J Korean Med Sci.
2007 Jun;22(3):580-582. 10.3346/jkms.2007.22.3.580.
Intramuscular Hemangioma Mimicking Myofascial Pain Syndrome: A Case Report
- Affiliations
-
- 1Department of Physical Medicine & Rehabilitation, Korea University Ansan Hospital, 516 Gojan-dong, Danwon-gu, Ansan, Korea. rmkdh@korea.ac.kr
- KMID: 1778377
- DOI: http://doi.org/10.3346/jkms.2007.22.3.580
Abstract
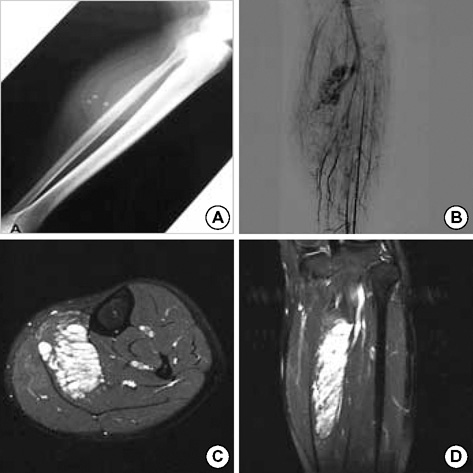
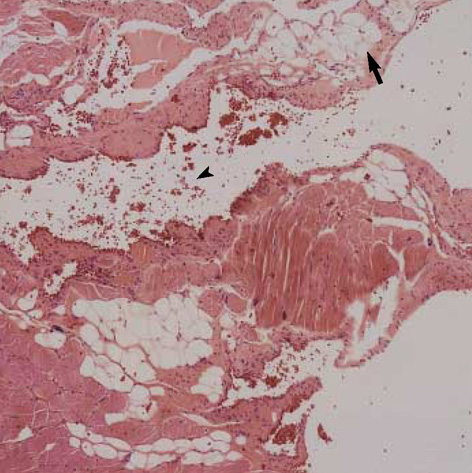
- Intramuscular hemangioma, an infrequent but important cause of musculoskeletal pain, is often difficult to establish the diagnosis clinically. This report describes a case of a 32-yr-old woman who presented with severe left calf pain for 10 yr. Initial conservative treatments consisting of intramuscular electrical stimulation, herb medication, acupuncture, and intramuscular lidocaine injection under the diagnosis of myofascial pain syndrome in other facilities, failed to alleviate the symptoms. On physical examination, there was no motor weakness or sensory change. Conventional radiography of the leg revealed a soft tissue phlebolith. Conventional angiography study showed hemangioma. Intramuscular hemangioma within the soleus muscle was confirmed by magnetic resonance imaging. Following surgical excision of the hemangioma, the patient's symptom resolved completely. Intramuscular hemangioma is a rare cause of calf pain and should be considered in the differential diagnosis if a patient with muscle pain, particularly if associated with a soft tissue mass, fails to respond to conservative treatment.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Hybrid Operation for Arteriovenous Malformation in Left Soleus Muscle with Embolization of Feeding Artery and En Bloc Resection: A Case Report
Dong-Il Chun, Seong-Min Kim, Sangchul Yun, Yong Jae Kim, Dong Erk Goo, In Ho Choi
J Korean Foot Ankle Soc. 2015;19(1):23-26. doi: 10.14193/jkfas.2015.19.1.23.
