J Korean Med Sci.
2011 Jun;26(6):765-770. 10.3346/jkms.2011.26.6.765.
Effect of Aspirin on the Expression of Hepatocyte NF-kappaB and Serum TNF-alpha in Streptozotocin-Induced Type 2 Diabetic Rats
- Affiliations
-
- 1Department of Endocrinology and Metabolism, West China Hospital, Sichuan University, Chengdu, China. sxdfriend@sina.com
- 2Department of Pathology, 401 Hospital of Chinese People's Liberation Army, Qingdao, China.
- 3Department of Laboratory Medicine, Qingdao Municipal Hospital, Qingdao, China.
- KMID: 1785962
- DOI: http://doi.org/10.3346/jkms.2011.26.6.765
Abstract
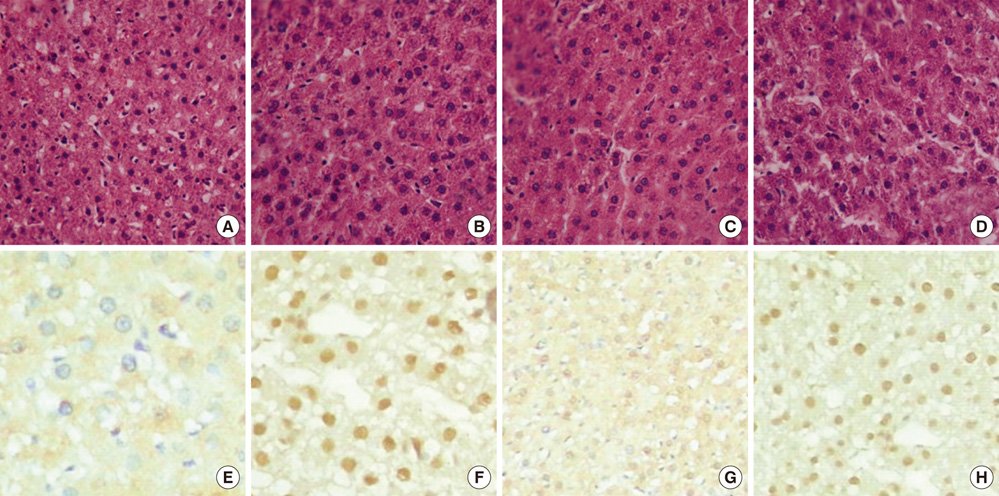
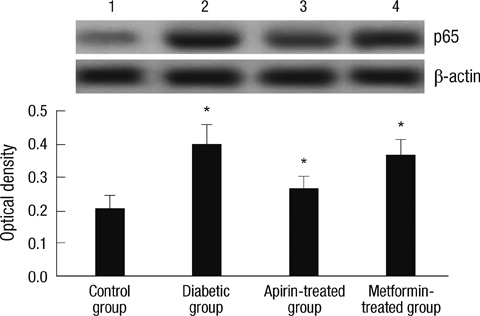
- Aspirin is a kind of anti-inflammatory drug and may be used to reverse hyperglycemia, hyperinsulinemia, and dyslipidemia by improving insulin resistance. We hypothesized that aspirin improves insulin resistance in type 2 diabetes by inhibiting hepatic nuclear factor kappa-beta (NF-kappaB) activation and serum tumor necrosis factor-alpha (TNF-alpha). Adult male Wistar rats were randomly divided into four groups: control, untreated diabetic, diabetic treated with metformin (100 mg/kg/day), and diabetic treated with aspirin (120 mg/kg/day). Diabetes was induced by high-fat feeding and a low dose of streptozotocin (30 mg/kg). After treatment, plasma glucose, insulin, lipids, free fatty acids (FFAs) concentrations and serum TNF-alpha were determined. The expression of NF-kappaB in hepatocytes was analyzed by immunohistochemistry and western blot. The results showed administration of aspirin caused no significant lowering in fasting glucose level but significant reduction of hepatic NF-kappaB expression and serum TNF-alpha level with improved insulin resistance compared to the diabetic group. The relevant analysis showed positive correlation between the expression of homeostasis model assessment-insulin resistance (HOMA-IR) and NF-kappaB (r = 0.799, P < 0.01); HOMA-IR and serum TNF-alpha (r = 0.790, P < 0.01). It is concluded that aspirin improves insulin resistance by inhibiting hepatic NF-kappaB activation and TNF-alpha level in streptozotocin-induced type 2 diabetic rats.
