Korean J Lab Med.
2007 Oct;27(5):369-372. 10.3343/kjlm.2007.27.5.369.
A RhD Negative Patient Failed to Produce Detectable Anti-D after Transfusion of 35 Units of RhD Positive Red Blood Cells
- Affiliations
-
- 1Department of Laboratory Medicine, School of Medicine, Keimyung University, Daegu, Korea. lwm@dsmc.or.kr
- 2Department of Laboratory Medicine, Chonnam National University Medical School, Gwangju, Korea.
- KMID: 1781537
- DOI: http://doi.org/10.3343/kjlm.2007.27.5.369
Abstract
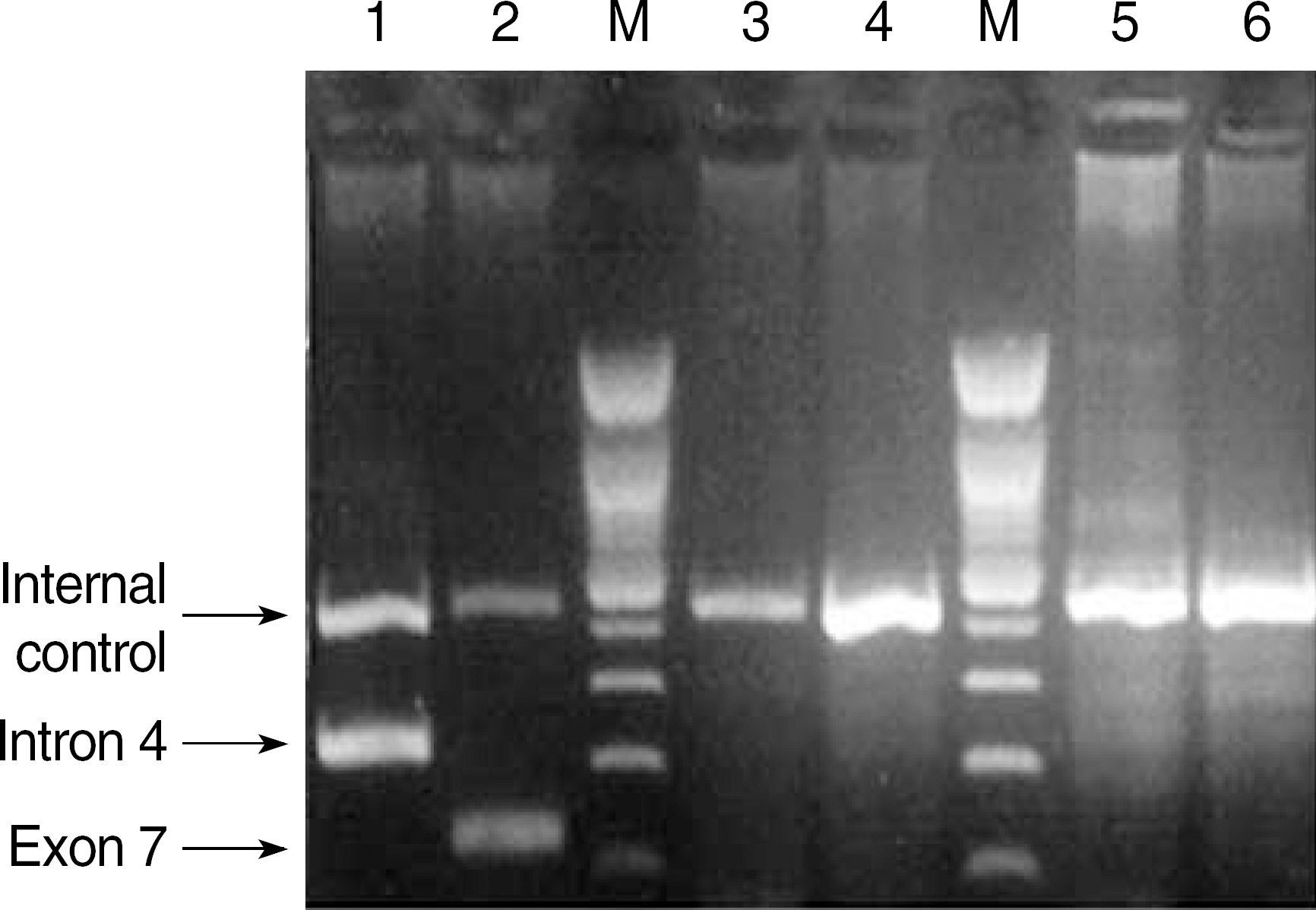
- In the present day, pretransfusion tests include ABO and RhD grouping, antibody screening, antibody identification, and cross matching. Although error rates for these tests have decreased compared to those in the past, clerical errors still occur. When exposed to RhD positive RBCs, a RhD negative person can produce anti-D that causes a severe hemolytic disease of the fetus and the newborn in addition to hemolytic transfusion reactions. Therefore, administration of RhD positive RBCs to a RhD negative person should be avoided. We experienced a RhD negative patient who had been misidentified as positive and transfused 35 units of RhD positive RBCs eight years ago, but did not have detectable anti-D in present. The red cells of the patient showed no agglutination with the anti-D reagent and a negative result in the standard weak D test. The multiplex PCR with sequence-specific priming revealed that the patient was RhD negative.
