Anat Cell Biol.
2019 Jun;52(2):143-148. 10.5115/acb.2019.52.2.143.
The characteristics of osteophyte around lumbar vertebral foramina associated with spinal stenosis
- Affiliations
-
- 1Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand.
- 2Department of Anatomy, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand. pasuk034@gmail.com
- 3Forensic Osteology Research Center, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand.
- 4Excellence Center in Osteology Research and Training Center (ORTC), Chiang Mai University, Chiang Mai, Thailand.
- KMID: 2451218
- DOI: http://doi.org/10.5115/acb.2019.52.2.143
Abstract
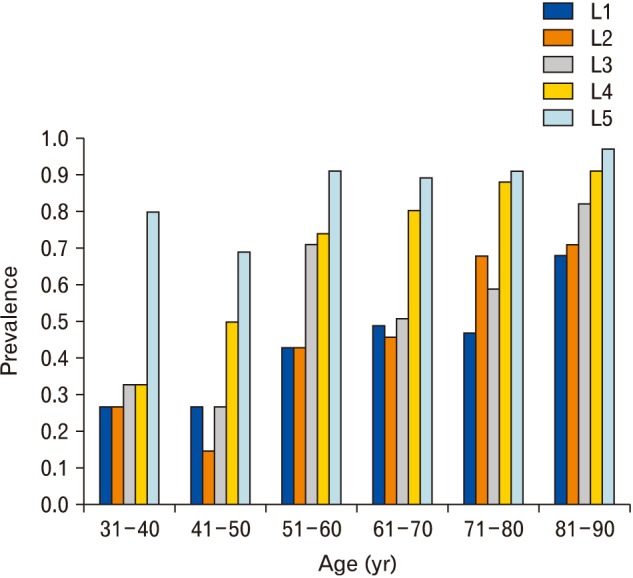
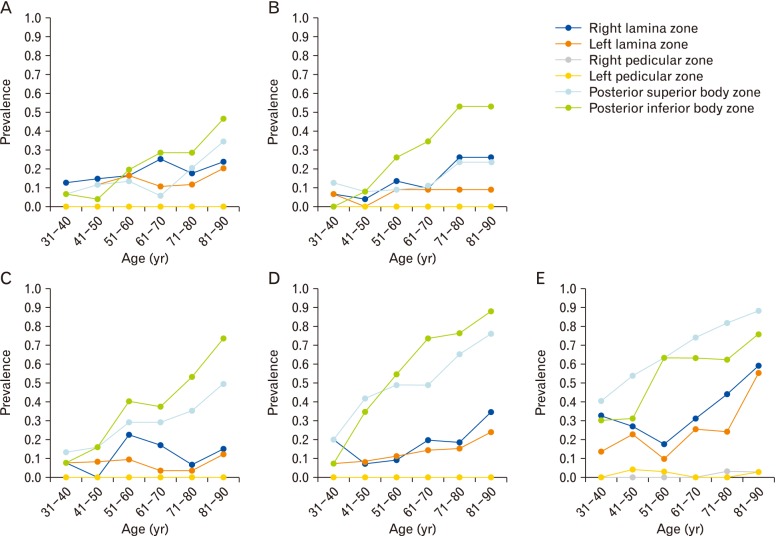
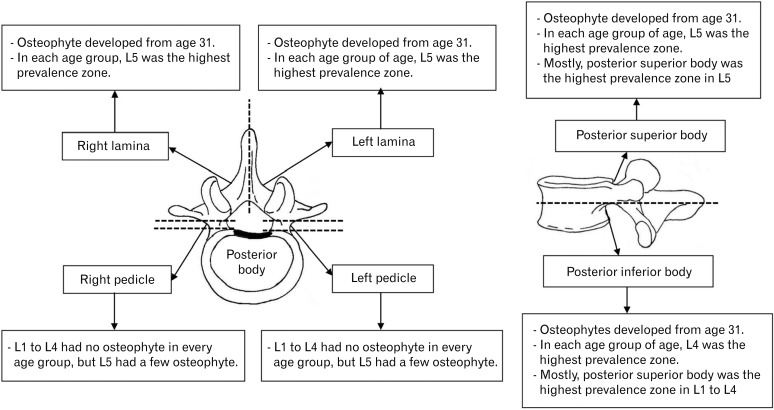
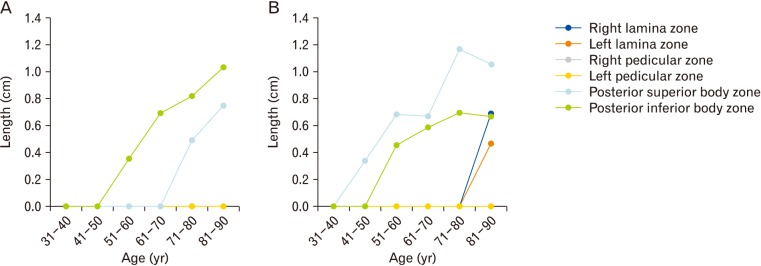
- Spinal stenosis most commonly occurs on lumbar vertebrae because of degenerative changes. This research studied the characteristics of osteophyte development in lumbar vertebrae foramina and association of osteophyte development with lumbar spinal stenosis. The total number of all levels of lumbar spines of subjects was 179 from 31 to 90 years of age. The vertebral foramen was divided into six zones. The prevalence and measurements of the length of osteophytes in the vertebral foramina were obtained. The prevalence and length of osteophytes in the posterior body zone were higher than the laminal zone, and higher than the pedicular zone, respectively. In each zone, the highest prevalence of osteophytes was at L5, except for the inferior posterior body zone that the highest prevalence is at L4. The length of osteophyte was also in same direction as the prevalence. The prevalence of osteophytes among six zones of each level were compared, and found, in L1 to L4, the inferior posterior body zone generally had the highest prevalence, except in L5, the superior posterior body zone had the highest prevalence. Moreover, prevalence, as well as length, of osteophytes in lumbar vertebral foramina, of all levels, was positively associated with age. Vertebral osteophytes can develop beginning at 31 years of age. In conclusion, posterior body of L4 and L5 had the highest prevalence of osteophyte formation, thus, these area had the highest probability to cause spinal stenosis.
