Old Age at Diagnosis Is Associated With Favorable Outcomes in Korean Patients With Inflammatory Bowel Disease
- Affiliations
-
- 1Division of Gastroenterology and Hepatology, Department of Internal Medicine, Keimyung University School of Medicine, Daegu, Korea. dandy813@hanmail.net
- 2Division of Gastroenterology and Hepatology, Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea.
- KMID: 1807377
- DOI: http://doi.org/10.5217/ir.2015.13.1.60
Abstract
- BACKGROUND/AIMS
Despite the rising incidence and prevalence of inflammatory bowel disease (IBD) in Asian populations, data regarding clinical characteristics of patients in Asia based on age at diagnosis are relatively sparse. The aim of this study was to compare clinical characteristics based on the age at diagnosis according to the Montreal Classification in Korean IBD patients.
METHODS
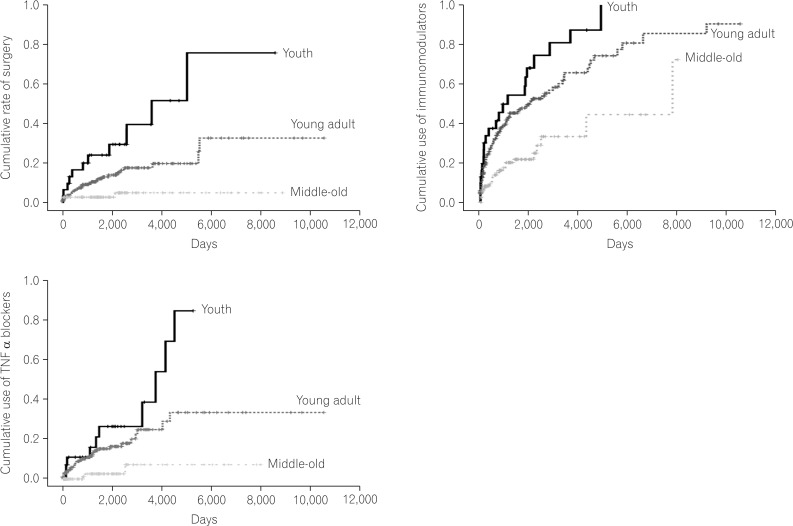
We recruited consecutive patients with IBD at two tertiary hospitals and retrospectively reviewed their medical information. Patients were divided into three groups according to their age at diagnosis: youth (<17 years), young adult (17-40 years), and middle-old (>40 years). The main clinical characteristics for comparison were the achievement of a remission state at the last follow-up visit, cumulative rate of surgery, and cumulative use of immunomodulators and tumor necrosis factor-alpha (TNFalpha) blockers during the follow-up period.
RESULTS
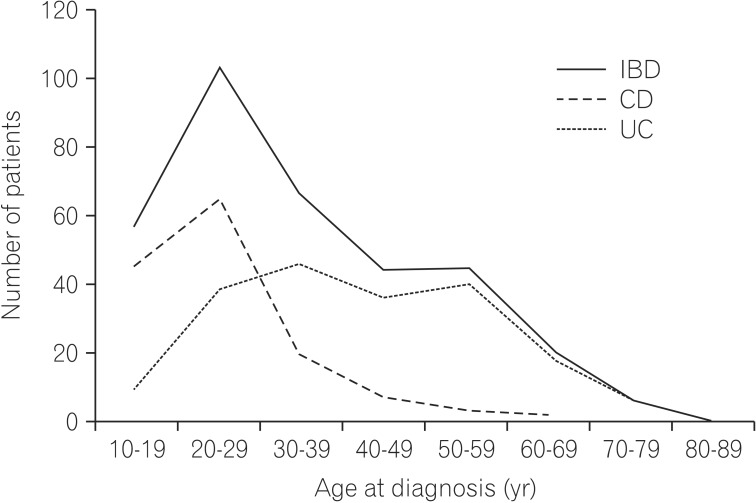
In total, 346 IBD patients were included (Crohn's disease [CD] 146 and ulcerative colitis 200; 36 youth, 202 young adult, and 113 middle-old). The middle-old group with CD was characterized by a predominance of uncomplicated behavior (P=0.013) and a lower frequency of perianal disease (P=0.009). The middle-old group was associated more with a less aggressive disease course than the younger group, as shown by more frequent remission (P=0.004), being less likely to undergo surgery (P<0.001), and lower cumulative use of immunomodulators and TNFalpha blockers (P<0.001).
CONCLUSIONS
Age at diagnosis according to the Montreal Classification is an important prognostic factor for Korean IBD patients.
