Neurointervention.
2017 Sep;12(2):110-115. 10.5469/neuroint.2017.12.2.110.
Visualization of Soft Tissue Venous Malformations of Head and Neck with 4D Flow Magnetic Resonance Imaging
- Affiliations
-
- 1Department of Radiology, Soonchunhyang University Bucheon Hospital, Bucheon, Korea.
- 2Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea. dcsuh@amc.seoul.kr
- KMID: 2389503
- DOI: http://doi.org/10.5469/neuroint.2017.12.2.110
Abstract
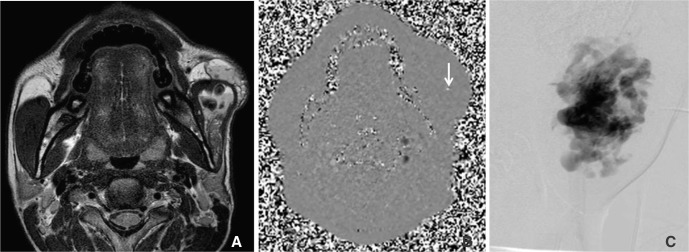
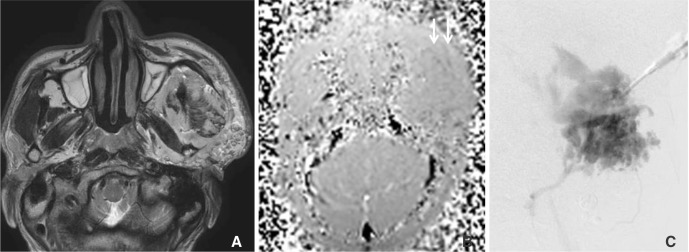
- Evaluation of hemodynamics in venous malformation (VM) in the head and neck area is done by direct puncture venography before alcohol sclerotherapy, but it is difficult due to a variable degree of filling in from the artery and filling out into the draining vein. We present our preliminary experience of 4D MRI to evaluate VM hemodynamics. Four patients with venous malformation in the maxillofacial area underwent both 4D MRI and direct puncture venography before alcohol sclerotherapy. To find out appropriate velocity encoding (VENC) for VM, we applied 5-50 cm/sec VENC. Significant high-flow foci demonstrated by phase changes in magnitude images were compared with lesion types shown on a direct puncture venogram. Detection of flow in VM was possible in magnitude images or phase-difference images when VENC was set to less than 30 cm/sec. Appropriate VENC for VM was regarded as less than 5 cm/sec. High-flow areas in the dilated venous sac demonstrated focal spots or linear band-like areas on phase changes of 4D MRI. Appropriate VENC application was mandatory to detect flow in VM. Flow information on 4D MRI provided flow information in VM which was not detected on a direct puncture venogram in the compartmentalized lesion and thus can make alcohol sclerotherapy safer.
MeSH Terms
Figure
Reference
-
1. Legiehn GM, Heran MKS. Venous malformations: classification, development, diagnosis, and interventional radiologic management. Radiol Clin North Am. 2008; 46:545–597. PMID: 18707962.
Article2. Do YS, Yakes WF, Shin SW, Lee BB, Kim DI, Liu WC, et al. Ethanol embolization of arteriovenous malformations: interim results. Radiology. 2005; 235:674–682. PMID: 15858106.
Article3. Ryu CW, Kim JK, Kim SJ, Lee JH, Kim JH, Ha HI, et al. Head and neck vascular lesions: characterization of the flow pattern by the use of three-phase CT. Korean J Radiol. 2009; 10:323–332. PMID: 19568459.
Article4. Lee HY, Kim SM, Choi JW, In HS, Cho KJ, Cha EY, et al. The Significance of immunohistochemical staining, including that for glucose transporter protein isoform 1, as related to the clinical and angiographic features of adult soft-tissue hemangioma and arteriovenous malformation in the head and neck. J Korean Soc Radiol. 2009; 60:83–91.
Article5. Yakes WF, Luethke JM, Parker SH, Stavros AT, Rak KM, Hopper KD, et al. Ethanol embolization of vascular malformations. Radiographics. 1990; 10:787–796. PMID: 2217971.
Article6. Berenguer B, Burrows PE, Zurakowski D, Mulliken JB. Sclerotherapy of craniofacial venous malformations: complications and results. Plast Reconstr Surg. 1999; 104:1–11. PMID: 10597669.
Article7. Mason KP, Michna E, Zurakowski D, Koka BV, Burrows PE. Serum ethanol levels in children and adults after ethanol embolization or sclerotherapy for vascular anomalies. Radiology. 2000; 217:127–132. PMID: 11012433.
