J Korean Med Sci.
2009 Jun;24(3):420-426. 10.3346/jkms.2009.24.3.420.
Acute Physiology and Chronic Health Evaluation II and Simplified Acute Physiology Score II in Predicting Hospital Mortality of Neurosurgical Intensive Care Unit Patients
- Affiliations
-
- 1Department of Neurosurgery, Ajou University Hospital, Suwon, Korea.
- 2Department of Neurosurgery, Hanyang University Medical Center, Seoul, Korea. hjyi8499@hanyang.ac.kr
- 3Department of Anesthesia and Pain Medicine, Hanyang University Medical Center, Seoul, Korea.
- 4Department of Emergency Medicine, Hanyang University Medical Center, Seoul, Korea.
- KMID: 1779157
- DOI: http://doi.org/10.3346/jkms.2009.24.3.420
Abstract
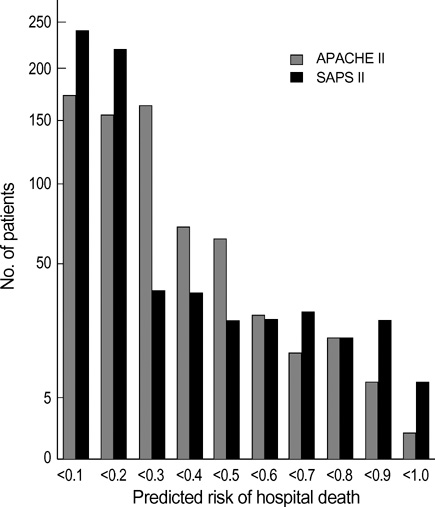
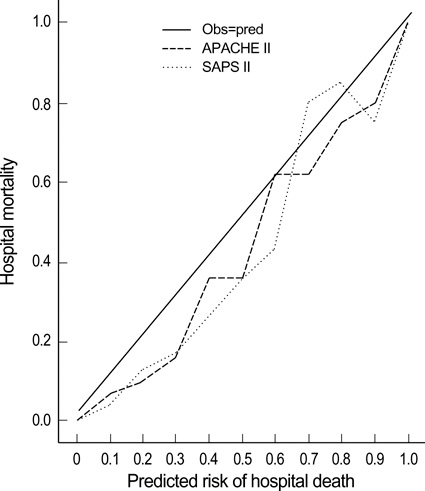
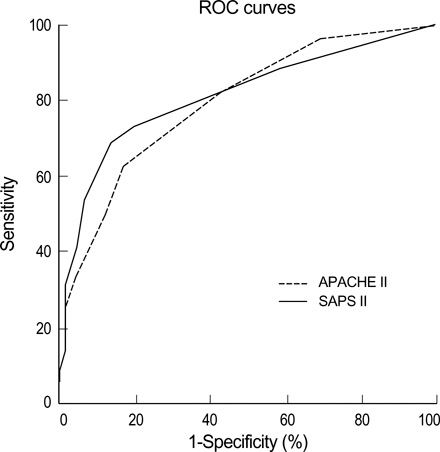
- We study the predictive power of Acute Physiology and Chronic Health Evaluation II (APACHE II) and Simplified Acute Physiology Score II (SAPS II) in neurosurgical intensive care unit (ICU) patients. Retrospective investigation was conducted on 672 consecutive ICU patients during the last 2 yr. Data were collected during the first 24 hours of admission and analyzed to calculate predicted mortality. Mortality predicted by two systems was compared and, multivariate analyses were then performed for subarachnoid hemorrhage (SAH) and traumatic brain injury (TBI) patients. Observed mortality was 24.8% whereas predicted mortalities were 37.7% and 38.4%, according to APACHE II and SAPS II. Calibration curve was close to the line of perfect prediction. SAPS II was not statistically significant according to a Lemeshow-Hosmer test, but slightly favored by area under the curve (AUC). In SAH patients, SAPS II was an independent predictor for mortality. In TBI patients, both systems had independent prognostic implications. Scoring systems are useful in predicting mortality and measuring performance in neurosurgical ICU setting. TBI patients are more affected by systemic insults than SAH patients, and this discrepancy of predicting mortality in each neurosurgical disease prompts us to develop a more specific scoring system targeted to cerebral dysfunction.
