J Cerebrovasc Endovasc Neurosurg.
2012 Sep;14(3):192-202. 10.7461/jcen.2012.14.3.192.
Intracranial Dural Arteriovenous Fistulas: Clinical Characteristics and Management Based on Location and Hemodynamics
- Affiliations
-
- 1Department of Neurosurgery, College of Medicine, Eulji University, Daejeon, Korea. neurocsy@eulji.ac.kr
- 2Department of Neurosurgery, Mayo Clinic, Minnesota, USA.
- KMID: 1808455
- DOI: http://doi.org/10.7461/jcen.2012.14.3.192
Abstract
OBJECTIVE
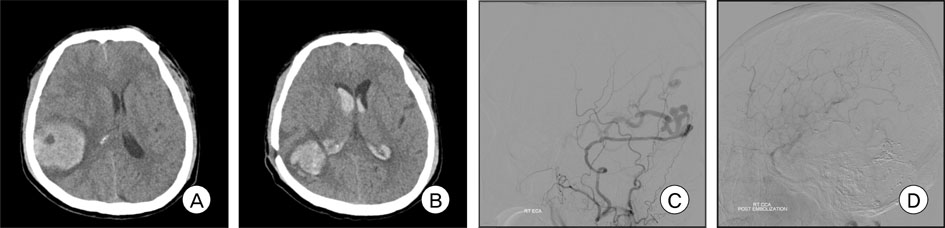
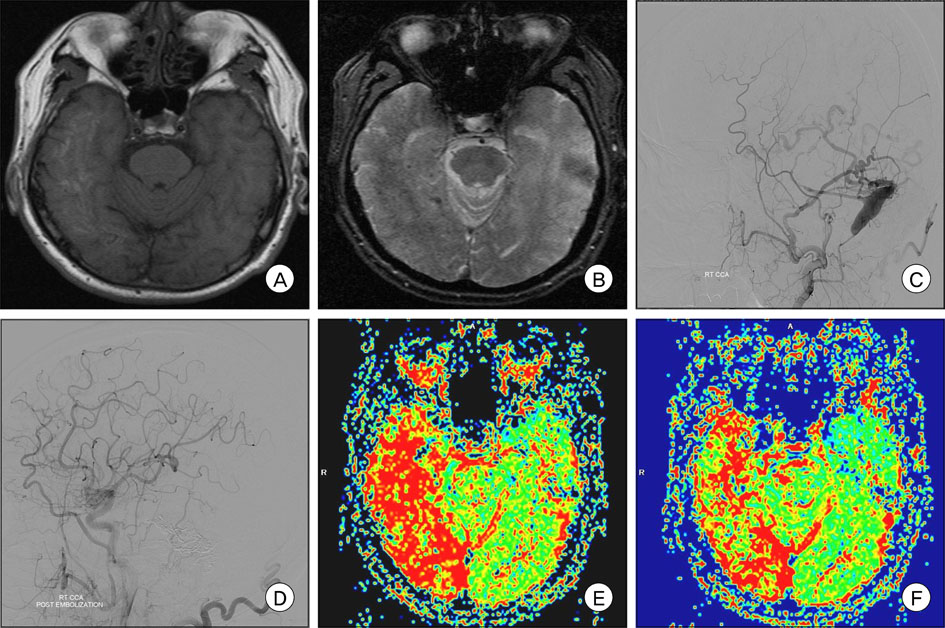
A dural arteriovenous fistula (DAVF) generally refers to a vascular malformation of the wall of a major venous sinus. These lesions have diverse symptoms according to the location and venous drainage, and require multidisciplinary treatment. We report on our experience and analyze the treatment outcome of intracranial DAVFs for a nine-year period.
METHODS
Between January 2000 and December 2008, 95 patients with intracranial DAVFs were enrolled in this study. A retrospective review of clinical records and imaging studies of all patients was conducted. Endovascular embolization, surgical interruption, gamma knife stereotactic radiosurgery (GKS), or combinations of these treatments were performed based on clinical symptoms, lesion location, and venous drainage pattern.
