Pediatr Gastroenterol Hepatol Nutr.
2014 Sep;17(3):162-169. 10.5223/pghn.2014.17.3.162.
Serum Liver Enzyme Pattern in Birth Asphyxia Associated Liver Injury
- Affiliations
-
- 1Department of Pediatrics, Vivekananda Polyclinic and Institute of Medical Sciences, Lucknow, UP, India.
- 2Department of Biostatistics & Health Informatics, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, UP, India.
- 3Department of Gastroenterology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, UP, India. agoel.ag@gmail.com
- KMID: 1803116
- DOI: http://doi.org/10.5223/pghn.2014.17.3.162
Abstract
- PURPOSE
To study temporal pattern of serum liver enzymes levels in newborns with hepatic injury associated with birth asphyxia (BA).
METHODS
Singleton term newborns with BA and < or =72 hours of age admitted to neonatal intensive care unit were prospectively enrolled. Term newborns with physiological jaundice and without BA were studied as controls. Serum liver enzymes were measured at <24 hours, 24-72 hours, and at 6-12 days of age for cases and at 1-6 days of age for controls. BA was defined by 1 minute Apgar score <7 or delayed or absent cry with hypoxic ischemic encephalopathy. BA-associated liver injury was defined as serum alanine aminotransferase (ALT) elevation beyond +2 standard deviation (ALT > +2 SD) above the mean of control subjects at any of the three time points.
RESULTS
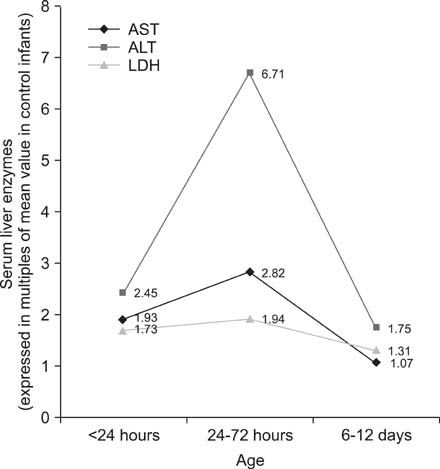
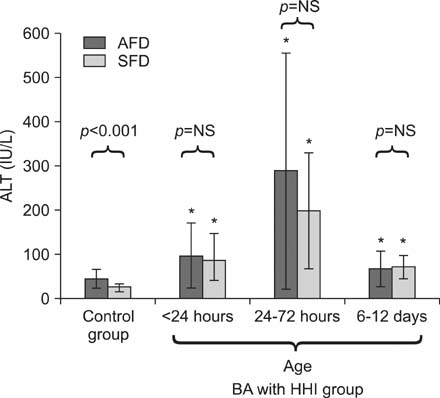
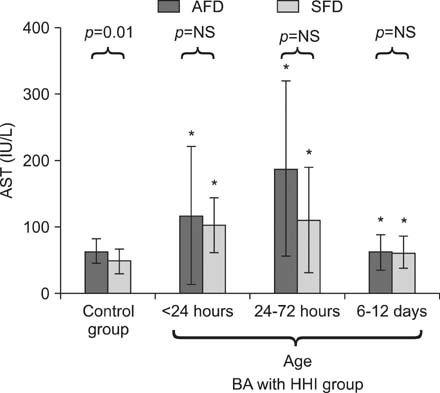
Sixty controls and 62 cases were enrolled. Thirty-five cases (56%) developed BA-associated liver injury (ALT>81 IU/L). They had higher serum levels of ALT, aspartate aminotransferase, lactate dehydrogenase than the control infants, with peak at 24-72 hours. In controls, serum liver enzyme levels were significantly higher in appropriate-for-date (AFD) babies than small-for-date (SFD) babies. Serum enzyme pattern and extent of elevation were comparable between SFD and AFD babies. Degree of serum liver enzyme elevation had no relationship with severity of hypoxic encephalopathy.
CONCLUSION
Serum liver enzyme elevation is common in BA; it peaks at 24-72 hours followed by a sharp decline by 6-12 days of age. Pattern and extent of enzyme elevation are comparable between SFD and AFD babies.
Keyword
MeSH Terms
-
Alanine Transaminase
Apgar Score
Aspartate Aminotransferases
Asphyxia Neonatorum
Asphyxia*
Hepatitis
Humans
Hypoxia, Brain
Hypoxia-Ischemia, Brain
Infant
Infant, Newborn
Intensive Care, Neonatal
Ischemia
Jaundice
L-Lactate Dehydrogenase
Liver*
Parturition*
Prospective Studies
Transaminases
Alanine Transaminase
Aspartate Aminotransferases
L-Lactate Dehydrogenase
Transaminases
Figure
Cited by 1 articles
-
Validation of Serum Aminotransferases Levels to Define Severe Dengue Fever in Children
Geetika Srivastava, Nanda Chhavi, Amit Goel
Pediatr Gastroenterol Hepatol Nutr. 2018;21(4):289-296. doi: 10.5223/pghn.2018.21.4.289.
