Neurointervention.
2011 Aug;6(2):84-88. 10.5469/neuroint.2011.6.2.84.
Direct Percutaneous Alcohol Sclerotherapy for Venous Malformations of Head and Neck Region without Fluoroscopic Guidance: Technical Consideration and Outcome
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiology, University of Ulsan, College of Medicine, Asan Medical Center, Seoul, Korea. dcsuh@amc.seoul.kr
- 2Department of Plastic Surgery, University of Ulsan, College of Medicine, Asan Medical Center, Seoul, Korea.
- KMID: 1783988
- DOI: http://doi.org/10.5469/neuroint.2011.6.2.84
Abstract
- PURPOSE
Alcohol is not used directly to the vascular lesion without mixing with the contrast agent because alcohol itself cannot be seen on the fluoroscopy. Since we have used alcohol for the venous malformations in the head and neck area, we realized that alcohol can be safely and effectively used without using fluoroscopy. We present the method of direct sclerotherapy using absolute alcohol without using fluoroscopy.
MATERIALS AND METHODS
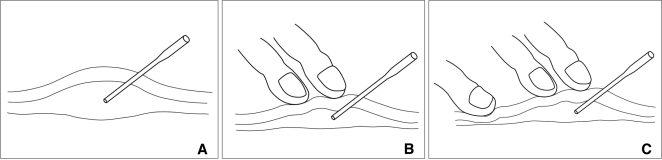
After obtaining and carefully analyzing direct puncture venogram, we used this technique in 22 patients who underwent alcohol sclerotherapy. Because fluoroscopy was not used during alcohol injection, the angiotable can be placed outside of C-arm so that alcohol was comfortably injected without any obstacle around the patients. Venogram can also be obtained between the injections to detect whether there is any dangerous venous outflow drainage such as the superior ophthalmic vein to the cavernous sinus. To control the venous outflow, local compression to the draining vein was applied. The result and complication such as skin necrosis, infection, and nerve injury were evaluated during mean follow-up period of 13 months (range, 1-63 months).
RESULTS
The frequency of sclerotherapy was one in 16 and 2-5 in 6 patients. The volume of alcohol used per treatment session ranged from 2 to 18 mL (mean, 8.5 mL). There was the minimum change in 1 (4.5%), moderately decreased lesion in 12 (54.5%), and markedly decreased lesion in 9 (41%) patients. The patients did not reveal any complications during 12.9 months follow-up period.
CONCLUSION
Direct puncture alcohol sclerotherapy without using fluoroscopy can be a safe and effective technique for treating venous malformation of the head and neck areas. In addition, the procedure can be performed in the comfortable position because biplane fluoroscopy would not be necessary.
MeSH Terms
Figure
Cited by 2 articles
-
Sclerotherapy for Venous Malformations of Head and Neck: Systematic Review and Meta-Analysis
Lucio De Maria, Paolo De Sanctis, Karthik Balakrishnan, Megha Tollefson, Waleed Brinjikji
Neurointervention. 2020;15(1):4-17. doi: 10.5469/neuroint.2019.00213.Visualization of Soft Tissue Venous Malformations of Head and Neck with 4D Flow Magnetic Resonance Imaging
Ji Ye Lee, Dae Chul Suh
Neurointervention. 2017;12(2):110-115. doi: 10.5469/neuroint.2017.12.2.110.
Reference
-
1. Johnson PL, Eckard DA, Brecheisen MA, Girod DA, Tsue TT. Percutaneous ethanol sclerotherapy of venous malformations of the tongue. AJNR Am J Neuroradiol. 2002; 23:779–782. PMID: 12006276.2. Spence J, Krings T, terBrugge K, da Costa L, Agid R. Percutaneous sclerotherapy for facial venous malformations: subjective clinical and objective MR imaging follow-up results. AJNR Am J Neuroradiol. 2010; 31:955–960. PMID: 20044505.
Article3. Legiehn GM, Heran MKS. Venous malformations: classification, development, diagnosis, and interventional radiologic management. Radiol Clin North Am. 2008; 46:545–597. PMID: 18707962.
Article4. Do YS, Yakes WF, Shin SW, Lee BB, Kim DI, Liu WC, et al. Ethanol embolization of arteriovenous malformations: interim results. Radiology. 2005; 235:674–682. PMID: 15858106.
Article5. Lee HY, Kim SM, Choi JW, In HS, Jang YJ, Cho KJ, et al. The Significance of immunohistochemical staining, including that for glucose transporter protein isoform 1, as related to the clinical and angiographic features of adult soft-tissue hemangioma and arteriovenous malformation in the head and neck. J Korean Soc Radiol. 2009; 60:83–91.
Article6. Yakes W, Luethke J, Parker S, Stavros A, Rak K, Hopper K, et al. Ethanol embolization of vascular malformations. Radiographics. 1990; 10:787–796. PMID: 2217971.
Article7. Berenguer B, Burrows PE, Zurakowski D, Mulliken JB. Sclerotherapy of craniofacial venous malformations: complications and results. Plast Reconstr Surg. 1999; 104:1–11. PMID: 10597669.
Article8. Mason KP, Michna E, Zurakowski D, Koka BV, Burrows PE. Serum ethanol levels in children and adults after ethanol embolization or sclerotherapy for vascular anomalies. Radiology. 2000; 217:127–132. PMID: 11012433.
Article9. Yakes W, Haas D, Parker S, Gibson M, Hopper K, Mulligan J, et al. Symptomatic vascular malformations: ethanol embolotherapy. Radiology. 1989; 170:1059–1066. PMID: 2916057.
Article10. Hammer FD, Boon LM, Mathurin P, Vanwijck RR. Ethanol sclerotherapy of venous malformations: evaluation of systemic ethanol contamination. J Vasc Interv Radiol. 2001; 12:595–600. PMID: 11340138.
Article11. Fan X, Su L, Zheng J, Zheng L, Zhang Z. Ethanol embolization of arteriovenous malformations of the mandible. AJNR Am J Neuroradiol. 2009; 30:1178–1183. PMID: 19270102.
Article12. Goyal M, Causer PA, Armstrong D. Venous vascular malformations in pediatric patients: comparison of results of alcohol sclerotherapy with proposed MR imaging classification. Radiology. 2002; 223:639–644. PMID: 12034929.
Article13. Ryu C, Whang S, Suh D, Kim SM, Jang YJ, Kim HJ, et al. Percutaneous direct puncture glue embolization of high-flow craniofacial arteriovenous lesions: a new circular ring compression device with a beveled edge. AJNR Am J Neuroradiol. 2007; 28:528–530. PMID: 17353329.14. Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg. 1982; 69:412–422. PMID: 7063565.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Venous Malformation of the Pyriform Sinus Treated with Ethanol Sclerotherapy
- Clicically improved venous malformation by sclerotherapy
- Visualization of Soft Tissue Venous Malformations of Head and Neck with 4D Flow Magnetic Resonance Imaging
- Sclerotherapy for Venous Malformations of Head and Neck: Systematic Review and Meta-Analysis
- Efficacy of Percutaneous Sclerotherapy in Low Flow Venous Malformations - A Single Center Series