Lab Med Online.
2013 Jan;3(1):34-39. 10.3343/lmo.2013.3.1.34.
Epidemiology and Resistance Patterns of Bacterial Pathogens in Urinary Tract Infections in the Northern Gyeonggi-do Area during 2007-2011
- Affiliations
-
- 1Department of Laboratory Medicine, Kwandong University College of Medicine, Goyang, Korea. hmlee.labmed@gmail.com
- KMID: 1845394
- DOI: http://doi.org/10.3343/lmo.2013.3.1.34
Abstract
- BACKGROUND
Bacteria that cause urinary tract infections (UTIs) are found with different frequencies in different regions; moreover, antibiotic susceptibility can also vary by region. We retrospectively studied and compared the species and antimicrobial susceptibility of bacterial pathogens isolated from patients with UTIs in the northern Gyeonggi-do area.
METHODS
We analyzed urine specimens collected from patients who visited the Myongji Hospital between 2007 and 2011. The urine specimens were cultured, and bacteria were identified by biochemical examination with an API kit (bioMerieux Inc., USA). Antimicrobial susceptibility was determined by the disc diffusion method and the Vitek II system (bioMerieux Inc., USA).
RESULTS
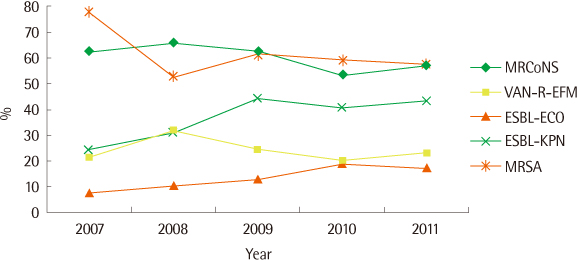
A total of 11,818 (31.4%) urine specimens were culture positive. The most common species identified were Escherichia coli (37.1%), Klebsiella pneumoniae (7.4%), Enterococcus faecium (6.1%), and Candida spp. (5.5%). The proportion of isolates producing extended-spectrum beta-lactamases significantly increased during the study period.
CONCLUSIONS
E. coli, K. pneumoniae, and E. faecium were the 3 most common organisms identified. Of note, however, was the increasing frequency of Pseudomonas spp. and Proteus spp. isolated during the more recent years. Further studies are required from other centers in the northern Gyeonggi-do area.
MeSH Terms
Figure
Cited by 1 articles
-
Profiles of Yeast Isolated from Urinary Tracts with and without Catheter during 2011-2013
Jae Hyung Ryu, Tae-Hyoung Kim, Oh Joo Kweon, Mi-Kyung Lee
Korean J Urogenit Tract Infect Inflamm. 2014;9(2):93-98. doi: 10.14777/kjutii.2014.9.2.93.
Reference
-
1. Kim YR, Huh JS, Kang SH. Patterns of antimicrobial susceptibility of the causative bacteria of urinary tract Infections in recent years in an island region. Korean J Clin Microbiol. 2007. 10:19–24.2. Shin JH, Kim HR, Lee HR, Chung JI, Min K, Moon CS, et al. Etiology and antimicrobial susceptibility of bacterial pathogens causing community-acquired urinary tract infection at a tertiary-care hospital. Korean J Clin Microbiol. 2005. 8:142–147.3. Kim HY, Yim SH, Cho HJ, Kim JS, Ha US, Kim DB, et al. Changes in causative organisms and antibiotic sensitivity in intensive care unit-acquired urinary tract infection. Korean J Urol. 2009. 50:1108–1113.
Article4. Yu SM, Park KY. Risk factors for nosocomial urinary tract infection in the intensive care unit with a positive urine culture and foley catheterization. J Korean Acad Nurs. 2007. 37:1149–1158.
Article5. Foxman B. Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Am J Med. 2002. 113:Suppl 1A. S5–S13.
Article6. Lizioli A, Privitera G, Alliata E, Antonietta Banfi EM, Boselli L, Panceri ML, et al. Prevalence of nosocomial infections in Italy: result from the Lombardy survey in 2000. J Hosp Infect. 2003. 54:141–148.
Article7. Eriksen HM, Iversen BG, Aavitsland P. Prevalence of nosocomial infections in hospitals in Norway, 2002 and 2003. J Hosp Infect. 2005. 60:40–45.
Article8. Murray PR, editor. Manual of clinical microbiology. 2007. 9th ed. Washington: ASM Press;323–324.9. Jeong YS, Lee KW, et al. Diagnostic microbiology. 2009. 4th ed. Seoul: Seoheung Publish;102–105.10. Ferry S, Burman LG, Mattsson B. Urinary tract infection in primary health care in northern Sweden. I. Epidemiology. Scand J Prim Health Care. 1987. 5:123–128.
Article11. Ko HS, Choi DY, Han YT. A study of the changes of anitibiotic sensitivity to the causative organisms of urinary tract infection for recent 5 years. Korean J Urol. 1999. 40:809–816.12. Alvarez-Lerma F, Nolla-Salas J, León C, Palomar M, Jordá R, Carrasco N, et al. Candiduria in critically ill patients admitted to intensive care medical units. Intensive Care Med. 2003. 29:1069–1076.
Article13. Richards MJ, Edwards JR, Culver DH, Gaynes RP. Nosocomial infections in combined medical-surgical intensive care units in the United States. Infect Control Hosp Epidemiol. 2000. 21:510–515.
Article14. Mathai D, Jones RN, Pfallera MA. Epidemiology and frequency of resistance among pathogens causing urinary tract infections in 1,510 hospitalized patients: A report from the SENTRY Antimicrobial Aurveillance Program (North America). Diagn Microbiol Infect Dis. 2001. 40:129–136.
Article15. Ryu KH, Kim MK, Jeong YB. A recent study on the antimicrobial sensitivity of the organisms that cause urinary tract infection. Korean J Urol. 2007. 48:638–645.
Article16. Warren JW, Abrutyn E, Hebel JR, Johnson JR, Schaeffer AJ, Stamm WE. Guidelines for antimicrobial treatment of uncomplicated acute bacterial cystitis and acute pyelonephritis in women. Infectious Diseases Society of America (IDSA). Clin Infect Dis. 1999. 29:745–758.
Article17. The Korean Society of Infectious Diseases. The Korean Society for Chemotherapy. Korean Association of Urogenital Tract Infection and Inflammation. The Korean Society of Clinical Microbiology. Clinical guideline for the diagnosis and treatment of urinary tract infections: asymptomatic bacteriuria, uncomplicated & complicated urinary tract infections, bacterial prostatitis. Infect Chemother. 2011. 43:1–25.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Guideline for the Diagnosis and Treatment of Urinary Tract Infections: Asymptomatic Bacteriuria, Uncomplicated & Complicated Urinary Tract Infections, Bacterial Prostatitis
- Treatment of Community-Acquired Uncomplicated Urinary Tract Infection
- Therapeutic strategy for the management of multidrug-resistant gram-negative bacterial infections
- Clinical Importance and Epidemiology of Quinolone Resistance
- Patterns of Antimicrobial Susceptibility of the Causative Bacteria of Urinary Tract Infections in Recent Years in an Island Region