MeSH Terms
-
Adolescent
Age of Onset
Asia
Asian Continental Ancestry Group
Classification
Colitis, Ulcerative
Crohn Disease
Diagnosis*
Follow-Up Studies
Humans
Immunologic Factors
Incidence
Inflammatory Bowel Diseases*
Prevalence
Prognosis
Retrospective Studies
Tertiary Care Centers
Tumor Necrosis Factor-alpha
Young Adult
Immunologic Factors
Tumor Necrosis Factor-alpha
Figure
Cited by 3 articles
-
Clinical Efficacy of Beclomethasone Dipropionate in Korean Patients with Ulcerative Colitis
Yoon Jee Lee, Jae Hee Cheon, Jae Hyun Kim, SunHo Yoo, Hyun Jung Lee, Soo Jung Park, Sung Pil Hong, Tae Il Kim, Won Ho Kim
Yonsei Med J. 2017;58(1):144-149. doi: 10.3349/ymj.2017.58.1.144.Characteristics and management of patients with inflammatory bowel disease between a secondary and tertiary hospitals: a propensity score analysis
Ki Hwan Song, Eun Soo Kim, Yoo Jin Lee, Byung Ik Jang, Kyeong Ok Kim, Sang Gyu Kwak, Hyun Seok Lee,
Intest Res. 2018;16(2):216-222. doi: 10.5217/ir.2018.16.2.216.Impact of inflammatory bowel disease on daily life: an online survey by the Korean Association for the Study of Intestinal Diseases
Young Sun Kim, Sung-Ae Jung, Kang-Moon Lee, Soo Jung Park, Tae Oh Kim, Chang Hwan Choi, Hyun Gun Kim, Won Moon, Chang Mo Moon, Hye Kyoung Song, Soo-Young Na, Suk-Kyun Yang,
Intest Res. 2017;15(3):338-344. doi: 10.5217/ir.2017.15.3.338.
Reference
-
1. Ananthakrishnan AN, McGinley EL, Binion DG. Inflammatory bowel disease in the elderly is associated with worse outcomes: a national study of hospitalizations. Inflamm Bowel Dis. 2009; 15:182–189. PMID: 18668678.2. Stowe SP, Redmond SR, Stormont JM, et al. An epidemiologic study of inflammatory bowel disease in Rochester, New York. Hospital incidence. Gastroenterology. 1990; 98:104–110. PMID: 2293567.3. Cottone M, Cipolla C, Orlando A, Oliva L, Aiala R, Puleo A. Epidemiology of Crohn's disease in Sicily: a hospital incidence study from 1987 to 1989. "The Sicilian Study Group of Inflammatory Bowel Disease". Eur J Epidemiol. 1991; 7:636–640. PMID: 1783057.4. Sonnenberg A. Age distribution of IBD hospitalization. Inflamm Bowel Dis. 2010; 16:452–457. PMID: 19714765.5. Jang JH, Lee SH, Sung JM, et al. Seasonal variation in flares of inflammatory bowel disease in a Korean population. Intest Res. 2012; 10:161–167.6. Hadithi M, Cazemier M, Meijer GA, et al. Retrospective analysis of old-age colitis in the Dutch inflammatory bowel disease population. World J Gastroenterol. 2008; 14:3183–3187. PMID: 18506923.7. Loftus CG, Loftus EV Jr, Harmsen WS, et al. Update on the incidence and prevalence of Crohn's disease and ulcerative colitis in Olmsted County, Minnesota, 1940-2000. Inflamm Bowel Dis. 2007; 13:254–261. PMID: 17206702.8. Lok KH, Hung HG, Ng CH, et al. Epidemiology and clinical characteristics of ulcerative colitis in Chinese population: experience from a single center in Hong Kong. J Gastroenterol Hepatol. 2008; 23:406–410. PMID: 17623033.9. Fujimoto T, Kato J, Nasu J, et al. Change of clinical characteristics of ulcerative colitis in Japan: analysis of 844 hospital-based patients from 1981 to 2000. Eur J Gastroenterol Hepatol. 2007; 19:229–235. PMID: 17301650.10. Heresbach D, Alexandre JL, Bretagne JF, et al. Crohn's disease in the over-60 age group: a population based study. Eur J Gastroenterol Hepatol. 2004; 16:657–664. PMID: 15201578.11. Riegler G, Tartaglione MT, Carratu R, et al. Age-related clinical severity at diagnosis in 1705 patients with ulcerative colitis: a study by GISC (Italian Colon-Rectum Study Group). Dig Dis Sci. 2000; 45:462–465. PMID: 10749318.12. Page MJ, Poritz LS, Kunselman SJ, Koltun WA. Factors affecting surgical risk in elderly patients with inflammatory bowel disease. J Gastrointest Surg. 2002; 6:606–613. PMID: 12127128.13. Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006; 55:749–753. PMID: 16698746.14. Ha CY, Newberry RD, Stone CD, Ciorba MA. Patients with lateadult-onset ulcerative colitis have better outcomes than those with early onset disease. Clin Gastroenterol Hepatol. 2010; 8:682–687. PMID: 20363368.15. Triantafillidis JK, Emmanouilidis A, Pomonis E, et al. Ulcerative colitis in the elderly: clinical patterns and outcome in 51 Greek patients. J Gastroenterol. 2001; 36:312–316. PMID: 11388393.16. Quezada SM, Steinberger EK, Cross RK. Association of age at diagnosis and Crohn's disease phenotype. Age Ageing. 