J Korean Assoc Oral Maxillofac Surg.
2015 Jun;41(3):156-164. 10.5125/jkaoms.2015.41.3.156.
Stability of unilateral sagittal split ramus osteotomy for correction of facial asymmetry: long-term case series and literature review
- Affiliations
-
- 1Ilsan Ye Dental Clinic, Goyang, Korea.
- 2Graduate School of Clinical Dentistry, Ewha Womans University, Seoul, Korea.
- 3Department of Oral and Maxillofacial Surgery, School of Medicine and Institute of Health Science, Gyeongsang National University, Jinju, Korea. parkbw@gnu.ac.kr
- 4Department of Oral and Maxillofacial Surgery, School of Dentistry, Pusan National University, Yangsan, Korea.
- 5Department of Oral and Maxillofacial Surgery, Jaw and Face Surgery Center, On General Hospital, Busan, Korea.
- KMID: 1797847
- DOI: http://doi.org/10.5125/jkaoms.2015.41.3.156
Abstract
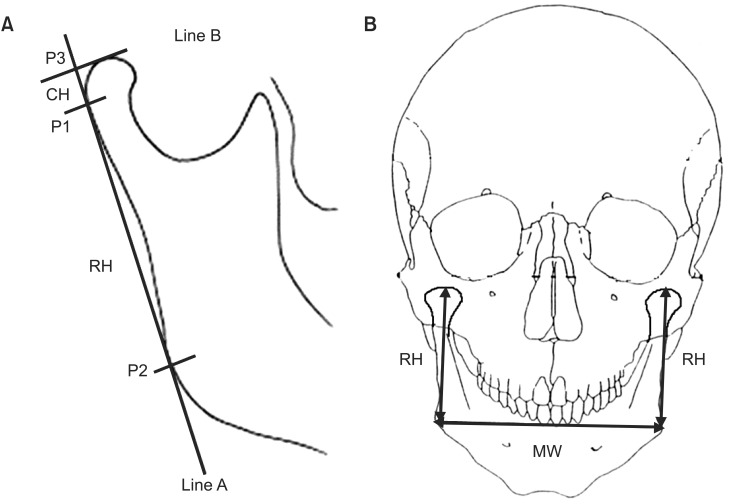
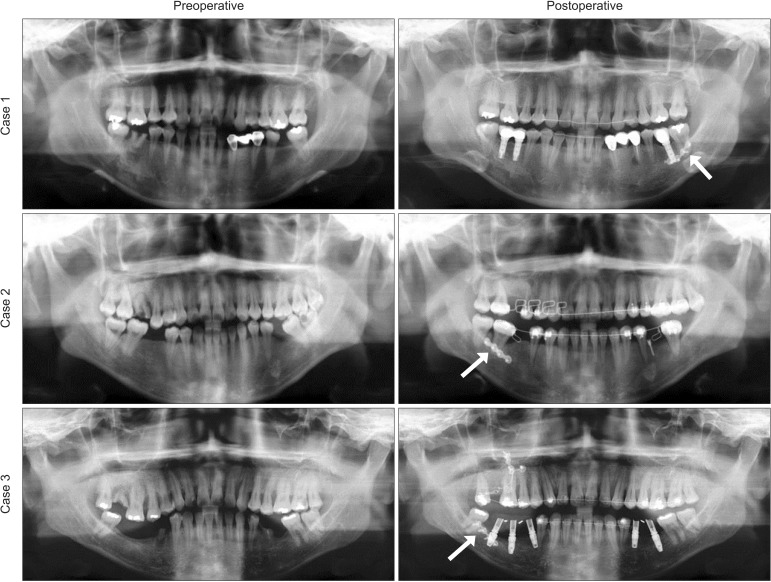
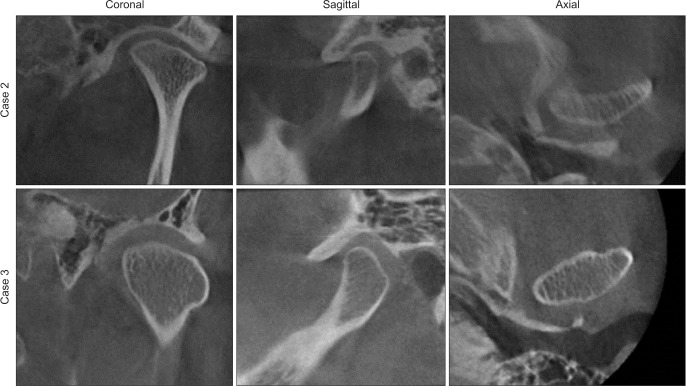
- Bilateral sagittal split ramus osteotomy is considered a standard technique in mandibular orthognathic surgeries to reduce unexpected bilateral stress in the temporomandibular joints. Unilateral sagittal split ramus osteotomy (USSO) was recently introduced to correct facial asymmetry caused by asymmetric mandibular prognathism and has shown favorable outcomes. If unilateral surgery could guarantee long-term postoperative stability as well as favorable results, operation time and the incidence of postoperative complications could be reduced compared to those in bilateral surgery. This report highlights three consecutive cases with long-term follow-up in which USSO was used to correct asymmetric mandibular prognathism. Long-term postoperative changes in the condylar contour and ramus and condylar head length were analyzed using routine radiography and computed tomography. In addition, prior USSO studies were reviewed to outline clear criteria for applying this technique. In conclusion, patients showing functional-type asymmetry with predicted unilateral mandibular movement of less than 7 mm can be considered suitable candidates for USSO-based correction of asymmetric mandibular prognathism with or without maxillary arch surgeries.