Keyword
MeSH Terms
-
*APACHE
Adolescent
Adult
Aged
Aged, 80 and over
Area Under Curve
Brain Injuries/diagnosis/*mortality/surgery
Child, Preschool
Female
*Hospital Mortality
Humans
*Intensive Care Units
Male
Middle Aged
Multivariate Analysis
Predictive Value of Tests
ROC Curve
Retrospective Studies
Severity of Illness Index
Subarachnoid Hemorrhage/diagnosis/*mortality/surgery
Time Factors
Figure
Reference
-
1. Rapoport J, Teres D, Lemeshow S, Gehlbach S. A method for assessing the clinical performance and cost-effectiveness of intensive care units: a multicenter inception cohort study. Crit Care Med. 1994. 22:1385–1391.2. Rowan KM, Kerr JH, Major E, McPherson K, Short A, Vessey MP. Intensive Care Society's Acute Physiology and Chronic Health Evaluation (APACHE II) study in Britain and Ireland: a prospective, multicenter, cohort study comparing two methods for predicting outcome for adult intensive care patients. Crit Care Med. 1994. 22:1392–1401.3. Zimmerman JE, Shortell SM, Knaus WA, Rousseau DM, Wagner DP, Gillies RR, Draper EA, Devers K. Value and cost of teaching hospitals: a prospective, multicenter, inception cohort study. Crit Care Med. 1993. 21:1432–1442.4. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985. 13:818–829.5. Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993. 270:2957–2963.
Article6. Lemeshow S, Teres D, Pastides H, Avrunin JS, Steingrub JS. A method for predicting survival and mortality of ICU patients using objectively derived weights. Crit Care Med. 1985. 13:519–525.
Article7. Pittet D, Thievent B, Wenzel RP, Li N, Gurman G, Suter PM. Importance of pre-existing co-morbidities for prognosis of septicemia in critically ill patients. Intensive Care Med. 1993. 19:265–272.
Article8. Brown MC, Crede WB. Predictive ability of acute physiology and chronic health evaluation II scoring applied to human immunodeficiency virus-positive patients. Crit Care Med. 1995. 23:848–853.
Article9. Smith RL, Levine SM, Lewis ML. Prognosis of patients with AIDS requiring intensive care. Chest. 1989. 96:857–861.
Article10. Chu DY. Predicting survival in AIDS patients with respiratory failure. Application of the APACHE II scoring system. Crit Care Clin. 1993. 9:89–105.
Article11. Pierpont GL, Parenti CM. Physician risk assessment and APACHE scores in cardiac care units. Clin Cardiol. 1999. 22:366–368.
Article12. Blot F, Guiguet M, Nitenberg G, Leclercq B, Gachot B, Escudier B. Prognostic factors for neutropenic patients in an intensive care unit: respective roles of underlying malignancies and acute organ failures. Eur J Cancer. 1997. 33:1031–1037.
Article13. Headley J, Theriault R, Smith TL. Independent validation of APACHE II severity of illness score for predicting mortality in patients with breast cancer admitted to the intensive care unit. Cancer. 1992. 70:497–503.
Article14. Cho DY, Wang YC. Comparison of the APACHE II, APACHE III and Glasgow Coma Scale in acute head injury for prediction of mortality and functional outcome. Intensive Care Med. 1997. 23:77–84.15. Murthy JM, Meena AK, Kumar SR. Severity-of-illness scoring systems and models: neurological and neurosurgical intensive care units. Neurol India. 2001. 49:Supple 1. S91–S94.16. Schuiling WJ, de Weerd AW, Dennesen PJ, Algra A, Rinkel GJ. The simplified acute physiology score to predict outcome in patients with subarachnoid hemorrhage. Neurosurgery. 2005. 57:230–236.
