Yonsei Med J.
2013 Sep;54(5):1266-1272. 10.3349/ymj.2013.54.5.1266.
Kidney Function in Living Donors Undergoing Nephrectomy by Sevoflurane or Desflurane Anesthesia
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Anesthesia and Pain Research Institute, Yonsei University College of Medicine, Seoul, Korea. csho99@yuhs.ac
- 2Department of Surgery, The Research Institute for Transplantation, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 1793178
- DOI: http://doi.org/10.3349/ymj.2013.54.5.1266
Abstract
- PURPOSE
Although there is no clinical evidence of nephrotoxicity with the volatile anesthetics currently used in general anesthesia, a better agent should be needed in terms of preserving postoperative renal function in living kidney donors who have only single remaining kidney. The purpose of the current retrospective, single-center study was to evaluate and compare renal function of living kidney donors after nephrectomy under either sevoflurane or desflurane anesthesia.
MATERIALS AND METHODS
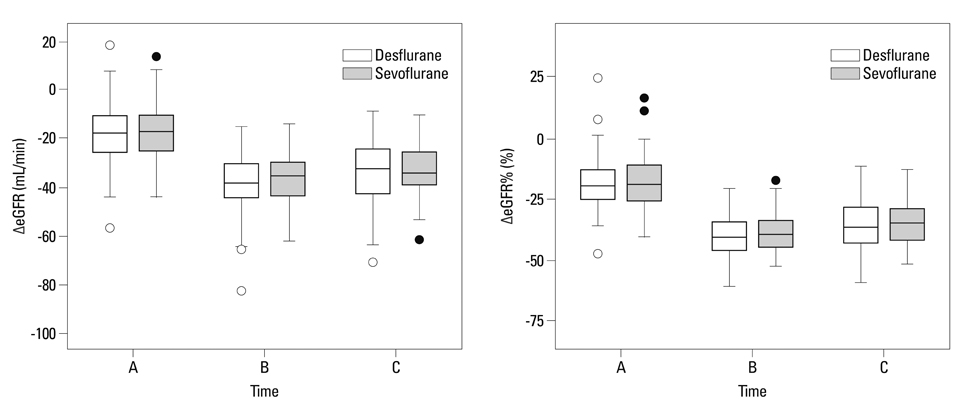
From January 2006 through December 2011, a total of 228 donors undergoing video assisted minilaparotomy surgery nephrectomy for kidney donation were retrospectively enrolled in the current study. The donors were categorized into a sevoflurane group or desflurane group based on the type of volatile anesthetic used. We collected laboratory data from the patients preoperatively, immediately after the operation, on the first postoperative day and on the third postoperative day. We also compared renal function of the kidney donors after donor nephrectomy by comparing creatinine level and estimated glomerular filtration rate (eGFR).
RESULTS
The decrease in renal function after surgery in both groups was the most prominent on the first postoperative day. There were no significant differences between the two groups in postoperative changes of creatinine or eGFR.
CONCLUSION
Sevoflurane and desflurane can be used safely as volatile anesthetics in donors undergoing nephrectomy.
Keyword
MeSH Terms
-
Adult
Anesthesia, General/methods
Anesthetics, Inhalation/adverse effects/*therapeutic use
Female
Humans
Isoflurane/adverse effects/*analogs & derivatives/therapeutic use
Kidney/*physiology
Kidney Function Tests
*Kidney Transplantation
*Living Donors
Male
Methyl Ethers/adverse effects/*therapeutic use
*Nephrectomy
Postoperative Complications
Retrospective Studies
Anesthetics, Inhalation
Isoflurane
Methyl Ethers
Figure
Reference
-
1. Ommen ES, Winston JA, Murphy B. Medical risks in living kidney donors: absence of proof is not proof of absence. Clin J Am Soc Nephrol. 2006; 1:885–895.
Article2. Ibrahim HN, Foley R, Tan L, Rogers T, Bailey RF, Guo H, et al. Long-term consequences of kidney donation. N Engl J Med. 2009; 360:459–469.
Article3. Gossmann J, Wilhelm A, Kachel HG, Jordan J, Sann U, Geiger H, et al. Long-term consequences of live kidney donation follow-up in 93% of living kidney donors in a single transplant center. Am J Transplant. 2005; 5:2417–2424.
Article4. Tent H, Sanders JS, Rook M, Hofker HS, Ploeg RJ, Navis G, et al. Effects of preexistent hypertension on blood pressure and residual renal function after donor nephrectomy. Transplantation. 2012; 93:412–417.
Article5. Modesti C, Sacco T, Morelli G, Bocci MG, Ciocchetti P, Vitale F, et al. Balanced anestesia versus total intravenous anestesia for kidney transplantation. Minerva Anestesiol. 2006; 72:627–635.6. Teixeira S, Costa G, Costa F, da Silva Viana J, Mota A. Sevoflurane versus isoflurane: does it matter in renal transplantation? Transplant Proc. 2007; 39:2486–2488.
Article7. Shah VR, Butala BP, Parikh GP, Vora KS, Parikh BK, Modi MP, et al. Combined epidural and general anesthesia for paediatric renal transplantation-a single center experience. Transplant Proc. 2008; 40:3451–3454.
Article8. Bhosale G, Shah V. Combined spinal-epidural anesthesia for renal transplantation. Transplant Proc. 2008; 40:1122–1124.
Article9. Campagna JA, Miller KW, Forman SA. Mechanisms of actions of inhaled anesthetics. N Engl J Med. 2003; 348:2110–2124.
