Imaging Sci Dent.
2012 Dec;42(4):249-253. 10.5624/isd.2012.42.4.249.
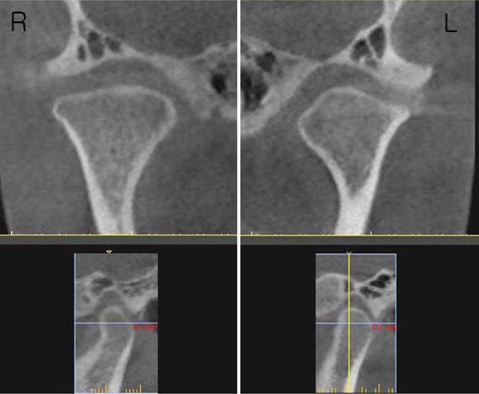
Condylar bony changes in patients with temporomandibular disorders: a CBCT study
- Affiliations
-
- 1Department of Oral and Maxillofacial Radiology, School of Dentistry, Pusan National University, Yangsan, Korea. ksnah@pusan.ac.kr
- KMID: 1806792
- DOI: http://doi.org/10.5624/isd.2012.42.4.249
Abstract
- PURPOSE
Diagnosis of osteoarthritis most commonly depends on clinical and radiographic findings. The present study attempted to observe the bony changes in temporomandibular joint (TMJ) patients from all age groups.
MATERIALS AND METHODS
The first-visit clinical records and cone beam computed tomography (CBCT) data of 440 TMJs from 220 consecutive TMJ patients were reviewed retrospectively.
RESULTS
The most frequent condylar bony change observed was sclerosis (133 joints, 30.2%) followed by surface erosion (129 joints, 29.3%), flattening of the articular surface (112 joints, 25.5%), and deviation in form (58 joints, 13.2%), which included 33 TMJs in a cane-shape, 16 with a lateral or medial pole depression, 6 with posterior condylar surface flattening, and 3 with a bifid-shaped condyle. Fifty-three joints (12.0%) showed hypoplastic condyles but only 1 joint showed hyperplasia. Osteophyte was found in 35 joints (8.0%) and subcortical cyst in 24 joints (5.5%), 5 of which had surface erosion as well. One hundred nineteen joints (27.0%) had only one kind of condylar bony change, 66 joints (15.0%) had two, 52 joints (11.8%) had three, 12 joints (5.0%) had four, and 6 joints (1.4%) had five kinds of condylar bony changes at the same time. Eighty-five (65.9%) of 129 joints with surface erosion had pain recorded at the chief complaint.
CONCLUSION
With more widespread use of CBCT, more specific or detailed guidelines for osteoarthritis are needed.
MeSH Terms
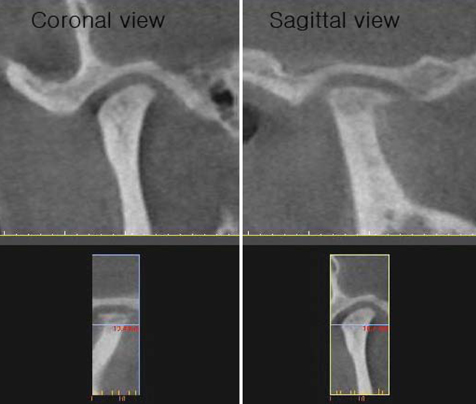
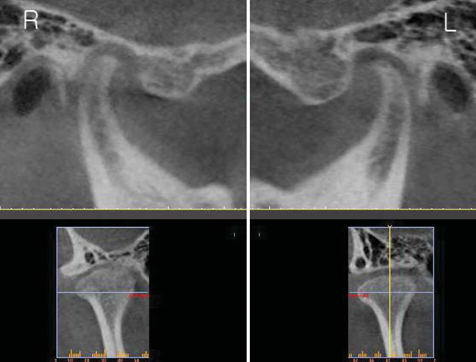
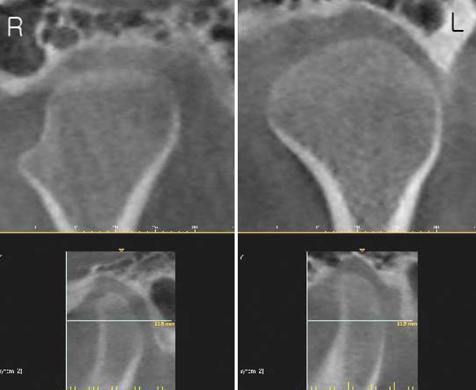
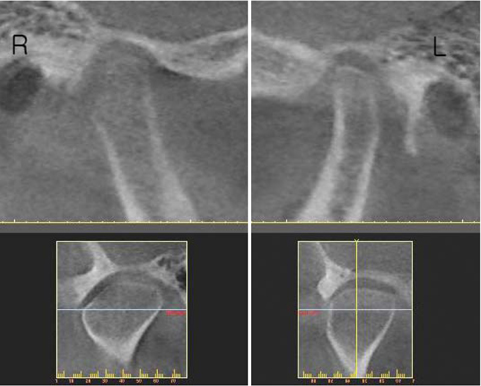
Figure
Cited by 3 articles
-
Three-dimensional cone-beam computed tomography based comparison of condylar position and morphology according to the vertical skeletal pattern
In-Young Park, Ji-Hyun Kim, Yang-Ho Park
Korean J Orthod. 2015;45(2):66-73. doi: 10.4041/kjod.2015.45.2.66.New evolution of cone-beam computed tomography in dentistry: Combining digital technologies
Supreet Jain, Kartik Choudhary, Ravleen Nagi, Stuti Shukla, Navneet Kaur, Deepak Grover
Imaging Sci Dent. 2019;49(3):179-190. doi: 10.5624/isd.2019.49.3.179.Pierre Robin sequence with severe scoliosis in an adult: A case report of clinical and radiological features
Jae-Jun Kim, Dong-Soon Choi, Insan Jang, Bong-Kuen Cha, In-Woo Park
Imaging Sci Dent. 2019;49(4):323-329. doi: 10.5624/isd.2019.49.4.323.
Reference
-
1. Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and maxillofacial pathology. 2002. 2nd ed. Philadelphia: Saunders;755.2. Pereira FJ Jr, Lundh H, Westesson PL. Morphologic changes in the temporomandibular joint in different age groups. An autopsy investigation. Oral Surg Oral Med Oral Pathol. 1994. 78:279–287.3. Zhao YP, Zhang ZY, Wu YT, Zhang WL, Ma XC. Investigation of the clinical and radiographic features of osteoarthrosis of the temporomandibular joints in adolescents and young adults. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011. 111:e27–e34.
Article4. Westesson PL, Katzberg RW, Tallents RH, Sanchez-Woodworth RE, Svensson SA. CT and MR of the temporomandibular joint: comparison with autopsy specimens. AJR Am J Roentgenol. 1987. 148:1165–1171.
Article5. Ahmad M, Hollender L, Anderson Q, Kartha K, Ohrbach R, Truelove EL, et al. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for image analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009. 107:844–860.
Article6. Hintze H, Wiese M, Wenzel A. Cone beam CT and conventional tomography for the detection of morphological temporomandibular joint changes. Dentomaxillofac Radiol. 2007. 36:192–197.
Article7. Petersson A. What you can and cannot see in TMJ imaging - an overview related to the RDC/TMD diagnostic system. J Oral Rehabil. 2010. 37:771–778.
Article8. Larheim TA, Westesson PL. Maxillofacial imaging. 2006. Berlin Heidelberg: Springer-Verlag;149.9. Cevidanes LH, Hajati AK, Paniagua B, Lim PF, Walker DG, Palconet G, et al. Quantification of condylar resorption in temporomandibular joint osteoarthritis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010. 110:110–117.
Article10. Kurita H, Kojima Y, Nakatsuka A, Koike T, Kobayashi H, Kurashina K. Relationship between temporomandibular joint (TMJ)-related pain and morphological changes of the TMJ condyle in patients with temporomandibular disorders. Dentomaxillofac Radiol. 2004. 33:329–333.
Article11. Liu XM, Zhang SY, Yang C, Chen MJ, Y Cai X, Haddad MS, et al. Correlation between disc displacements and locations of disc perforation in the temporomandibular joint. Dentomaxillofac Radiol. 2010. 39:149–156.
Article12. Palconet G, Ludlow JB, Tyndall DA, Lim PF. Correlating cone beam CT results with temporomandibular joint pain of osteoarthritic origin. Dentomaxillofac Radiol. 2012. 41:126–130.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of bony changes between panoramic radiograph and cone beam computed tomographic images in patients with temporomandibular joint disorders
- Correlation between pain and degenerative bony changes on cone-beam computed tomography images of temporomandibular joints
- Cone-beam computed tomographic evaluation of the condylar remodeling occurring after mandibular set-back by bilateral sagittal split ramus osteotomy and rigid fixation
- Evaluation of condylar positions in patients with temporomandibular disorders: A cone-beam computed tomographic study
- Osteoarthritic changes and condylar positioning of the temporomandibular joint in Korean children and adolescents