J Korean Med Sci.
2014 Sep;29(9):1260-1265. 10.3346/jkms.2014.29.9.1260.
Results of Surgical Treatment on Benign Anal Diseases in Korean HIV-Positive Patients
- Affiliations
-
- 1Department of Surgery, Seoul National University Bundang Hospital, Seongnam, Korea.
- 2Department of Surgery, Seoul National University College of Medicine, Seoul, Korea. kjparkmd@plaza.snu.ac.kr
- KMID: 1794605
- DOI: http://doi.org/10.3346/jkms.2014.29.9.1260
Abstract
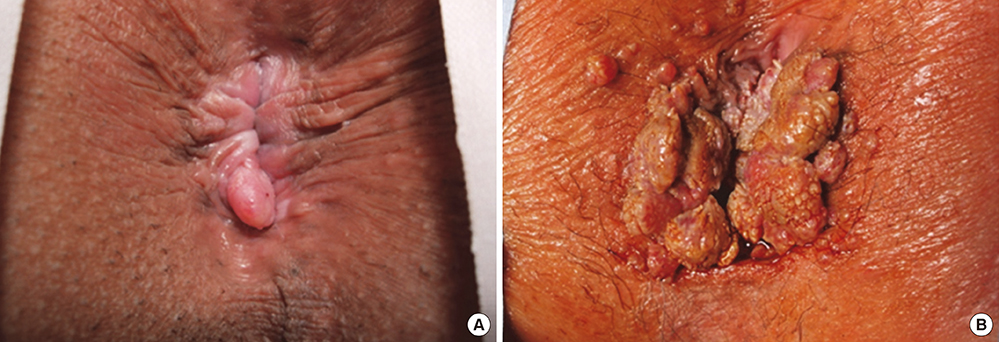
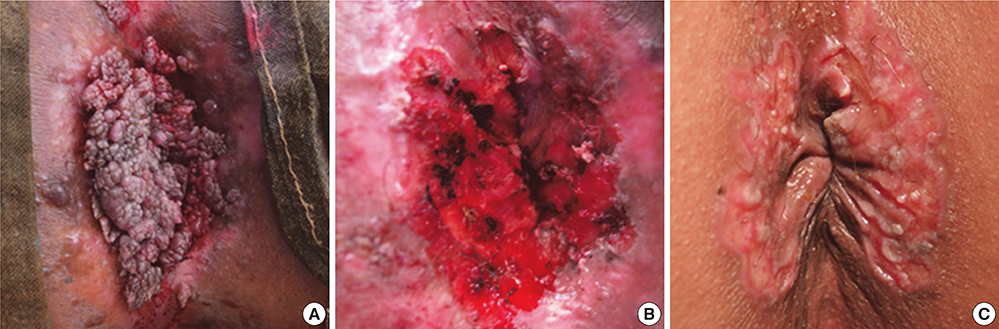
- Perianal diseases are the most common reasons for surgery in HIV-positive patients. This study aimed to evaluate the outcomes of these surgical procedures in Korean patients, focusing on wound healing and postoperative complications. Retrospective analysis was performed on 72 HIV-positive patients who underwent surgery by a single surgeon for benign anal disease between 1998 and 2011. Of these, 68.1% (49/72) of patients received surgery for condyloma acuminata, 19.4% (14/72) for anal fistulas, 6.9% (5/72) for hemorrhoids, and 5.6% (4/72) for perianal abscesses. Patients with condyloma acuminata received surgical excision with electrical coagulation, and all wounds healed completely within 3 months, though 16.3% (8/49) of these patients experienced recurrence. Twelve of the 49 patients (24.5%) who were treated for condyloma acuminata underwent simultaneous operations for concomitant anal fistulas (n = 6), hemorrhoids (n = 4), and perianal abscesses (n = 2). Overall, 3 postoperative complications developed following a total of 94 procedures, and there was no significant increase in complication rate for patients with a low CD4+ T-cell count ( < 200/microL) compared to those with a higher count. The results demonstrate favorable results following perianal surgery in HIV-positive Korean patients.