2013; 42:102–106. PMID: 22918090.17. Lennard-Jones JE. Classification of inflammatory bowel disease. Scand J Gastroenterol. 1989; 24(Suppl s170):2–6.18. Gower-Rousseau C, Salomez JL, Dupas JL, et al. Incidence of inflammatory bowel disease in northern France (1988-1990). Gut. 1994; 35:1433–1438. PMID: 7959201.19. Bernstein CN, Nabalamba A. Hospitalization, surgery, and readmission rates of IBD in Canada: a population-based study. Am J Gastroenterol. 2006; 101:110–118. PMID: 16405542.20. Polito JM 2nd, Childs B, Mellits ED, Tokayer AZ, Harris ML, Bayless TM. Crohn's disease: influence of age at diagnosis on site and clinical type of disease. Gastroenterology. 1996; 111:580–586. PMID: 8780560.21. Ye BD, Yang SK, Cho YK, et al. Clinical features and long-term prognosis of Crohn's disease in Korea. Scand J Gastroenterol. 2010; 45:1178–1185. PMID: 20560811.22. Lapidus A. Crohn's disease in Stockholm County during 1990-2001: an epidemiological update. World J Gastroenterol. 2006; 12:75–81. PMID: 16440421.23. Vind I, Riis L, Jess T, et al. Increasing incidences of inflammatory bowel disease and decreasing surgery rates in Copenhagen City and County, 2003-2005: a population-based study from the Danish Crohn colitis database. Am J Gastroenterol. 2006; 101:1274–1282. PMID: 16771949.24. Yang SK, Yun S, Kim JH, et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986-2005: a KASID study. Inflamm Bowel Dis. 2008; 14:542–549. PMID: 17941073.25. Yao T, Matsui T, Hiwatashi N. Crohn's disease in Japan: diagnostic criteria and epidemiology. Dis Colon Rectum. 2000; 43:S85–S93. PMID: 11052483.26. Leong RW, Lau JY, Sung JJ. The epidemiology and phenotype of Crohn's disease in the Chinese population. Inflamm Bowel Dis. 2004; 10:646–651. PMID: 15472528.27. Bernstein CN, Wajda A, Svenson LW, et al. The epidemiology of inflammatory bowel disease in Canada: a population-based study. Am J Gastroenterol. 2006; 101:1559–1568. PMID: 16863561.28. Jacobsen BA, Fallingborg J, Rasmussen HH, et al. Increase in incidence and prevalence of inflammatory bowel disease in northern Denmark: a population-based study, 1978-2002. Eur J Gastroenterol Hepatol. 2006; 18:601–606. PMID: 16702848.29. Tremaine WJ, Timmons LJ, Loftus EV Jr, et al. Age at onset of inflammatory bowel disease and the risk of surgery for non-neoplastic bowel disease. Aliment Pharmacol Ther. 2007; 25:1435–1441. PMID: 17539983.30. Moum B, Ekbom A, Vatn MH, et al. Clinical course during the 1st year after diagnosis in ulcerative colitis and Crohn's disease. Results of a large, prospective population-based study in southeastern Norway, 1990-93. Scand J Gastroenterol. 1997; 32:1005–1012. PMID: 9361173.31. Horne R, Parham R, Driscoll R, Robinson A. Patients' attitudes to medicines and adherence to maintenance treatment in inflammatory bowel disease. Inflamm Bowel Dis. 2009; 15:837–844. PMID: 19107771.32. D'Inca R, Bertomoro P, Mazzocco K, Vettorato MG, Rumiati R, Sturniolo GC. Risk factors for non-adherence to medication in inflammatory bowel disease patients. Aliment Pharmacol Ther. 2008; 27:166–172. PMID: 17949472.33. Cerveny P, Bortlik M, Kubena A, Vlcek J, Lakatos PL, Lukas M. Nonadherence in inflammatory bowel disease: results of factor analysis. Inflamm Bowel Dis. 2007; 13:1244–1249. PMID: 17538983.34. Gruver AL, Hudson LL, Sempowski GD. Immunosenescence of ageing. J Pathol. 2007; 211:144–156. PMID: 17200946.35. Dorshkind K, Montecino-Rodriguez E, Signer RA. The ageing immune system: is it ever too old to become young again? Nat Rev Immunol. 2009; 9:57–62. PMID: 19104499.36. Park SH, Kim YM, Yang SK, et al. Clinical features and natural history of ulcerative colitis in Korea. Inflamm Bowel Dis. 2007; 13:278–283. PMID: 17206722.37. Fleischer DE, Grimm IS, Friedman LS. Inflammatory bowel disease in older patients. Med Clin North Am. 1994; 78:1303–1319. PMID: 7967911.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Inflammatory Bowel Disease in Pediatric Age
- Diagnosis and Treatment of Inflammatory Bowel Disease
- Abdominal Pain over 6 Months
- Clinical Implication of Sarcopenia in Patients with Inflammatory Bowel Disease
- The Positive Influences of Increasing Age at Diagnosis of Inflammatory Bowel Disease on Disease Prognostication in Asian Perspective