Article10. Young CJ, Apfelbaum JL. Inhalational anesthetics: desflurane and sevoflurane. J Clin Anesth. 1995; 7:564–577.
Article11. Kim JM, Lee JH, Lee HJ, Koo BN. Comparison of emergence time in children undergoing minor surgery according to anesthetic: desflurane and sevoflurane. Yonsei Med J. 2013; 54:732–738.
Article12. Kim ES, Chang HW. The effects of a single bolus of remifentanil on corrected QT interval change during sevoflurane induction. Yonsei Med J. 2011; 52:333–338.
Article13. Chang DJ, Choi SH, Choi YS, Min KT. Effect of charcoal filter on the emergence from sevoflurane anesthesia in a semi-closed rebreathing circuit. Yonsei Med J. 2011; 52:668–672.
Article14. Kobayashi Y, Ochiai R, Takeda J, Sekiguchi H, Fukushima K. Serum and urinary inorganic fluoride concentrations after prolonged inhalation of sevoflurane in humans. Anesth Analg. 1992; 74:753–757.
Article15. Keller KA, Callan C, Prokocimer P, Delgado-Herrera L, Friedman MB, Hoffman GM, et al. Inhalation toxicity study of a haloalkene degradant of sevoflurane, Compound A (PIFE), in Sprague-Dawley rats. Anesthesiology. 1995; 83:1220–1232.
Article16. Smiley RM, Ornstein E, Pantuck EJ, Pantuck CB, Matteo RS. Metabolism of desflurane and isoflurane to fluoride ion in surgical patients. Can J Anaesth. 1991; 38:965–968.
Article17. Goldberg ME, Cantillo J, Larijani GE, Torjman M, Vekeman D, Schieren H. Sevoflurane versus isoflurane for maintenance of anesthesia: are serum inorganic fluoride ion concentrations of concern? Anesth Analg. 1996; 82:1268–1272.18. Ebert TJ, Arain SR. Renal responses to low-flow desflurane, sevoflurane, and propofol in patients. Anesthesiology. 2000; 93:1401–1406.
Article19. Mazze RI. The safety of sevoflurane in humans. Anesthesiology. 1992; 77:1062–1063.
Article20. Ko JS, Gwak MS, Choi SJ, Yang M, Kim MJ, Lee JY, et al. The effects of desflurane and sevoflurane on hepatic and renal functions after right hepatectomy in living donors*. Transpl Int. 2010; 23:736–744.
Article21. Kim SI, Rha KH, Lee JH, Kim HJ, Kwon KI, Kim YS, et al. Favorable outcomes among recipients of living-donor nephrectomy using video-assisted minilaparotomy. Transplantation. 2004; 77:1725–1728.
Article22. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. Modification of Diet in Renal Disease Study Group. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med. 1999; 130:461–470.
Article23. Fang ZX, Kandel L, Laster MJ, Ionescu P, Eger EI. Factors affecting production of compound A from the interaction of sevoflurane with Baralyme and soda lime. Anesth Analg. 1996; 82:775–781.
Article24. Cousins MJ, Mazze RI. Methoxyflurane nephrotoxicity. A study of dose response in man. JAMA. 1973; 225:1611–1616.
Article25. Mazze RI, Calverley RK, Smith NT. Inorganic fluoride nephrotoxicity: prolonged enflurane and halothane anesthesia in volunteers. Anesthesiology. 1977; 46:265–271.26. Frink EJ Jr, Malan TP, Atlas M, Dominguez LM, DiNardo JA, Brown BR Jr. Clinical comparison of sevoflurane and isoflurane in healthy patients. Anesth Analg. 1992; 74:241–245.
Article27. Kharasch ED, Hankins DC, Thummel KE. Human kidney methoxyflurane and sevoflurane metabolism. Intrarenal fluoride production as a possible mechanism of methoxyflurane nephrotoxicity. Anesthesiology. 1995; 82:689–699.28. Conzen PF, Kharasch ED, Czerner SF, Artru AA, Reichle FM, Michalowski P, et al. Low-flow sevoflurane compared with low-flow isoflurane anesthesia in patients with stable renal insufficiency. Anesthesiology. 2002; 97:578–584.
Article29. Bito H, Ikeuchi Y, Ikeda K. Effects of low-flow sevoflurane anesthesia on renal function: comparison with high-flow sevoflurane anesthesia and low-flow isoflurane anesthesia. Anesthesiology. 1997; 86:1231–1237.30. Vats HS, Rayhill SC, Thomas CP. Early postnephrectomy donor renal function: laparoscopic versus open procedure. Transplantation. 2005; 79:609–612.
Article31. Bito H, Ikeda K. Closed-circuit anesthesia with sevoflurane in humans. Effects on renal and hepatic function and concentrations of breakdown products with soda lime in the circuit. Anesthesiology. 1994; 80:71–76.
Article32. Moore E, Bellomo R, Nichol A. Biomarkers of acute kidney injury in anesthesia, intensive care and major surgery: from the bench to clinical research to clinical practice. Minerva Anestesiol. 2010; 76:425–440.33. McIlroy DR, Wagener G, Lee HT. Biomarkers of acute kidney injury: an evolving domain. Anesthesiology. 2010; 112:998–1004.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changes of renal function in the remaining kidney after donor nephrectomy
- Living Donor Nephrectomy: Surgical Selection Criteria of Laterality
- Comparison of postoperative renal and hepatic function between desflurane-remifentanil and propofol-remifentanil for nephrectomy
- Cerebrovascular reactivity to hypercapnia during sevoflurane or desflurane anesthesia in rats
- Recovery Profile after Inhalation Anesthesia Using Sevoflurane and Desflurane