Reference
-
1. NNPD Network, Indian Council of Medical Research, National Neonatology Forum (India). National neonatal-perinatal database: report 2002-2003. New Delhi: Nodal Centre, AIIMS;2005.2. Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012; 380:2095–2128.3. Shah P, Riphagen S, Beyene J, Perlman M. Multiorgan dysfunction in infants with post-asphyxial hypoxic-ischaemic encephalopathy. Arch Dis Child Fetal Neonatal Ed. 2004; 89:F152–F155.
Article4. Hankins GD, Koen S, Gei AF, Lopez SM, Van Hook JW, Anderson GD. Neonatal organ system injury in acute birth asphyxia sufficient to result in neonatal encephalopathy. Obstet Gynecol. 2002; 99:688–691.
Article5. Al-Macki N, Miller SP, Hall N, Shevell M. The spectrum of abnormal neurologic outcomes subsequent to term intrapartum asphyxia. Pediatr Neurol. 2009; 41:399–405.
Article6. Volpe J. Neurology of the newborn. 4th ed. Philadelphia: WB Saunders;2001.7. Sarnat HB, Sarnat MS. Neonatal encephalopathy following fetal distress. A clinical and electroencephalographic study. Arch Neurol. 1976; 33:696–705.8. Gupta BD, Sharma P, Bagla J, Parakh M, Soni JP. Renal failure in asphyxiated neonates. Indian Pediatr. 2005; 42:928–934.9. Jayashree G, Dutta AK, Sarna MS, Saili A. Acute renal failure in asphyxiated newborns. Indian Pediatr. 1991; 28:19–23.10. Shastri AT, Samarasekara S, Muniraman H, Clarke P. Cardiac troponin I concentrations in neonates with hypoxic-ischaemic encephalopathy. Acta Paediatr. 2012; 101:26–29.
Article11. Kanik E, Ozer EA, Bakiler AR, Aydinlioglu H, Dorak C, Dogrusoz B, et al. Assessment of myocardial dysfunction in neonates with hypoxic-ischemic encephalopathy: is it a significant predictor of mortality? J Matern Fetal Neonatal Med. 2009; 22:239–242.
Article12. Rennie JM, Roberton NRC. Textbook of neonatology. 3rd ed. Edinburgh: Churchill Livingstone;1999.13. Jensen A, Garnier Y, Berger R. Dynamics of fetal circulatory responses to hypoxia and asphyxia. Eur J Obstet Gynecol Reprod Biol. 1999; 84:155–172.
Article14. Tarcan A, Tiker F, Güvenir H, Gürakan B. Hepatic involvement in perinatal asphyxia. J Matern Fetal Neonatal Med. 2007; 20:407–410.
Article15. Feldman M, Lawrence SF, Lawrence JB. Sleisenger and Fordtran's gastrointestinal and liver disease: pathophysiology, diagnosis, management. 9th ed. Philadelphia: Saunders Elsevier;2010.16. Schiff ER, Sorrell MF, Maddrey WC. Schiff's diseases of the liver. 10th ed. Philadelphia: Lippincott Williams & Wilkins;2007.17. Karlsson M, Blennow M, Nemeth A, Winbladh B. Dynamics of hepatic enzyme activity following birth asphyxia. Acta Paediatr. 2006; 95:1405–1411.
Article18. Godambe SV, Udani RH, Malik S, Kandalkar BM. Hepatic profile in asphyxia neonatorum. Indian Pediatr. 1997; 34:927–930.19. Prati D, Taioli E, Zanella A, Della Torre E, Butelli S, Del Vecchio E, et al. Updated definitions of healthy ranges for serum alanine aminotransferase levels. Ann Intern Med. 2002; 137:1–10.
Article20. Córdoba J, O'Riordan K, Dupuis J, Borensztajin J, Blei AT. Diurnal variation of serum alanine transaminase activity in chronic liver disease. Hepatology. 1998; 28:1724–1725.
Article21. Ramakumar L, Dogra KN, Sood SC. Serum transaminases in the newborn. Indian Pediatr. 1965; 2:43–48.22. Park SH, Park HY, Kang JW, Park J, Shin KJ. Aminotransferase upper reference limits and the prevalence of elevated aminotransferases in the Korean adolescent population. J Pediatr Gastroenterol Nutr. 2012; 55:668–672.
Article23. Henrion J. Hypoxic hepatitis. Liver Int. 2012; 32:1039–1052.
Article24. Kocylowski R, Dubiel M, Gudmundsson S, Fritzer E, Kiserud T, von Kaisenberg C. Hepatic aminotransferases of normal and IUGR fetuses in cord blood at birth. Early Hum Dev. 2012; 88:461–465.
Article25. Birrer R, Takuda Y, Takara T. Hypoxic hepatopathy: pathophysiology and prognosis. Intern Med. 2007; 46:1063–1070.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Drug Induced Liver Injury by Prophylactic Administration of Albendazole
- A study of auditory brainstem in neonates with birth asphyxia
- Changes of Serum Lipid Concentration and Serum Liver Enzyme Levels During Etretinate Treatment in Patients with Psoriasis
- A study of serum and spinal fluid enzyme such as CPK and LDH as predictors of neurologic disability following perinatal asphyxia
- A Case of Intrauterine Intracranial Hemorrhage due to Coagulopathy Caused by Chronic Intrauterine Liver Failure