Keyword
MeSH Terms
-
Animals
Anti-Inflammatory Agents, Non-Steroidal/*pharmacology
Aspirin/*pharmacology
Blood Glucose/analysis
Diabetes Mellitus, Experimental/blood/chemically induced/*metabolism
Fatty Acids, Nonesterified/blood
Hypoglycemic Agents/*pharmacology
Insulin/blood
Insulin Resistance
Liver/metabolism
Male
Metformin/therapeutic use
NF-kappa B/*metabolism
Rats
Rats, Wistar
Tumor Necrosis Factor-alpha/*blood
Figure
Reference
-
1. Virally M, Blicklé JF, Girard J, Halimi S, Simon D, Guillausseau PJ. Type 2 diabetes mellitus: epidemiology, pathophysiology, unmet needs and therapeutical perspectives. Diabetes Metab. 2007. 33:231–244.2. Spellman CW. Pathophysiology of type 2 diabetes: targeting islet cell dysfunction. J Am Osteopath Assoc. 2010. 110:S2–S7.3. Hotamisligil GS. Inflammatory pathways and insulin action. Int J Obes Relat Metab Disord. 2003. 27:Suppl 3. S53–S55.4. Yuan M, Konstantopoulos N, Lee J, Hansen L, Li ZW, Karin M, Shoelson SE. Reversal of obesity- and diet-induced insulin resistance with salicylates or targeted disruption of IKK-β. Science. 2001. 293:1673–1677.5. Hundal RS, Petersen KF, Mayerson AB, Randhawa PS, Inzucchi S, Shoelson SE, Shulman GI. Mechanism by which high-dose aspirin improves glucose metabolism in type 2 diabetes. J Clin Invest. 2002. 109:1321–1326.6. Festa A, D'Agostino R Jr, Howard G, Mykkänen L, Tracy RP, Haffner SM. Chronic subclinical inflammation as part of the insulin resistance syndrome: the Insulin Resistance Atherosclerosis Study (IRAS). Circulation. 2000. 102:42–47.7. Vozarova B, Weyer C, Hanson K, Tataranni PA, Bogardus C, Pratley RE. Circulating interleukin-6 in relation to adiposity, insulin action, and insulin secretion. Obes Res. 2001. 9:414–417.8. Pankow JS, Duncan BB, Schmidt MI, Ballantyne CM, Couper DJ, Hoogeveen RC, Golden SH. Atherosclerosis Risk in Communities Study. Fasting plasma free fatty acids and risk of type 2 diabetes: the atherosclerosis risk in communities study. Diabetes Care. 2004. 27:77–82.9. Cai D, Yuan M, Frantz DF, Melendez PA, Hansen L, Lee J, Shoelson SE. Local and systemic insulin resistance resulting from hepatic activation of IKK-beta and NF-kappaB. Nat Med. 2005. 11:183–190.10. Arkan MC, Hevener AL, Greten FR, Maeda S, Li ZW, Long JM, Wynshaw-Boris A, Poli G, Olefsky J, Karin M. IKK-beta links inflammation to obesity-induced insulin resistance. Nat Med. 2005. 11:191–198.11. Wang HJ, Jin YX, Shen W, Neng J, Wu T, Li YJ, Fu ZW. Low dose streptozotocin (STZ) combined with high energy intake can effectively induce type 2 diabetes through altering the related gene expression. Asia Pac J Clin Nutr. 2007. 16:Suppl 1. 412–417.12. Abdin AA, Baalash AA, Hamooda HE. Effects of rosiglitazone and aspirin on experimental model of induced type 2 diabetes in rats: focus on insulin resistance and inflammatory markers. J Diabetes Complications. 2010. 24:168–178.13. Haffner SM, Greenberg AS, Weston WM, Chen H, Williams K, Freed MI. Effect of rosiglitazone treatment on nontraditional markers of cardiovascular disease in patients with type 2 diabetes mellitus. Circulation. 