Keyword
MeSH Terms
Figure
Reference
-
1. Trauner R, Obwegeser H. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty. I. Surgical procedures to correct mandibular prognathism and reshaping of the chin. Oral Surg Oral Med Oral Pathol. 1957; 10:677–689. PMID: 13441284.2. Borstlap WA, Stoelinga PJ, Hoppenreijs TJ, van't Hof MA. Stabilisation of sagittal split advancement osteotomies with miniplates: a prospective, multicentre study with two-year follow-up. Part III--condylar remodelling and resorption. Int J Oral Maxillofac Surg. 2004; 33:649–655. PMID: 15337177.3. Wohlwender I, Daake G, Weingart D, Brandstätter A, Kessler P, Lethaus B. Condylar resorption and functional outcome after unilateral sagittal split osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011; 112:315–321. PMID: 21292514.
Article4. Falter B, Schepers S, Vrielinck L, Lambrichts I, Thijs H, Politis C. Occurrence of bad splits during sagittal split osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 110:430–435. PMID: 20452254.
Article5. Cutbirth M, Van Sickels JE, Thrash WJ. Condylar resorption after bicortical screw fixation of mandibular advancement. J Oral Maxillofac Surg. 1998; 56:178–182. PMID: 9461141.
Article6. Habets LL, Bezuur JN, Naeiji M, Hansson TL. The orthopantomogram, an aid in diagnosis of temporomandibular joint problems. II. The vertical symmetry. J Oral Rehabil. 1988; 15:465–471. PMID: 3244055.7. Snodell SF, Nanda RS, Currier GF. A longitudinal cephalometric study of transverse and vertical craniofacial growth. Am J Orthod Dentofacial Orthop. 1993; 104:471–483. PMID: 8237899.
Article8. Kilic N, Kiki A, Oktay H. Condylar asymmetry in unilateral posterior crossbite patients. Am J Orthod Dentofacial Orthop. 2008; 133:382–387. PMID: 18331937.
Article9. Cheong YW, Lo LJ. Facial asymmetry: etiology, evaluation, and management. Chang Gung Med J. 2011; 34:341–351. PMID: 21880188.10. Primozic J, Perinetti G, Richmond S, Ovsenik M. Three-dimensional evaluation of facial asymmetry in association with unilateral functional crossbite in the primary, early, and late mixed dentition phases. Angle Orthod. 2013; 83:253–258. PMID: 22889202.
Article11. Motamedi MH. Treatment of condylar hyperplasia of the mandible using unilateral ramus osteotomies. J Oral Maxillofac Surg. 1996; 54:1161–1169. PMID: 8859233.
Article12. Merkx MA, Van Damme PA. Condylar resorption after orthognathic surgery. Evaluation of treatment in 8 patients. J Craniomaxillofac Surg. 1994; 22:53–58. PMID: 8175999.13. Westermark A. LactoSorb resorbable osteosynthesis after sagittal split osteotomy of the mandible: a 2-year follow-up. J Craniofac Surg. 1999; 10:519–522. PMID: 10726505.14. Ozdemir R, Baran CN, Karagoz MA, Dogan S. Place of sagittal split osteotomy in mandibular surgery. J Craniofac Surg. 2009; 20:349–355. PMID: 19326485.
Article15. Fujita T, Shirakura M, Koh M, Itoh G, Hayashi H, Tanne K. Changes in the lip-line in asymmetrical cases treated with isolated mandibular surgery. J Orthod. 2013; 40:313–317. PMID: 24297963.
Article16. Rubens BC, Stoelinga PJ, Weaver TJ, Blijdorp PA. Management of malunited mandibular condylar fractures. Int J Oral Maxillofac Surg. 1990; 19:22–25. PMID: 2110955.
Article17. Wong GB. Large odontogenic myxoma of the mandible treated by sagittal ramus osteotomy and peripheral ostectomy. J Oral Maxillofac Surg. 1992; 50:1221–1224. PMID: 1403280.
Article18. Becking AG, Zijderveld SA, Tuinzing DB. Management of post-traumatic malocclusion caused by condylar process fractures. J Oral Maxillofac Surg. 1998; 56:1370–1374. PMID: 9846532.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unilateral intraoral vertical ramus osteotomy and sagittal split ramus osteotomy for the treatment of asymmetric mandibles
- Unilateral bimaxillary vertical elongation by maxillary distraction osteogenesis and mandibular sagittal split ramus osteotomy: a case report
- Facial palsy after sagittal split ramus osteotomies: Case report
- Correction of Facial Asymmetry Using Costochondral Graft and Orthognathic Surgery in Hemifacial Microsomia Patient: Case Report
- Sagittal split ramus osteotomy, intraoral vertical ramus osteotomy, and lateral corticectomy for asymmetric mandibular prognathism