Korean J Urol.
2013 Aug;54(8):541-546. 10.4111/kju.2013.54.8.541.
Laparoendoscopic Single-Site Urologic Surgery in Children Less Than 5 Years of Age
- Affiliations
-
- 1Department of Urology, Muljibhai Patel Urological Hospital, Gujarat, India. mrdesai@mpuh.org
- KMID: 1840468
- DOI: http://doi.org/10.4111/kju.2013.54.8.541
Abstract
- PURPOSE
We report our experience with laparoendoscopic single-site (LESS) urological procedures in children less than 5 years of age.
MATERIALS AND METHODS
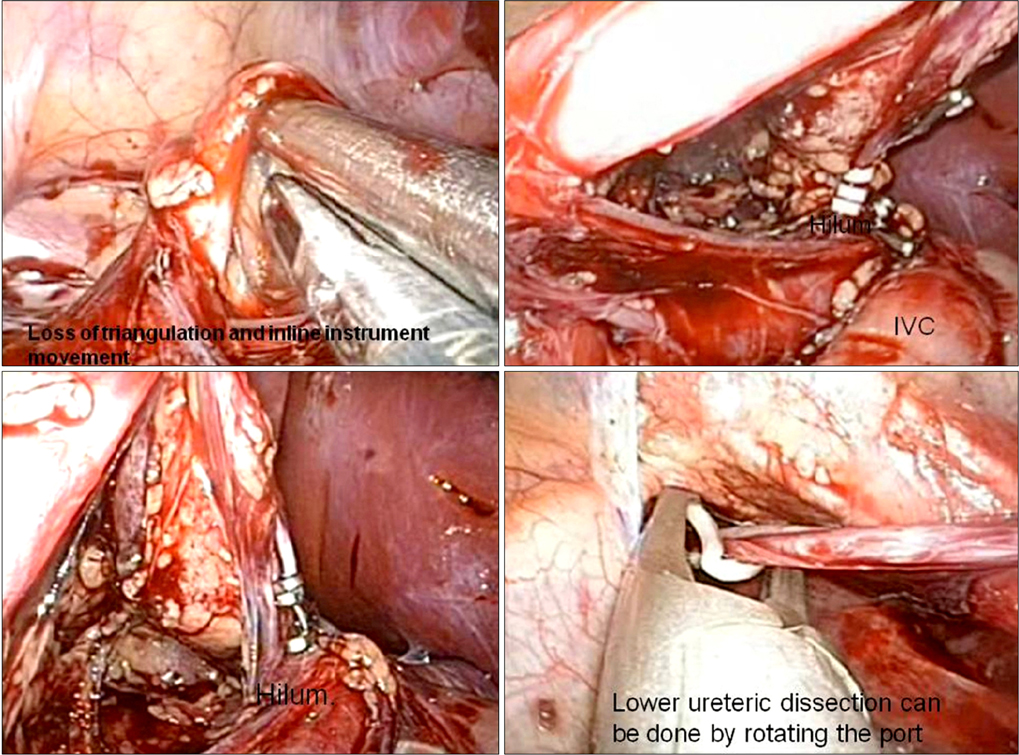
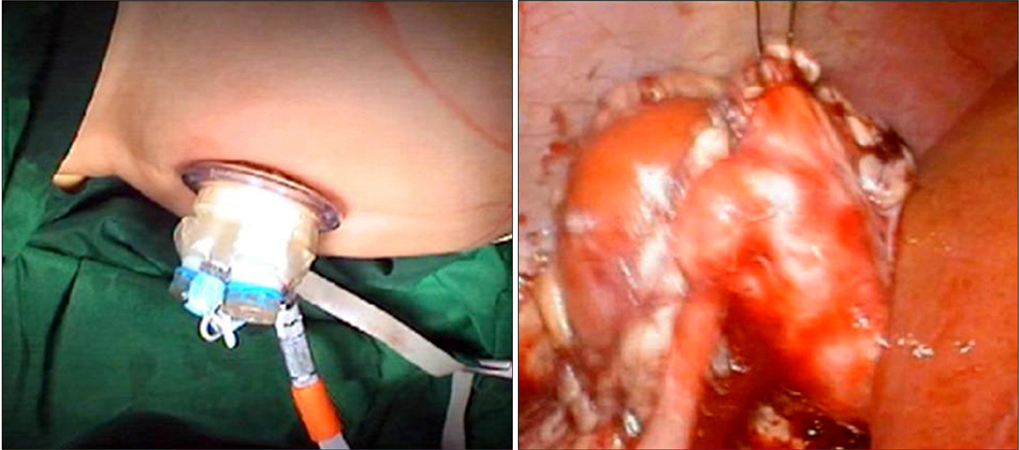
Ten patients (11 procedures) underwent LESS through the umbilicus. Seven patients underwent nephrectomy and three patients underwent pyeloplasty (one simultaneous bilateral). R-port port (Advanced Surgical Concepts, Ireland) was used in nine cases, in one case, the Gelpoint access port (Applied Medical, Rancho Santa Margarita, CA, USA) was used. The Olympus Endoeye camera with coaxial light cable was used. The hilum was secured in all cases with Hem-o-Lok clips (Teleflex Medical, Research Triangle Park, NC, USA) except in one case in which an Endo GIA stapler (Covidien Surgical, Norwalk, CT, USA) was used.