2002. 106:679–684.14. Laemmli UK. Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature. 1970. 227:680–685.15. Ceriello A, Motz E. Is oxidative stress the pathogenic mechanism underlying insulin resistance, diabetes, and cardiovascular disease? The common soil hypothesis revisited. Arterioscler Thromb Vasc Biol. 2004. 24:816–823.16. Pickup JC, Mattock MB, Chusney GD, Burt D. NIDDM as a disease of the innate immune system: association of acute-phase reactants and interleukin-6 with metabolic syndrome X. Diabetologia. 1997. 40:1286–1292.17. Park K, Steffes M, Lee DH, Himes JH, Jacobs DR Jr. Association of inflammation with worsening HOMA-insulin resistance. Diabetologia. 2009. 52:2337–2344.18. Olefsky JM, Glass CK. Macrophages, inflammation, and insulin resistance. Annu Rev Physiol. 2010. 72:219–246.19. Yang H, Youm YH, Vandanmagsar B, Ravussin A, Gimble JM, Greenway F, Stephens JM, Mynatt RL, Dixit VD. Obesity increases the production of proinflammatory mediators from adipose tissue T cells and compromises TCR repertoire diversity: implications for systemic inflammation and insulin resistance. J Immunol. 2010. 185:1836–1845.20. Nanes MS. Tumor necrosis factor-alpha: molecular and cellular mechanisms in skeletal pathology. Gene. 2003. 321:1–15.21. Yang J, Park Y, Zhang H, Xu X, Laine GA, Dellsperger KC, Zhang C. Feed-forward signaling of TNF-alpha and NF-kappaB via IKK-beta pathway contributes to insulin resistance and coronary arteriolar dysfunction in type 2 diabetic mice. Am J Physiol Heart Circ Physiol. 2009. 296:H1850–H1858.22. Soriano FG, Virág L, Szabó C. Diabetic endothelial dysfunction: role of reactive oxygen and nitrogen species production and poly (ADP-ribose) polymerase activation. J Mol Med. 2001. 79:437–448.23. Wunderlich FT, Luedde T, Singer S, Schmidt-Supprian M, Baumgartl J, Schirmacher P, Pasparakis M, Brüning JC. Hepatic NF-kappa B essential modulator deficiency prevents obesity-induced insulin resistance but synergizes with high-fat feeding in tumorigenesis. Proc Natl Acad Sci USA. 2008. 105:1297–1302.24. Kim JK, Kim YJ, Fillmore JJ, Chen Y, Moore I, Lee J, Yuan M, Li ZW, Karin M, Perret P, Shoelson SE, Shulman GI. Prevention of fat-induced insulin resistance by salicylate. J Clin Invest. 2001. 108:437–446.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Role of protein kinases on NF- kappaB activation and cell death in bovine cerebral endothelial cells
- The Role of NF-kappaB in the TNF-alpha-induced Apoptosis of Lung Cancer Cell Line
- Hyperglycemia-induced Activation of Nuclear Transcription Factor kappaB in Cultured Fibroblasts and Endothelial Cells
- Inhibition of TNF-alpha-Mediated NF-kappaB Transcriptional Activity by Dammarane-Type Ginsenosides from Steamed Flower Buds of Panax ginseng in HepG2 and SK-Hep1 Cells
- Nitric oxide prevents the bovine cerebral endothelial cell death induced by serum-deprivation