RESULTS
Borden type I, II, and III were 34, 48, and 13 patients, respectively. Aggressive presentation was reported in 6% of Borden type I, 31% of Borden type II, and 77% of Borden type III DAVFs, respectively, and DAVFs involving transverse, sigmoid, and superior sagittal sinus. Overall, the rate of complete obliteration was 68%. The complete occlusion rates with a combination treatment of endovascular embolization and surgery, surgery alone, and endovascular embolization were 89%, 86%, and 80%, respectively. When GKS was used with embolization, the obliteration rate was 83%, although it was only 54% in GKS alone. Spontaneous obliteration of the DAVF occurred in three patients. There were a few complications, including hemiparesis (in microsurgery), intracranial hemorrhage (in endovascular embolization), and facial palsy (in GKS).
CONCLUSION
The hemorrhagic risk of DAVFs is dependent on the location and hemodynamics of the lesions. Strategies for treatment of intracranial DAVFs should be decided according to the characteristic of the DAVFs, based on the location and drainage pattern. GKS can be used as an optional treatment for intracranial DAVFs.
MeSH Terms
Figure
Cited by 1 articles
-
Transcranial Direct Middle Meningeal Artery Puncture for the Onyx Embolization of Dural Arteriovenous Fistula Involving the Superior Sagittal Sinus
Jae-Sang Oh, Seok-Mann Yoon, Jai-Joon Shim, Hack-Gun Bae
J Korean Neurosurg Soc. 2015;57(1):54-57. doi: 10.3340/jkns.2015.57.1.54.
Reference
-
1. Sencer A, Kiris T. Intracranial dural arteriovenous fistulas: A brief review on classification and general features. Turk Neurosurg. 2006. 16(2):57–64.2. Barrow DL, Spector RH, Braun IF, Landman JA, Tindall SC, Tindall GT. Classification and treatment of spontaneous carotid cavernous sinus fistulas. J Neurosurg. 1985. 02. 62(2):248–256.3. Borden JA, Wu JK, Shucart WA. A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg. 1995. 02. 82(2):166–179.
Article4. Brown RD Jr, Wiebers DO, Nichols DA. Intracranial dural arteriovenous fistulae: angiographic predictors of intracranial hemorrhage and clinical outcome in nonsurgical patients. J Neurosurg. 1994. 10. 81(4):531–538.
Article5. Castaigne P. [Rene Djindjian, 1918-1977]. Rev Neurol (Paris). 1977. 12. 133(12):736–738. French.6. Chung SJ, Kim JS, Kim JC, Lee SK, Kwon SU, Lee MC, et al. Intracranial dural arteriovenous fistulas: analysis of 60 patients. Cerebrovasc Dis. 2002. 13(2):79–88.
Article7. Cognard C, Casasco A, Toevi M, Houdart E, Chiras J, Merland JJ. Dural arteriovenous fistulas as a cause of intracranial hypertension due to impairment of cranial venous outflow. J Neurol Neurosurg Psychiatry. 1998. 09. 65(3):308–316.
Article8. Cognard C, Gobin YP, Pierot L, Bailly AL, Houdart E, Casasco A, et al. Cerebral dural arteriovenous fistulas: clinical and angiographic correlation with a revised classification of venous drainage. Radiology. 1995. 03. 194(3):671–680.
Article9. Cognard C, Houdart E, Casasco AE, Jhaveri HS, Chapot R, Merland JJ. Connors JJ, Wojak JC, editors. Endovascular therapy and long term results for intracranial dural arteriovenous fistulae. Interventional Neuroradiology: Strategies and Practical Techniques. 1999. ed 1. Philadelphia: W.B. Saunders Co.;198–214.10. Collice M, D'Aliberti G, Arena O, Solaini C, Fontana RA, Talamonti G, et al. Surgical treatment of intracranial dural arteriovenous fistulae: role of venous drainage. Neurosurgery. 2000. 07. 47(1):56–66. discussion 66-7.
