Korean J Obstet Gynecol.
2012 Jun;55(6):424-428. 10.5468/KJOG.2012.55.6.424.
A case of primary retroperitoneal mucinous cystadenocarcinoma treated with fertility-sparing surgery
- Affiliations
-
- 1Department of Pathology, Gachon University Gil Medical Center, Incheon, Korea.
- 2Department of Obstetrics and Gynecology, Gachon University Gil Medical Center, Incheon, Korea. miracle627@gilhospital.com
- KMID: 1783937
- DOI: http://doi.org/10.5468/KJOG.2012.55.6.424
Abstract
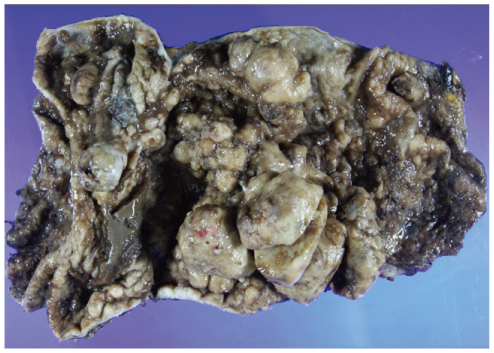
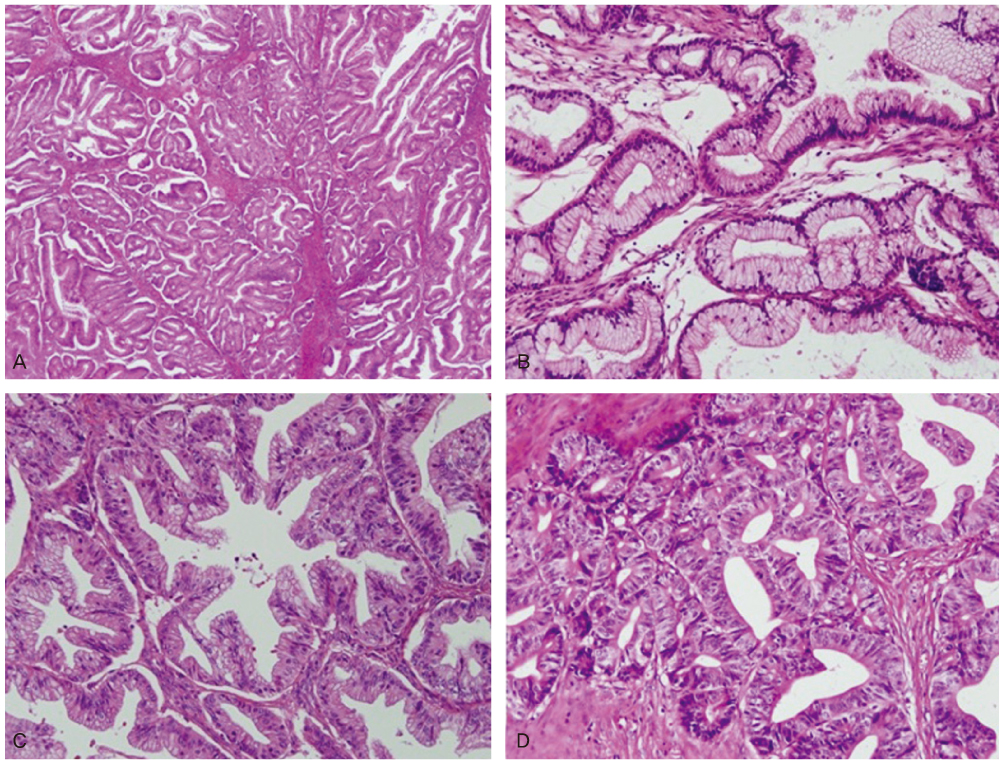
- Primary retroperitoneal mucinous cystadenocarcinoma is an extremely rare tumor. Preoperative diagnosis is very difficult and the treatment remains controversial. A 37-year-old Korean woman (gravida 0) presented with a huge abdominal mass. Computed tomography scan revealed an 18 x 11 cm sized unilocular cyst with irregular wall thickening and solid component at right adnexa. Serum CA 19-9 was slightly elevated (37.05 U/mL). At laparotomy, a huge right retroperitoneal cystic tumor originating from right paracolic gutter was found. Frozen section of the cystic tumor revealed a mucinous cystadenocarcinoma. Because the patient wished to remain fertile, fertility sparing surgery was performed. Microscopically, no evidence of metastasis was found and no further treatment was given. Six months after surgery, she has no evidence of recurrence. Fertility-sparing surgery should be considered for women with primary retroperitoneal mucinous cystadenocarcinoma, who wish to remain fertile.