Keyword
MeSH Terms
Figure
Reference
-
1.Han KS, Park MH, editors. Transfusion Medicine. 3rd ed.Seoul: Korea medical Publishing Co;2006. p. 214–9. (한규섭, 박명희등. 수혈의학. 제3판. 서울: 고려의학 2006 214-9).2.Brecher ME, editor. Technical manual. 15th ed.Bethesda: American Association of Blood Banks;2005. p. 315–33.3.Hwang YS. Haplotype frequencies of Rh gene loci in Koreans. Korean J Blood Transfus. 1996. 7:233–40. (황유성. 한국인 Rh혈액형의 유전자일배체형분석. 대한수혈학회지 1996;7: 233-40.).4.Frohn C., Dumbgen L., Brand JM., Gorg S., Luhm J., Kirchner H. Probability of anti-D development in D- patients receiving D+ RBCs. Transfusion. 2003. 43:893–8.
Article5.Boctor FN., Ali NM., Mohandas K., Uehlinger J. Absence of D- alloimmunization in AIDS patients receiving D-mismatched RBCs. Transfusion. 2003. 43:173–6.
Article6.Casanueva M., Valdes MD., Ribera MC. Lack of alloimmunization to D antigen in D-negative immunosuppressed liver transplant recipients. Transfusion. 1994. 34:570–2.
Article7.Kim JY., Kim SY., Kim CA., Yon GS., Park SS. Molecular characterization of D- Korean persons: development of a diagnostic strategy. Transfusion. 2005. 45:345–52.
Article8.Luettringhaus TA., Cho D., Ryang DW., Flegel WA. An easy RHD genotyping strategy for D negative East Asian persons applied to Korean blood donors. Transfusion. 2006. 46:2128–37.9.Lin M. Taiwan experience suggests that RhD typing for blood transfusion in unnecessary in southeast Asian populations. Transfusion. 2006. 46:95–8.10.Hensler T., Hecker H., Heeg K., Heidecke CD., Bartels H., Barthlen W, et al. Distinct mechanisms of immunosuppression as a consequence of major surgery. Infect Immun. 1997. 65:2283–91.
Article11.Urbaniak SJ., Robertson AE. A successful program of immunizing Rh-negative male volunteers for anti-D production using frozen/thawed blood. Transfusion. 1981. 21:64–9.12.Jakobowicz R., Williams L., Silberman F. Immunization of Rh-negative volunteers by repeated injections of very small amounts of Rh-positive blood. Vox Sang. 1972. 23:376–81.
Article13.Menitove JE. Immunoprophylaxis for D-patients receiving platelet transfusions from D+ donors? Transfusion. 2002. 42:136–8.14.Pack JY., Cho D., Choi HW., Jeon MJ., Park MS., Song JW, et al. A patient with RhDel (1227G>A) failed to produce detectable anti-D after transfusion of RhD positive red blood cells. Korean J Blood Transfus. 2006. 17:153–8. (박지영, 조덕, 최현우. 전미정, 박만석, 송정원등. RhD 양성농축적혈구투여후 Anti-D가검출되지않은RhDel (1227G>A) 1예. 대한수혈학회지 2006;17: 153-8.).15.Knowles SM., Milkins CE., Chapman JF., Scott M. The United Kingdom National External Quality Assessment Scheme (Blood Transfusion Laboratory Practice): trends in proficiency and practice between 1985 and 2000. Transfus Med. 2002. 12:11–23.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Patient with RhD(el) (1227G>A) Failed to Produce Detectable Anti-D after Transfusion of RhD Positive Red Blood Cells
- Transfusion of RhD-Positive Blood Components to Serologic RhD-Negative Patients-Review of Current Literature: An Opinion
- Transfusion of RhD-Positive Blood Products to Asia Type DEL Patients: A Report of Two Cases
- Transfusion in RhD Mismatch Hematopoietic Stem Cell Transplantation
- A Case of Primary Anti-D Alloimmunization by RHD (c.1227G>A) DEL Red Blood Cell Transfusion