Keyword
Figure
Reference
-
1. Lamer TJ. Lumbar spine pain originating from vertebral osteophytes. Reg Anesth Pain Med. 1999; 24:347–351. PMID: 10445775.2. Namking M, Buranaurgsa M, Jeeravipoolvarn P, Deesart M. The prevalence of vertebral osteophyte formation in Northeast Thais. Srinagarind Med J. 2008; 23:81–92.3. Klaassen Z, Tubbs RS, Apaydin N, Hage R, Jordan R, Loukas M. Vertebral spinal osteophytes. Anat Sci Int. 2011; 86:1–9. PMID: 20383671.4. Goode AP, Carey TS, Jordan JM. Low back pain and lumbar spine osteoarthritis: how are they related? Curr Rheumatol Rep. 2013; 15:305. PMID: 23307577.5. Zukowski LA, Falsetti AB, Tillman MD. The influence of sex, age and BMI on the degeneration of the lumbar spine. J Anat. 2012; 220:57–66. PMID: 22050626.6. O'Neill TW, McCloskey EV, Kanis JA, Bhalla AK, Reeve J, Reid DM, Todd C, Woolf AD, Silman AJ. The distribution, determinants, and clinical correlates of vertebral osteophytosis: a population based survey. J Rheumatol. 1999; 26:842–848. PMID: 10229405.7. Chanapa P. Relationship between Thai working lifestyles and lumbar osteophyte. Songkla Med J. 2016; 34:201–209.8. Chanapa P, Yoshiyuki T, Mahakkanukrauh P. Distribution and length of osteophytes in the lumbar vertebrae and risk of rupture of abdominal aortic aneurysms: a study of dry bones from Chiang Mai, Thailand. Anat Cell Biol. 2014; 47:157–161. PMID: 25276474.9. Griffith JF, Huang J, Law SW, Xiao F, Leung JC, Wang D, Shi L. Population reference range for developmental lumbar spinal canal size. Quant Imaging Med Surg. 2016; 6:671–679. PMID: 28090445.10. Genevay S, Atlas SJ. Lumbar spinal stenosis. Best Pract Res Clin Rheumatol. 2010; 24:253–265. PMID: 20227646.11. Adams MA, Bogduk N, Burton K, Dolan P. The biomechanics of back pain. Edinburgh: Elsevier Science;2002.12. Sokolove J, Lepus CM. Role of inflammation in the pathogenesis of osteoarthritis: latest findings and interpretations. Ther Adv Musculoskelet Dis. 2013; 5:77–94. PMID: 23641259.13. Williams SK. Thoracic and lumbar spinal injuries. In : Herkowitz HN, Garfin SR, Eismont FJ, Bell GR, Balderston RA, editors. Rothman-Simeone the Spine. 6th ed. Philadelphia, PA: Elsevier Saunders;2011. p. 1132–1156.14. Boos N, Aebi M. Spinal disorders: fundamentals of diagnosis and treatment. Berlin: Springer;2008.15. Kim DK, Kim MJ, Kim YS, Oh CS, Shin DH. Vertebral osteophyte of pre-modern Korean skeletons from Joseon tombs. Anat Cell Biol. 2012; 45:274–281. PMID: 23301195.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Coexisting Cervical and Lumbar Spinal Stenosis
- Lumbar Spinal Stenosis in Vertebral Ankylosing Hyperostosis: A Case Report
- A Clinical Observation on High Lumbar Disc Herniation
- Diagnostic Significance of Myelo-Enhanced Computerized Tomography(MECT) in Spinal Stenosis
- Y-Angle Stenosis of Lumbar Spine: New Concept of Lumbar Stenosis