Article11. Gandhi D, Chen J, Pearl M, Huang J, Gemmete JJ, Kathuria S. Intracranial dural arteriovenous fistulas: Classification, imaging findings, and treatment. AJNR Am J Neuroradiol. 2012. 06. 33(6):1007–1013.
Article12. Goto K, Sidipratomo P, Ogata N, Inoue T, Matsuno H. Combining endovascular and neurosurgical treatments of high-risk dural arteriovenous fistulas in the lateral sinus and the confluence of the sinuses. J Neurosurg. 1999. 02. 90(2):289–299.
Article13. Guo WY, Pan DH, Wu HM, Chung WY, Shiau CY, Wang LW, et al. Radiosurgery as a treatment alternative for dural arteriovenous fistulas of the cavernous sinus. AJNR Am J Neuroradiol. 1998. Jun-Jul. 19(6):1081–1087.14. Halbach VV, Higashida RT, Hieshima GB, Mehringer CM, Hardin CW. Transvenous embolization of dural fistulas involving the transverse and sigmoid sinuses. AJNR Am J Neuroradiol. 1989. Mar-Apr. 10(2):385–392.15. Hasumi T, Fukushima T, Haisa T, Yonemitsu T, Waragai M. Focal dural arteriovenous fistula (DAVF) presenting with progressive cognitive impairment including amnesia and alexia. Intern Med. 2007. 46(16):1317–1320.
Article16. Hirono N, Yamadori A, Komiyama M. Dural arteriovenous fistula: A cause of hypoperfusion-induced intellectual impairment. Eur Neurol. 1993. 33(1):5–8.17. Hurst RW, Bagley LJ, Galetta S, Glosser G, Lieberman AP, Trojanowski J, et al. Dementia resulting from dural arteriovenous fistulas: the pathologic findings of venous hypertensive encephalopathy. AJNR Am J Neuroradiol. 1998. 08. 19(7):1267–1273.18. Kakarla UK, Deshmukh VR, Zabramski JM, Albuquerque FC, McDougall CG, Spetzler RF. Surgical treatment of high-risk intracranial dural arteriovenous fistulae: clinical outcomes and avoidance of complications. Neurosurgery. 2007. 09. 61(3):447–457. discussion 457-9.19. Kim MS, Han DH, Kwon OK, Oh CW, Han MH. Clinical characteristics of dural arteriovenous fistula. J Clin Neurosci. 2002. 03. 9(2):147–155.
Article20. Kirsch M, Liebig T, Kuhne D, Henkes H. Endovascular management of dural arteriovenous fistulas of the transverse and sigmoid sinus in 150 patients. Neuroradiology. 2009. 07. 51(7):477–483.
Article21. Kiyosue H, Hori Y, Okahara M, Tanoue S, Sagara Y, Matsumoto S, et al. Treatment of intracranial dural arteriovenous fistulas: current strategies based on location and hemodynamics, and alternative techniques of transcatheter embolization. Radiographics. 2004. Nov-Dec. 24(6):1637–1653.
Article22. Lagares A, Perez-Nunez A, Alday R, Ramos A, Campollo J, Lobato RD. Dural arteriovenous fistula presenting as brainstem ischaemia. Acta Neurochir (Wien). 2007. 149(9):965–967. discussion 967.
Article23. Lalwani AK, Dowd CF, Halbach VV. Grading venous restrictive disease in patients with dural arteriovenous fistulas of the transverse/sigmoid sinus. J Neurosurg. 1993. 07. 79(1):11–15.
Article24. Lasjaunias P, Chiu M, ter Brugge K, Tolia A, Hurth M, Bernstein M. Neurological manifestations of intracranial dural arteriovenous malformations. J Neurosurg. 1986. 05. 64(5):724–730.
Article25. Lawton MT, Chun J, Wilson CB, Halbach VV. Ethmoidal dural arteriovenous fistulae: an assessment of surgical and endovascular management. Neurosurgery. 1999. 10. 45(4):805–810. discussion 810-1.
