syst Rev. 2000; (4):CD001893.15. Rodgers A, Walker N, Schug S, McKee A, Kehlet H, van Zundert A, Sage D, Futter M, Saville G, Clark T, MacMahon S. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomised trials. BMJ. 2000; 321:1493.
Article16. Gan TJ, Meyer T, Apfel CC, Chung F, Davis PJ, Eubanks S, Kovac A, Philip BK, Sessler DI, Temo J, Tramer MR, Watcha M. Department of Anesthesiology, Duke University Medical Center. Consensus guidelines for managing postoperative nausea and vomiting. Anesth Analg. 2003; 97:62–71.
Article17. Waldhausen JH, Shaffrey ME, Skenderis BS 2nd, Jones RS, Schirmer BD. Gastrointestinal myoelectric and clinical patterns of recovery after laparotomy. Ann Surg. 1990; 211:777–784.
Article18. Mueller C, Compher C, Ellen DM. American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Board of Directors. A.S.P.E.N. clinical guidelines: nutrition screening, assessment, and intervention in adults. JPEN J Parenter Enteral Nutr. 2011; 35:16–24.19. Jie B, Jiang ZM, Nolan MT, Zhu SN, Yu K, Kondrup J. Impact of preoperative nutritional support on clinical outcome in abdominal surgical patients at nutritional risk. Nutrition. 2012; 28:1022–1027.
Article20. Senkal M, Zumtobel V, Bauer KH, Marpe B, Wolfram G, Frei A, Eickhoff U, Kemen M. Outcome and cost-effectiveness of perioperative enteral immunonutrition in patients undergoing elective upper gastrointestinal tract surgery: a prospective randomized study. Arch Surg. 1999; 134:1309–1316.
Article21. American Society of Anesthesiologists Committee. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists Committee on Standards and Practice Parameters. Anesthesiology. 2011; 114:495–511.22. Gutierrez MC, Moore PG, Liu H. Goal-directed therapy in intraoperative fluid and hemodynamic management. J Biomed Res. 2013; 27:357–365.
Article23. Rinehart J, Liu N, Alexander B, Cannesson M. Review article: closed-loop systems in anesthesia: is there a potential for closed-loop fluid management and hemodynamic optimization? Anesth Analg. 2012; 114:130–143.24. Osland E, Yunus RM, Khan S, Memon MA. Early versus traditional postoperative feeding in patients undergoing resectional gastrointestinal surgery: a meta-analysis. JPEN J Parenter Enteral Nutr. 2011; 35:473–487.
Article25. Lewis SJ, Andersen HK, Thomas S. Early enteral nutrition within 24 h of intestinal surgery versus later commencement of feeding: a systematic review and meta-analysis. J Gastrointest Surg. 2009; 13:569–575.
Article26. Gwon JG, Lee YJ, Kyoung KH, Kim YH, Hong SK. Enteral nutrition associated non-occlusive bowel ischemia. J Korean Surg Soc. 2012; 83:171–174.
Article27. Mo JA, Lee SH, Jeon MH, Kim KS, Kim HS, Jang JY, Lee MD. Efficacy of feeding pump for patients on enteral tube feeding: a systematic literature review and analysis. Korean J Gastroenterol. 2014; 63:99–106.
Article28. Braga M, Ljungqvist O, Soeters P, Fearon K, Weimann A, Bozzetti F. ESPEN. ESPEN guidelines on parenteral nutrition: surgery. Clin Nutr. 2009; 28:378–386.
Article29. Casaer MP, Mesotten D, Hermans G, Wouters PJ, Schetz M, Meyfroidt G, Van Cromphaut S, Ingels C, Meersseman P, Muller J, Vlasselaers D, Debaveye Y, Desmet L, Dubois J, Van Assche A, Vanderheyden S, Wilmer A, Van den Berghe G. Early versus late parenteral nutrition in critically ill adults. N Engl J Med. 2011; 365:506–517.
Article30. Vanderheyden S, Casaer MP, Kesteloot K, Simoens S, De Rijdt T, Peers G, Wouters PJ, Coenegrachts J, Grieten T, Polders K, Maes A, Wilmer A, Dubois J, Van den Berghe G, Mesotten D. Early versus late parenteral nutrition in ICU patients: cost analysis of the EPaNIC trial. Crit Care. 2012; 16:R96.
Article31. Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb SA, Beale RJ, Vincent JL, Moreno R. Surviving Sepsis Campaign Guidelines Committee including the Pediatric Subgroup. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013; 41:580–637.
Article32. Doig GS, Heighes PT, Simpson F, Sweetman EA. Early enteral nutrition reduces mortality in trauma patients requiring intensive care: a meta-analysis of randomised controlled trials. Injury. 2011; 42:50–56.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Perioperative Nutritional Support
- Perioperative Nutritional Management in Cardiac Surgery
- Perioperative nutrition support: a narrative review
- Management of perioperative volume therapy – monitoring and pitfalls
- Perioperative nutritional practices and attitudes among gastrointestinal oncologic surgeons in Korea: a nation-wide survey study