Infect Chemother.
2011 Aug;43(4):359-362. 10.3947/ic.2011.43.4.359.
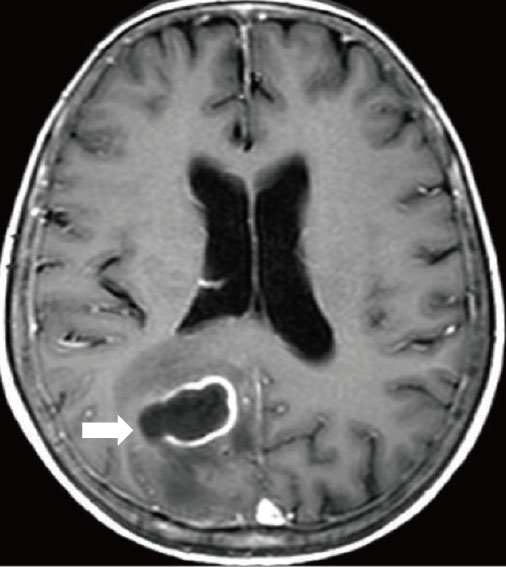
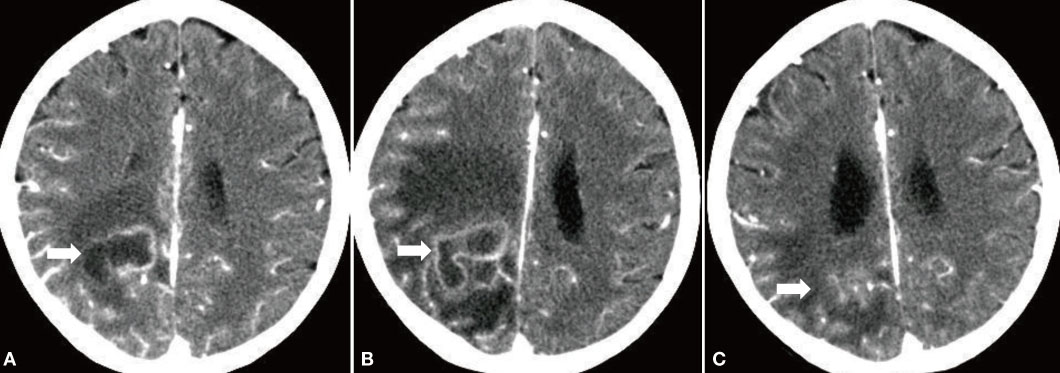
A Case of Bain Abscess caused by Mycobacterium intracellurare
- Affiliations
-
- 1Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea. joonsup.yeom@gmail.com
- 2Department of Neurosurgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 1936074
- DOI: http://doi.org/10.3947/ic.2011.43.4.359
Abstract
- Mycobacterium avium intracellulare complex (MAC) usually causes an opportunistic pulmonary infection in immunocompromised hosts who have underlying structural lung disease. Central nervous system infection due to MAC is very rare even in an immunocompromised host. Most previous reports of central nervous system infection due to MAC have been meningoencephalitis in patients infected with human immunodeficiency virus (HIV). Only four cases of brain abscess due to MAC have been reported worldwide. We report a case of brain abscess due to MAC in a non-HIV patient. Although drugs used for treatment of MAC have limited central nervous penetration, an azithromycin-based anti-tuberculous therapy after surgical drainage of the abscess showed improvement. To the best of our knowledge, this is the first reported case of MAC brain abscess in the Korean literature.
MeSH Terms
Figure
Reference
-
1. Koh WJ, Kwon OJ. Diagnosis and treatment of nontuberculous mycobacterial lung disease. Korean J Med. 2008. 74:120–131.
Article2. Uldry PA, Bogousslavsky J, Regli F, Chave JP, Beer V. Chronic Mycobacterium avium complex infection of the central nervous system in a nonimmunosuppressed woman. Eur Neurol. 1992. 32:285–288.
Article3. Murray R, Mallal S, Heath C, French M. Cerebral mycobacterium avium infection in an HIV-infected patient following immune reconstitution and cessation of therapy for disseminated mycobacterium avium complex infection. Eur J Clin Microbiol Infect Dis. 2001. 20:199–201.
Article4. Berger P, Lepidi H, Drogoul-Vey MP, Poizot-Martin I, Drancourt M. Mycobacterium avium brain abscess at the initiation of highly active antiretroviral therapy. Eur J Clin Microbiol Infect Dis. 2004. 23:142–144.
Article5. Fortin C, Rouleau D. Cerebral Mycobacterium avium abscesses: Late immune reconstitution syndrome in an HIV-1-infected patient receiving highly active antiretroviral therapy. Can J Infect Dis Med Microbiol. 2005. 16:187–189.