Article26. Lee PH, Lee JS, Shin DH, Kim BM, Huh K. Parkinsonism as an initial manifestation of dural arteriovenous fistula. Eur J Neurol. 2005. 05. 12(5):403–406.
Article27. Lewis AI, Tomsick TA, Tew JM Jr. Management of tentorial dural arteriovenous malformations: transarterial embolization combined with stereotactic radiation or surgery. J Neurosurg. 1994. 12. 81(6):851–859.
Article28. Lucas Cde P, Zabramski JM. Dural arteriovenous fistula of the transverse-sigmoid sinus causing trigeminal neuralgia. Acta Neurochir (Wien). 2007. 12. 149(12):1249–1253. discussion 1253.
Article29. Lucas CP, Zabramski JM, Spetzler RF, Jacobowitz R. Treatment for intracranial dural arteriovenous malformations: a meta-analysis from the English language literature. Neurosurgery. 1997. 06. 40(6):1119–1130. discussion 1130-2.
Article30. Luciani A, Houdart E, Mounayer C, Saint Maurice JP, Merland JJ. Spontaneous closure of dural arteriovenous fistulas: report of three cases and review of the literature. AJNR Am J Neuroradiol. 2001. 05. 22(5):992–996.31. Pan DH, Chung WY, Guo WY, Wu HM, Liu KD, Shiau CY, et al. Stereotactic radiosurgery for the treatment of dural arteriovenous fistulas involving the transverse-sigmoid sinus. J Neurosurg. 2002. 05. 96(5):823–829.
Article32. Pollock BE, Nichols DA, Garrity JA, Gorman DA, Stafford SL. Stereotactic radiosurgery and particulate embolization for cavernous sinus dural arteriovenous fistulae. Neurosurgery. 1999. 09. 45(3):459–466. discussion 466-7.
Article33. Roy D, Raymond J. The role of transvenous embolization in the treatment of intracranial dural arteriovenous fistulas. Neurosurgery. 1997. 06. 40(6):1133–1141. discussion 1141-4.
Article34. Sasaki H, Nukui H, Kaneko M, Mitsuka S, Hosaka T, Kakizawa T, et al. Long-term observations in cases with spontaneous carotid cavernous fistulas. Acta Neurochir (Wien). 1988. 90(3-4):117–120.35. Suh DC, Lee JH, Kim SJ, Chung SJ, Choi CG, Kim HJ, et al. New concept in cavernous sinus dural arteriovenous fistula: correlation with presenting symptom and venous drainage patterns. Stroke. 2005. 06. 36(6):1134–1139.36. Sung KH, Min KS, Lee MS, Kim YG, Kim DH. Treatment modalities for dural arteriovenous fistulas (DAVFs) according to venous drainage patterns. Korean J Cerebrovasc Surg. 2008. 06. 10(2):364–373.37. Ushikoshi S, Houkin K, Kuroda S, Asano T, Iwasaki Y, Miyasaka K, et al. Surgical treatment of intracranial dural arteriovenous fistulas. Surg Neurol. 2002. 04. 57(4):253–261.
Article38. van Dijk JM, terBrugge KG, Willinsky RA, Wallace MC. Clinical course of cranial dural arteriovenous fistulas with long-term persistent cortical venous reflux. Stroke. 2002. 05. 33(5):1233–1236.
Article39. Wu HM, Pan DH, Chung WY, Guo WY, Liu KD, Shiau CY, et al. Gamma knife surgery for the management of intracranial dural arteriovenous fistulas. J Neurosurg. 2006. 12. 105:Suppl. 43–51.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Role of surgery in management of intracranial dural arteriovenous fistulas
- Occurrence of Metachronous Intracranial Dural Arteriovenous Fistula after Embolization of Intracranial Dural Arteriovenous Fistula: A Case Report
- Pathophysiology and classification of intracranial and spinal dural AVF
- Endovascular management of cavernous sinus dural arteriovenous fistulas: Overall review and considerations
- Embryological Consideration of Dural AVFs in Relation to the Neural Crest and the Mesoderm