Reference
-
1. Prateepavanich P, Kupniratsaikul V, Charoensak T. The relationship between myofascial trigger points of gastrocnemius muscle and nocturnal calf cramps. J Med Assoc Thai. 1999. 82:541–549.2. Travell JG, Simons DG. Myofascial pain and dysfunction. 1992. Volum 2:first edition. Baltimore: Williams & Wilkins.3. Bonica JJ, Sola AE. Bonica JJ, editor. Other painful disorders of the lower limbs. The management of pain. 1990. second edition. Malvern: Lea & Febiger;1621–1634.4. Walsh NE, Dumitru D, Schoenfeld LS, Ramamurthy S. Delisa JA, editor. Treatment of the patient with chronic pain. Physical Medicine and Rehabilitation: Principles and practice. 2005. 4th ed. Philadelphia: Lippincott Williams & Wilkins;493–529.5. Fabre T, Montero C, Gaujard E, Gervais-Dellion F, Durandeau A. Chronic calf pain in athletes due to sural nerve entrapment. A report of 18 cases. Am J Sports Med. 2000. 28:679–682.6. Enzinger FM, Weiss SW. Enzinger FM, Weiss SW, editors. Benign tumors and tumorlike lesions of blood vessels. Soft tissue tumors. 1995. third ed. St Louis: Mosby;579–626.7. Engelstad BL, Gilula LA, Kyriakos M. Ossified skeletal muscle hemangioma: radiologic and pathologic features. Skeletal Radiol. 1980. 5:35–40.
Article8. Greenspan A, McGahan J, Vogelsang P, Szabo RM. Imaging strategies in the evaluation of soft tissue hemangiomas of the extremities: correlation of the findings of plain radiography, angiography, CT, MRI, and ultrasonography in 12 histologically proven cases. Skeletal Radiol. 1992. 21:11–18.
Article9. Hawnaur JM, Whitehouse RW, Jenkins JP, Isherwood I. Musculoskeletal haemangiomas: comparison of MRI with CT. Skeletal Radiol. 1990. 19:251–258.
Article10. Kim EY, Ahn JM, Yoon HK, Suh YL, Do YS, Kim SH, Choo SW, Shoo IW, Kim SM, Kang HS. Intramuscular vascular malformations of an extremity: findings on MR imaging and pathologic correlation. Skeletal Radiol. 1999. 28:515–521.
Article11. Hatayama K, Watanabe H, Ahmed AR, Yanagawa T, Shinozaki T, Oriuchi N, Aoki J, Takeuchi K, Endo K, Takagishi K. Evaluation of hemangioma by positron emission tomography: role in a multimodality approach. J Comput Assist Tomogr. 2003. 27:70–77.
Article12. Jones KG. Cavernous hemangioma of striated muscle. J Bone Joint Surg Am. 1953. 35:717–728.
Article13. Conners JJ, Khan G. Hemangiomas of striated muscle. South Med J. 1977. 70:1423–1424.14. Kim SH, Shin HH, Rho BK, Lee ES, Baek SH. A case of intramuscular hemangioma presenting with large-angle hypertropia. Korean J Ophthalmol. 2006. 20:195–198.
Article15. Wu JL, Wu CC, Wang SJ, Chen YJ, Huang GS, Wu SS. Imaging strategies in intramuscular haemangiomas: an analysis of 20 cases. Int Orthop. 2006. Oct. 05. [Epub ahead of print].
Article16. Sung MS, Kang HS, Lee HG. Regional bone changes in deep soft tissue hemangioma: radiographic and MR features. Skeletal Radiol. 1998. 27:205–210.17. Levin DC, Gordon DH, McSweeney J. Arteriography of peripheral hemangiomas. Radiology. 1976. 121:625–630.
Article18. Hein KD, Mulliken JB, Kozakewich HP, Upton J, Burrows PE. Venous malformations fo skeletal muscle. Plast Reconstr Surg. 2002. 110:1625–1635.19. Beham A, Fletcher CD. Intramuscular angioma: a clinicopathological analysis of 74 cases. Histopathology. 1991. 18:53–59.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Incidentally Found Intramuscular Hemangioma, Mimicking Traumatic Hematoma after Military Training: A Case Report
- Intramuscular Stimulation Therapy
- Effects of Intramuscular Electrical Stimulation Using Inversely Placed Electrodes on Myofascial Pain Syndrome in the Shoulder: A Case Series
- The Effect of Intramuscular Stimulation on Otalgia due to Myofascial Pain Syndrome by Contraction of Trapezius Muscle
- Botulinum Toxin-Type A in Cervical Myofascial Pain Syndrome: A report of 3 cases