Article6. Medical Section of the American Lung Association. Diagnosis and treatment of disease caused by nontuberculous mycobacteria. This official statement of the American Thoracic Society was approved by the Board of Directors, March 1997. Am J Respir Crit Care Med. 1997. 156:S1–S25.7. Gray F, Geny C, Lionnet F, Dournon E, Fenelon G, Gherardi R, Poirier J. Neuropathologic study of 135 adult cases of acquired immunodeficiency syndrome (AIDS). Ann Pathol. 1991. 11:236–247.8. Gray F, Gherardi R, Keohane C, Favolini M, Sobel A, Poirier J. Pathology of the central nervous system in 40 cases of acquired immune deficiency syndrome (AIDS). Neuropathol Appl Neurobiol. 1988. 14:365–380.
Article9. Cegielski JP, Wallace RJ Jr. Central nervous system infections with nontuberculous mycobacteria. Clin Infect Dis. 1997. 25:1496–1497.
Article10. Mathisen GE, Johnson JP. Brain abscess. Clin Infect Dis. 1997. 25:763–779. quiz 780-1.
Article11. Cárdenas G, Soto-Hernández JL, Orozco RV, Silva EG, Revuelta R, Amador JL. Tuberculous brain abscesses in immunocompetent patients: management and outcome. Neurosurgery. 2010. 67:1081–1087.
Article12. Katti MK. Pathogenesis, diagnosis, treatment, and outcome aspects of cerebral tuberculosis. Med Sci Monit. 2004. 10:RA215–RA229.13. Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, Holland SM, Horsburgh R, Huitt G, Iademarco MF, Iseman M, Olivier K, Ruoss S, von Reyn CF, Wallace RJ Jr, Winthrop K. ATS Mycobacterial Diseases Subcommittee. American Thoracic Society. Infectious Disease Society of America. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007. 175:367–416.
Article14. Benson CA, Williams PL, Currier JS, Holland F, Mahon LF, MacGregor RR, Inderlied CB, Flexner C, Neidig J, Chaisson R, Notario GF, Hafner R. AIDS Clinical Trials Group 223 Protocol Team. A prospective, randomized trial examining the efficacy and safety of clarithromycin in combination with ethambutol, rifabutin, or both for the treatment of disseminated Mycobacterium avium complex disease in persons with acquired immunodeficiency syndrome. Clin Infect Dis. 2003. 37:1234–1243.
Article15. Dubé MP, Sattler FR, Torriani FJ, See D, Havlir DV, Kemper CA, Dezfuli MG, Bozzette SA, Bartok AE, Leedom JM, Tilles JG, McCutchan JA. California Collaborative Treatment Group. A randomized evaluation of ethambutol for prevention of relapse and drug resistance during treatment of Mycobacterium avium complex bacteremia with clarithromycin-based combination therapy. J Infect Dis. 1997. 176:1225–1232.
Article16. Nau R, Sörgel F, Eiffert H. Penetration of drugs through the blood-cerebrospinal fluid/blood-brain barrier for treatment of central nervous system infections. Clin Microbiol Rev. 2010. 23:858–883.
Article17. Prasad KN, Mishra AM, Gupta D, Husain N, Husain M, Gupta RK. Analysis of microbial etiology and mortality in patients with brain abscess. J Infect. 2006. 53:221–227.
Article18. Gupta RK, Vatsal DK, Husain N, Chawla S, Prasad KN, Roy R, Kumar R, Jha D, Husain M. Differentiation of tuberculous from pyogenic brain abscesses with in vivo proton MR spectroscopy and magnetization transfer MR imaging. AJNR Am J Neuroradiol. 2001. 22:1503–1509.19. Chakraborti S, Mahadevan A, Govindan A, Nagarathna S, Santosh V, Yasha TC, Devi BI, Chandramouli BA, Kovoor JM, Chandramuki A, Shankar SK. Clinicopathological study of tuberculous brain abscess. Pathol Res Pract. 2009. 205:815–822.
Article20. Lu CH, Chang WN, Lin YC, Tsai NW, Liliang PC, Su TM, Rau CS, Tsai YD, Liang CL, Chang CJ, Lee PY, Chang HW, Wu JJ. Bacterial brain abscess: microbiological features, epidemiological trends and therapeutic outcomes. QJM. 2002. 95:501–509.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spondylitis with an Epidural Abscess due to Mycobacterium fortuitum: A Case Report
- Mycobacterium fortuitum Infection Caused by a Nerve Block
- A Case of Vertebral Osteomyelitis With Epidural Abscess Caused by Mycobacterium intracellulare in a Rheumatoid Arthritis Patient
- A Case of Skin Infection Caused by Mycobacterium abscessus
- Retroperitoneal Abscess by Citrobacter and Klebsiella in a Renal Transpant Recipient