Anat Cell Biol.
2014 Sep;47(3):157-161. 10.5115/acb.2014.47.3.157.
Distribution and length of osteophytes in the lumbar vertebrae and risk of rupture of abdominal aortic aneurysms: a study of dry bones from Chiang Mai, Thailand
- Affiliations
-
- 1Department of Basic Science, Faculty of Science, Payap University, Chiang Mai, Thailand.
- 2Department of Anatomy, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand. pasuk034@gmail.com
- KMID: 1882590
- DOI: http://doi.org/10.5115/acb.2014.47.3.157
Abstract
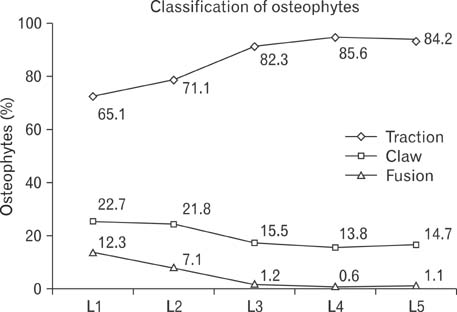
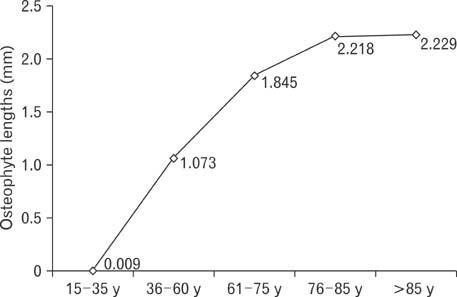
- Vertebral osteophytes are a characteristic feature of intervertebral disc degeneration. In the lumbar spinal region, the two major structures in close proximity anterior to the spine are the inferior vena cava and the abdominal aorta, both of which have been reported to be affected by osteophytes. The purpose of this study was to determine the distribution, classification and lengths of osteophytes in the lumbar vertebrae. One hundred and eighty lumbar columns of 90 males and 90 females from Chiang Mai, Thailand, in the age range 15 to 96 years (mean age, 63 years) were collected. The measuring length of osteophytes was assessed on vertebral body and articular facet. Statistical analysis was performed by descriptive analysis, chi-square and Pearson Correlation. Lumbar osteophytes were presented in 175 specimens (97.2%), 88 males and 87 females. The highest frequency was at L4, most were on the superior, inferior surface of body and articular facet (39.7%, 38.4%, and 22%), respectively. The greatest mean length was 3.47+/-2.21 mm at L5, and the longest length of anterior superior surface of body was 28.56 mm. The osteophyte length was significantly correlated directly with age (P<0.01), and males were significantly greater than females (P<0.05). The highest prevalence of osteophytes was on the anterior side of superior surface of body (30.4%), and the classification was traction. It can be proposed that the abdominal aorta could be damaged, especially a risk of rupture of abdominal aortic aneurysm.
Keyword
MeSH Terms
Figure
Reference
-
1. Dregelid E, Jenssen G, Jonung T, Braaten A. Pseudoaneurysm of the abdominal aorta due to a needle-like osteophyte on the first lumbar vertebra. J Vasc Surg. 2007; 45:1059–1061.2. Karasik D, Kiel DP, Kiely DK, Cupples LA, Wilson PW, O'Donnell CJ, Felson DT. Abdominal aortic calcification and exostoses at the hand and lumbar spine: the Framingham Study. Calcif Tissue Int. 2006; 78:1–8.3. Witteman JC, Kok FJ, van Saase JL, Valkenburg HA. Aortic calcification as a predictor of cardiovascular mortality. Lancet. 1986; 2:1120–1122.4. Iribarren C, Sidney S, Sternfeld B, Browner WS. Calcification of the aortic arch: risk factors and association with coronary heart disease, stroke, and peripheral vascular disease. JAMA. 2000; 283:2810–2815.5. Macnab I. The traction spur. An indicator of segmental instability. J Bone Joint Surg Am. 1971; 53:663–670.6. Pye SR, Reid DM, Lunt M, Adams JE, Silman AJ, O'Neill TW. Lumbar disc degeneration: association between osteophytes, end-plate sclerosis and disc space narrowing. Ann Rheum Dis. 2007; 66:330–333.7. O'Neill TW, McCloskey EV, Kanis JA, Bhalla AK, Reeve J, Reid DM, Todd C, Woolf AD, Silman AJ. The distribution, determinants, and clinical correlates of vertebral osteophytosis: a population based survey. J Rheumatol. 1999; 26:842–848.8. Rothschild BM. Lumbar spondylosis: epidemiology [Internet]. New York: Medscape;2011. cited 2012 Sep 14. Available from: http://emedicine.medscape.com/article/249036-overview#a0199.9. Klaassen Z, Tubbs RS, Apaydin N, Hage R, Jordan R, Loukas M. Vertebral spinal osteophytes. Anat Sci Int. 2011; 86:1–9.10. Panjabi M, Brown M, Lindahl S, Irstam L, Hermens M. Intrinsic disc pressure as a measure of integrity of the lumbar spine. Spine (Phila Pa 1976). 1988; 13:913–917.11. Heuer F, Schmidt H, Wilke HJ. The relation between intervertebral disc bulging and annular fiber associated strains for simple and complex loading. J Biomech. 2008; 41:1086–1094.12. McGill S. Low back disorders: evidence-based prevention and rehabilitation. 2nd ed. Champaign: Human Kinetics;2007. p. 73.13. Harthun NL, Cheanvechai V, Graham LM, Freischlag JA, Gahtan V. Prevalence of abdominal aortic aneurysm and repair outcomes on the basis of patient sex: Should the timing of intervention be the same? J Thorac Cardiovasc Surg. 2004; 127:325–328.14. Bridges PS. Vertebral arthritis and physical activities in the prehistoric southeastern United States. Am J Phys Anthropol. 1994; 93:83–93.15. Yamada Y, Okuizumi H, Miyauchi A, Takagi Y, Ikeda K, Harada A. Association of transforming growth factor beta1 genotype with spinal osteophytosis in Japanese women. Arthritis Rheum. 2000; 43:452–460.16. Kramer PA, Newell-Morris LL, Simkin PA. Spinal degenerative disk disease (DDD) in female macaque monkeys: epidemiology and comparison with women. J Orthop Res. 2002; 20:399–408.17. Yoshimura N, Dennison E, Wilman C, Hashimoto T, Cooper C. Epidemiology of chronic disc degeneration and osteoarthritis of the lumbar spine in Britain and Japan: a comparative study. J Rheumatol. 2000; 27:429–433.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The characteristics of osteophyte around lumbar vertebral foramina associated with spinal stenosis
- Age estimation equations using vertebral osteophyte formation in a Thai population: comparison and modified osteophyte scoring method
- Morphology of the human aorta and age-related changes: anatomical facts
- The estimation of age from elastic fibers in the tunica media of the aortic wall in a thai population: a preliminary study using aorta image analysis
- Stature estimation using the sternum in a Thai population