Article8. Baek HJ, Hong JP, Choi JW, Suh DC. Direct percutaneous alcohol sclerotherapy for venous malformations of head and neck region without fluoroscopic guidance: technical consideration and outcome. Neurointervention. 2011; 6:84–88. PMID: 22125754.
Article9. Moukaddam H, Pollak J, Haims AH. MRI characteristics and classification of peripheral vascular malformations and tumors. Skeletal Radiol. 2009; 38:535–547. PMID: 19020874.
Article10. Ryu CW, Whang SM, Suh DC, Kim SM, Jang YJ, Kim HJ, et al. Percutaneous direct puncture glue embolization of high-flow craniofacial arteriovenous lesions: a new circular ring compression device with a beveled edge. AJNR Am J Neuroradiol. 2007; 28:528–530. PMID: 17353329.11. Hope TA, Zarins CK, Herfkens RJ. Initial experience characterizing a type I endoleak from velocity profiles using time-resolved three-dimensional phase-contrast MRI. J Vasc Surg. 2009; 49:1580–1584. PMID: 19223146.
Article12. Dubois J, Soulez G, Oliva VL, Berthiaume MJ, Lapierre C, Therasse E. Soft-tissue venous malformations in adult patients: imaging and therapeutic issues. Radiographics. 2001; 21:1519–1531. PMID: 11706222.
Article13. Dubois JM, Sebag GH, De Prost Y, Teillac D, Chretien B, Brunelle FO. Soft-tissue venous malformations in children: percutaneous sclerotherapy with Ethibloc. Radiology. 1991; 180:195–198. PMID: 2052693.
Article14. Jackson IT, Carreno R, Potparñic Z, Hussain K. Hemangiomas, vascular malformations, and lymphovenous malformations: classification and methods of treatment. Plast Reconstr Surg. 1993; 91:1216–1230. PMID: 8497521.15. Burrows PE, Mulliken JB, Fellows KE, Strand RD. Childhood hemangiomas and vascular malformations: angiographic differentiation. AJR Am J Roentgenol. 1983; 141:483–488. PMID: 6603756.
Article16. Trop I, Dubois J, Guibaud L, Grignon A, Patriquin H, McCuaig C, et al. Soft-tissue venous malformations in pediatric and young adult patients: diagnosis with Doppler US. Radiology. 1999; 212:841–845. PMID: 10478255.
Article17. Fordham LA, Chung CJ, Donnelly LF. Imaging of congenital vascular and lymphatic anomalies of the head and neck. Neuroimaging Clin N Am. 2000; 10:117–136. PMID: 10658158.18. Ziyeh S, Schumacher M, Strecker R, R¨ossler J, Hochmuth A, Klisch J. Head and neck vascular malformations: time-resolved MR projection angiography. Neuroradiology. 2003; 45:681–686. PMID: 12942216.
Article19. Dobson M, Hartley R, Ashleigh R, Watson Y, Hawnaur J. MR angiography and MR imaging of symptomatic vascular malformations. Clinical Radiology. 1997; 52:595–602. PMID: 9285419.
Article20. van Rijswijk CS, van der Linden E, van der Woude HJ, van Baalen JM, Bloem JL. Value of dynamic contrast-enhanced MR imaging in diagnosing and classifying peripheral vascular malformations. AJR Am J Roentgenol. 2002; 178:1181–1187. PMID: 11959728.
Article21. Lee BB, Kim DI, Huh S, Kim HH, Choo IW, Byun HS, et al. New experiences with absolute ethanol sclerotherapy in the management of a complex form of congenital venous malformation. J Vasc Surg. 2001; 33:764–772. PMID: 11296330.
Article22. Kim YH, Choi JY, Kim YW, Kim DI, Do YS, Hwang JH, et al. Characterization of congenital vascular malformation in the extremities using whole body blood pool scintigraphy and lymphscintigraphy. Lymphology. 2009; 42:77–84. PMID: 19725272.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Four-Dimensional Flow Magnetic Resonance Imaging for Cardiovascular Imaging: from Basic Concept to Clinical Application
- Cerebellar Venous Angioma Confused with Peripheral Vestibulopathy
- Efficacy of Percutaneous Sclerotherapy in Low Flow Venous Malformations - A Single Center Series
- Demonstration of Turbulence at the Site of Ascending Aorta Graft Kinking Using 4-Dimensional Flow Magnetic Resonance Imaging
- Upper Extremity Hemolymphangiomas in Children: A Case Report