MeSH Terms
-
Adult
Aged
Anus Diseases/complications/*surgery
Asian Continental Ancestry Group
CD4-Positive T-Lymphocytes/cytology
Condylomata Acuminata/surgery
Female
HIV Infections/*complications
Hemorrhoids/surgery
Humans
Male
Middle Aged
Postoperative Complications
Rectal Fistula/surgery
Republic of Korea
Retrospective Studies
Treatment Outcome
Wound Healing
Young Adult
Figure
Reference
-
1. United Nations Programme on HIV/AIDS. UNAIDS report on the global AIDS epidemic 2013. accessed on 15 May 2014. Available at http://www.unaids.org/en/dataanalysis/knowyourepidemic.2. Korea Centers for Disease Control and Prevention. Annual report on the notified HIV/AIDS in Korea. accessed on 15 May 2014. Available at http://aidsinfo.cdc.go.kr/aidsinfo/user/jsp/ud/ud04_1ht01i.jsp.3. Miles AJ, Mellor CH, Gazzard B, Allen-Mersh TG, Wastell C. Surgical management of anorectal disease in HIV-positive homosexuals. Br J Surg. 1990; 77:869–871.4. Wexner SD, Smithy WB, Milsom JW, Dailey TH. The surgical management of anorectal diseases in AIDS and pre-AIDS patients. Dis Colon Rectum. 1986; 29:719–723.5. Consten EC, Slors FJ, Noten HJ, Oosting H, Danner SA, van Lanschot JJ. Anorectal surgery in human immunodeficiency virus-infected patients: clinical outcome in relation to immune status. Dis Colon Rectum. 1995; 38:1169–1175.6. Burke EC, Orloff SL, Freise CE, Macho JR, Schecter WP. Wound healing after anorectal surgery in human immunodeficiency virus-infected patients. Arch Surg. 1991; 126:1267–1270.7. Hwang DY, Lee JS, Yoon SG, Rhyou JH, Song SG, Lee JK. Benign anal diseases on patients with HIV disease. J Korean Soc Coloproctol. 2003; 19:1–5.8. Centers for Disease Control (CDC). Update: universal precautions for prevention of transmission of human immunodeficiency virus, hepatitis B virus, and other bloodborne pathogens in health-care settings. MMWR Morb Mortal Wkly Rep. 1988; 37:377–382. 387–388.9. From the Centers for Disease Control and Prevention. 1993 revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults. JAMA. 1993; 269:729–730.10. Nadal SR, Manzione CR, Galvão VM, Salim VR, Speranzini MB. Perianal diseases in HIV-positive patients compared with a seronegative population. Dis Colon Rectum. 1999; 42:649–654.11. Yuhan R, Orsay C, DelPino A, Pearl R, Pulvirenti J, Kay S, Abcarian H. Anorectal disease in HIV-infected patients. Dis Colon Rectum. 1998; 41:1367–1370.12. Barrett WL, Callahan TD, Orkin BA. Perianal manifestations of human immunodeficiency virus infection: experience with 260 patients. Dis Colon Rectum. 1998; 41:606–611.13. Safavi A, Gottesman L, Dailey TH. Anorectal surgery in the HIV+ patient: update. Dis Colon Rectum. 1991; 34:299–304.14. Anderson CA, Boller AM, Richardson CJ, Balcos EG, Zera RT. Anal condyloma: a comparison between HIV positive and negative patients. Am Surg. 2004; 70:1014–1018.15. Manzione CR, Nadal SR, Calore EE. Postoperative follow-up of anal condylomata acuminata in HIV-positive patients. Dis Colon Rectum. 2003; 46:1358–1365.16. Diamond C, Taylor TH, Aboumrad T, Bringman D, Anton-Culver H. Increased incidence of squamous cell anal cancer among men with AIDS in the era of highly active antiretroviral therapy. Sex Transm Dis. 2005; 32:314–320.17. Wòjciak B, Crossan JF. The effects of T cells and their products on in vitro healing of epitenon cell microwounds. Immunology. 1994; 83:93–98.18. Nadal SR, Manzione CR, Galvao VM, Salim VR, Speranzini MB. Healing after anal fistulotomy: comparative study between HIV+ and HIV-patients. Dis Colon Rectum. 1998; 41:177–179.19. Lord RV. Anorectal surgery in patients infected with human immunodeficiency virus: factors associated with delayed wound healing. Ann Surg. 1997; 226:92–99.20. Orkin BA, Smith LE. Perineal manifestations of HIV infection. Dis Colon Rectum. 1992; 35:310–314.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Benign Anal Diseases on Patients with HIV Disease
- Detection and Typing of Human Papillomavirus in Anal Condyloma Acuminatum of HIV-positive Patients
- Association of Immune Status with Recurrent Anal Condylomata in Human Immunodeficiency Virus-Positive Patients
- A Case Report of Surgical Treatment of Anal Condyloma Acuminata in HIV-Infected Patient
- A Case of Management of Benign Lymphoepithelial Cysts of the Parotid Gland in Patient Infected with Human Immunodeficiency Virus