Article17. Goldhill DR, Sumner A. Outcome of intensive care patients in a group of British intensive care units. Crit Care Med. 1998. 26:1337–1345.
Article18. Lemeshow S, Hosmer DW Jr. A review of goodness of fit statistics for use in the development of logistic regression models. Am J Epidemiol. 1982. 115:92–106.19. Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982. 143:29–36.
Article20. Zimmerman JE, Shortell SM, Rousseau DM, Duffy J, Gillies RR, Knaus WA, Devers K, Wagner DP, Draper EA. Improving intensive care: observations based on organizational case studies in nine intensive care units: a prospective, multicenter study. Crit Care Med. 1993. 21:1443–1451.21. el-Solh AA, Grant BJ. A comparison of severity of illness scoring systems for critically ill obstetric patients. Chest. 1996. 110:1299–1304.22. Moreau R, Soupison T, Vauquelin P, Derrida S, Beaucour H, Sicot C. Comparison of two simplified severity scores (SAPS and APACHE II) for patients with acute myocardial infarction. Crit Care Med. 1989. 17:409–413.
Article23. Schuster HP, Schuster FP, Ritschel P, Wilts S, Bodmann KF. The ability of the Simplified Acute Physiology Score (SAPS II) to predict outcome in coronary care patients. Intensive Care Med. 1997. 23:1056–1061.
Article24. Yi HJ, Kim YS, Ko Y, Oh SJ, Kim KM, Oh SH. Factors associated with survival and neurological outcome after cardiopulmonary resuscitation of neurosurgical intensive care unit. Neurosurgery. 2006. 59:838–845.25. Gruber A, Reinprecht A, Illievich UM, Fitzgerald R, Dietrich W, Czech T, Richling B. Extracerebral organ dysfunction and neurologic outcome after aneurysmal subarachnoid hemorrhage. Crit Care Med. 1999. 27:505–514.
Article26. Solenski NJ, Haley EC, Kassell NF, Kongable G, Germanson T, Truskowski L, Torner JC. Medical complications of aneurysmal subarachnoid hemorrhage: a report of the multicenter, cooperative aneurysm study. Crit Care Med. 1995. 23:1007–1017.27. Claassen J, Vu A, Kreiter KT, Kowalski RG, Du EY, Ostapkovich N, Fitzsimmons BF, Connolly ES, Mayer SA. Effect of acute physiologic derangements on outcome after subarachnoid hemorrhage. Crit Care Med. 2004. 32:832–838.
Article28. Vassar MJ, Wilkerson CL, Duran PJ, Perry CA, Holcroft JW. Comparison of APACHE II, TRISS, and a proposed 24-hour ICU point system for prediction of outcome in ICU trauma patients. J Trauma. 1992. 32:490–499.
Article29. Cowen JS, Kelley MA. Errors and bias in using predictive scoring systems. Crit Care Clin. 1994. 10:53–72.
Article30. Tunnell RD, Millar BW, Smith GB. The effect of lead time bias on severity of illness scoring, mortality prediction and standardised mortality ratio in intensive care-a pilot study. Anaesthesia. 1998. 53:1045–1053.31. Sarmiento J, Torres A, Guardiola JJ, Milla J, Nadal P, Rozman C. Statistical modeling of prognostic indices for evaluation of critically ill patients. Crit Care Med. 1991. 19:867–870.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Validation of the APACHE IV model and its comparison with the APACHE II, SAPS 3, and Korean SAPS 3 models for the prediction of hospital mortality in a Korean surgical intensive care unit
- APACHE II Score and Evaluation of Intensive Care Unit Patients
- Comparison of Predict Mortality Scoring Systems for Spontaneous Intracerebral Hemorrhage Patients
- Comparison of mNUTRIC-S2 and mNUTRIC scores to assess nutritional risk and predict intensive care unit mortality
- Performance of APACHE IV in Medical Intensive Care Unit Patients: Comparisons with APACHE II, SAPS 3, and MPMâ‚€ III