MeSH Terms
Figure
Reference
-
1. Kanayama T, Yoshino K, Enomoto T, Ohashi H, Fujita M, Ueda Y, et al. Primary retroperitoneal mucinous cystadenocarcinoma with mural nodules: a case report and literature review. Int J Clin Oncol. 2011. 09. 17. [Epub]. DOI: 10.1007/s10147-011-0313-4.2. Law KS, Chang TM, Tung JN. Fertility-sparing treatment of a primary retroperitoneal mucinous cystadenocarcinoma. BJOG. 2006. 113:612–614.3. Roth LM, Ehrlich CE. Mucinous cystadenocarcinoma of the retroperitoneum. Obstet Gynecol. 1977. 49:486–488.4. Storch MP, Raghavan U. Mucinous cystadenocarcinoma of retroperitoneum. Conn Med. 1980. 44:140–141.5. Peterson WF. Malignant degeneration of benign cystic teratomas of the overy: a collective review of the literature. Obstet Gynecol Surv. 1957. 12:793–830.6. Chen JS, Lee WJ, Chang YJ, Wu MZ, Chiu KM. Laparoscopic resection of a primary retroperitoneal mucinous cystadenoma: report of a case. Surg Today. 1998. 28:343–345.7. Matsubara M, Shiozawa T, Tachibana R, Hondo T, Osasda K, Kawaguchi K, et al. Primary retroperitoneal mucinous cystadenoma of borderline malignancy: a case report and review of the literature. Int J Gynecol Pathol. 2005. 24:218–223.8. Guioli S, Sekido R, Lovell-Badge R. The origin of the Mullerian duct in chick and mouse. Dev Biol. 2007. 302:389–398.9. Yang DM, Jung DH, Kim H, Kang JH, Kim SH, Kim JH, et al. Retroperitoneal cystic masses: CT, clinical, and pathologic findings and literature review. Radiographics. 2004. 24:1353–1365.10. Tenti P, Carnevali L, Tateo S, Durola R. Primary mucinous cystoadenocarcinoma of the retroperitoneum: two cases. Gynecol Oncol. 1994. 55:308–312.11. Tangjitgamol S, Manusirivithaya S, Sheanakul C, Leelahakorn S, Thawaramara T, Kaewpila N. Retroperitoneal mucinous cystadenocarcinoma: a case report and review of literature. Int J Gynecol Cancer. 2002. 12:403–408.12. Satoh T, Hatae M, Watanabe Y, Yaegashi N, Ishiko O, Kodama S, et al. Outcomes of fertility-sparing surgery for stage I epithelial ovarian cancer: a proposal for patient selection. J Clin Oncol. 2010. 28:1727–1732.13. Suzuki S, Mishina T, Ishizuka D, Fukase M, Matsubara YI. Mucinous cystadenocarcinoma of the retroperitoneum: report of a case. Surg Today. 2001. 31:747–750.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary Retroperitoneal Mucinous Cystadenocarcioma Involving the Splenic Hilum
- MR Imaging of Primary Retroperitoneal Mucinous Cystadenocarcinoma in Pregnant Woman
- Primary Retroperitoneal Mucinous Cystadenocarcinoma: A Case Report and Review of the Literature
- Mucinous cystadenocarcinoma of ovary with metastasis in 14-year-old girl
- A case of mucinous adenocarcinoma arising from retroperitoneal teratoma treated with chemoradiation