Neurointervention.
2015 Feb;10(1):34-38. 10.5469/neuroint.2015.10.1.34.
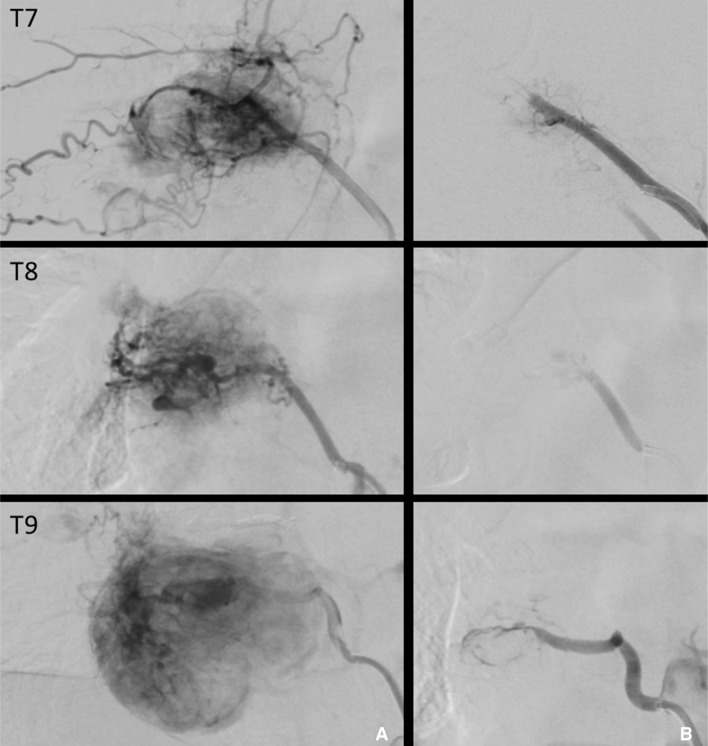
Trans-arterial Onyx Embolization of a Functional Thoracic Paraganglioma
- Affiliations
-
- 1Center of Excellence in Neurosciences, Texas Tech University Health Sciences Center, Paul L. Foster School of Medicine, EL Paso, TX, USA.
- 2Department of Neurology, Texas Tech University Health Sciences Center, Paul L, Foster School of Medicine, EL Paso, TX, USA. gustavo.j.rodriguez@ttuhsc.edu
- 3Department of Radiology, Texas Tech University Health Sciences Center, Paul L, Foster School of Medicine, EL Paso, TX, USA.
- 4Department of Pathology, Texas Tech University Health Sciences Center, Paul L, Foster School of Medicine, EL Paso, TX, USA.
- 5Department of Pediatric Surgery, Texas Tech University Health Sciences Center, Paul L, Foster School of Medicine, EL Paso, TX, USA.
- 6Department of Neurosurgery, University Medical Center, EL Paso, TX, USA.
- KMID: 1910758
- DOI: http://doi.org/10.5469/neuroint.2015.10.1.34
Abstract
- Paragangliomas are rare tumors of the endocrine system. They are highly vascular and in some cases hormonally active, making their management challenging. Although there is strong evidence of the safety and effectiveness of preoperative embolization in the management of spinal tumors, only five cases have been reported in the setting of thoracic paragangliomas. We present the case of a 19-year-old man with a large, primary, functional, malignant paraganglioma of the thoracic spine causing a vertebral fracture and spinal cord compression. To our knowledge this is the first report of preoperative trans-arterial balloon augmented Onyx embolization of a thoracic paraganglioma.
Keyword
Figure
Reference
-
1. Laird AM, Gauger PG, Doherty GM, Miller BS. Paraganglioma: not just an extra-adrenal pheochromocytoma. Langenbecks Arch Surg. 2012; 397:247–253. PMID: 22086065.
Article2. Ilias I, Pacak K. A clinical overview of pheochromocytomas/paragangliomas and carcinoid tumors. Nucl Med Biol. 2008; 35(Suppl 1):S27–S34. PMID: 18707631.
Article3. Brodkey JA, Brodkey JS, Watridge CB. Metastatic paraganglioma causing spinal cord compression. Spine. 1995; 20:367–372. PMID: 7732475.
Article4. Cybulski GR, Nijensohn E, Brody BA, Meyer PR Jr, Cohen B. Spinal cord compression from a thoracic paraganglioma: case report. Neurosurgery. 1991; 28:306–309. PMID: 1997903.
Article5. Kwan RB, Erasmus AM, Hunn AW, Dubey A, Waites P, Jessup PJ, et al. Pre-operative embolisation of metastatic paraganglioma of the thoracic spine. J Clin Neurosci. 2010; 17:394–396. PMID: 20074965.
Article6. Noorda RJ, Wuisman PI, Kummer AJ, Winters HA, Rauwerda JA, Egeler-Peerdeman SM. Nonfunctioning malignant paraganglioma of the posterior mediastinum with spinal cord compression. A case report. Spine. 1996; 21:1703–1709. PMID: 8839476.7. Shin JY, Lee SM, Hwang MY, Sohn CH, Suh SJ. MR findings of the spinal paraganglioma : report of three cases. J Korean Med Sci. 2001; 16:522–526. PMID: 11511803.8. Ghobrial GM, Chalouhi N, Harrop J, Dalyai RT, Tjoumakaris S, Gonzalez LF, et al. Preoperative spinal tumor embolization: an institutional experience with Onyx. Clin Neurol Neurosurg. 2013; 115:2457–2463. PMID: 24169150.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hairball-Like Migration of “Onyx Threads” into the Draining Vein during Transarterial Embolization of a Dural Arteriovenous Fistula: A Case Report and Experimental Validation
- Complication Associated with Onyx Embolization of Spinal Cord Arteriovenous Malformation
- Intra-arterial Onyx Embolization of Vertebral Body Lesions
- Transvenous Onyx embolization of cavernous sinus dural arteriovenous fistula using a balloon catheter in the arterial side for flow control
- Cranial Nerve Palsy after Onyx Embolization as a Treatment for Cerebral Vascular Malformation