RESULTS
All procedures were technically successful. Accessory port (3 mm) was used in 3 patients. Mean age in nephrectomized patients was 3.14+/-1.7 years, the mean operative room time (ORT) was 97.5+/-12.54 minutes. In the pyeloplasty group, mean ORT was 192+/-47.16 minutes and mean age was 2.43+/-2.3 years. Bilateral pyeloplasty was done in a 4-month-old infant. The ORT in this case was 180 minutes. A follow-up renogram done in the pyeloplasty patients (n=2) showed good drainage. Mean length of stay was 3.6 days (range, 3 to 6 days).The analgesic requirement was 23.86 mg (range, 12.5 to 50 mg) of diclofenac sodium.
CONCLUSIONS
LESS is technically feasible in patients as young as 4 months of age. It has the potential to offer better cosmesis. This needs to be proved in further comparative studies. Development of miniature instruments will further the growth of LESS in this age group.
Keyword
MeSH Terms
Figure
Reference
-
1. Rane A, Rao P, Rao P. Single-port-access nephrectomy and other laparoscopic urologic procedures using a novel laparoscopic port (R-port). Urology. 2008. 72:260–263.2. Hamilton BD, Gatti JM, Cartwright PC, Snow BW. Comparison of laparoscopic versus open nephrectomy in the pediatric population. J Urol. 2000. 163:937–939.3. Raman JD, Bagrodia A, Cadeddu JA. Single-incision, umbilical laparoscopic versus conventional laparoscopic nephrectomy: a comparison of perioperative outcomes and short-term measures of convalescence. Eur Urol. 2009. 55:1198–1204.4. Tugcu V, Ilbey YO, Polat H, Tasci AI. Early experience with laparoendoscopic single-site pyeloplasty in children. J Pediatr Urol. 2011. 7:187–191.5. Piaggio LA, Franc-Guimond J, Noh PH, Wehry M, Figueroa TE, Barthold J, et al. Transperitoneal laparoscopic pyeloplasty for primary repair of ureteropelvic junction obstruction in infants and children: comparison with open surgery. J Urol. 2007. 178(4 Pt 2):1579–1583.6. Broder HL, Smith FB, Strauss RP. Effects of visible and invisible orofacial defects on self-perception and adjustment across developmental eras and gender. Cleft Palate Craniofac J. 1994. 31:429–436.7. Peters CA. Complications in pediatric urological laparoscopy: results of a survey. J Urol. 1996. 155:1070–1073.8. Cost NG, Lee J, Snodgrass WT, Harrison CB, Wilcox DT, Baker LA. Hernia after pediatric urological laparoscopy. J Urol. 2010. 183:1163–1167.9. Koh CJ, De Filippo RE, Chang AY, Hardy BE, Berger A, Eisenberg M, et al. Laparoendoscopic single-site nephrectomy in pediatric patients: initial clinical series of infants to adolescents. Urology. 2010. 76:1457–1461.10. Ponsky TA, Krpata DM. Single-port laparoscopy: considerations in children. J Minim Access Surg. 2011. 7:96–98.11. Cadeddu J, Fernandez R, Desai M, Bergs R, Tracy C, Tang SJ, et al. Novel magnetically guided intra-abdominal camera to facilitate laparoendoscopic single-site surgery: initial human experience. Surg Endosc. 2009. 23:1894–1899.12. National Institutes of Health. Pediatric device consortia grant program (P50). Request for applications (RFA) number: RFA-FD-09-007 [Internet]. c2013. 2013 Feb 26. Bethesda: National Institutes of Health;Available from: http://grants.nih.gov/grants/guide/rfa-files/RFA-FD-09-007.html.13. Singh H, Ganpule A, Malhotra V, Manohar T, Muthu V, Desai M. Transperitoneal laparoscopic pyeloplasty in children. J Endourol. 2007. 21:1461–1466.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hybrid laparoscopic myomectomy: A novel technique
- Laparoendoscopic Single-Site Surgeries: A Single-Center Experience of 171 Consecutive Cases
- Simultaneous Robot-Assisted Laparoendoscopic Single-Site Partial Nephrectomy and Standard Radical Prostatectomy
- Current Status of Laparoendoscopic Single-Site Surgery in Urologic Surgery
- Public perception of "scarless" laparoendoscopic single-site surgery in gynecology