Tuberc Respir Dis.
2010 Mar;68(3):180-184. 10.4046/trd.2010.68.3.180.
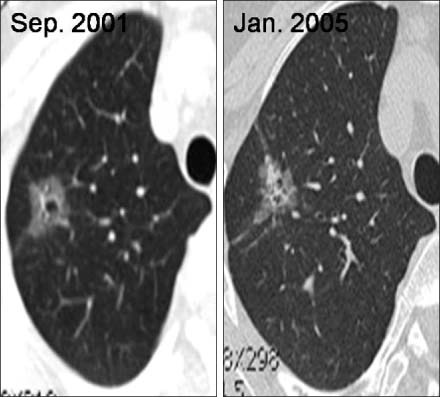
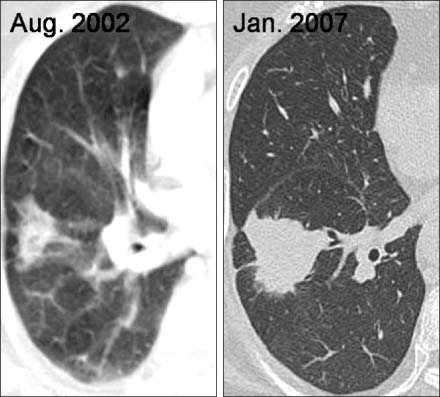
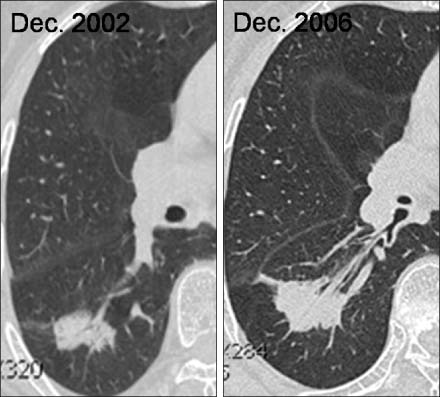
Clinical Characteristics of Slowly Growing Lung Cancer: 6 Case-Series Evaluation
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Inha University Hospital, College of Medicine, Inha University, Incheon, Korea. jsryu@inha.ac.kr
- 2Division of Hematooncology, Department of Internal Medicine, Inha University Hospital, College of Medicine, Inha University, Incheon, Korea.
- 3Department of Radiology, Inha University Hospital, College of Medicine, Inha University, Incheon, Korea.
- 4Department of Thoracic Surgery, Inha University Hospital, College of Medicine, Inha University, Incheon, Korea.
- KMID: 1728964
- DOI: http://doi.org/10.4046/trd.2010.68.3.180
Abstract
- Slowly growing lung cancers are quite rare and the leading cause of length time bias and over-diagnosis bias in lung cancer screening. We report 6 cases of slowly growing lung cancer in a tertiary hospital between January 1999 and December 2008. The clinical characteristics of these 6 cases with slowly growing lung cancer were examined. The median age at diagnosis was 68 years (range, 49~72), and 5 patients (83%) were female. The most common histology type was adenocarcinoma (83%). After excluding two patients who showed no change in the tumor size, the median tumor doubling time was 189 months (range, 86~387). The proportion of patients with slowly growing lung cancer appears to be particularly large in women, especially among patients with adenocarcinoma. Our experience shows that slowly growly lung cancers are more heterogeneous and diverse.
Keyword
MeSH Terms
Figure
Reference
-
1. Molina JR, Adjei AA, Jett JR. Advances in chemotherapy of non-small cell lung cancer. Chest. 2006. 130:1211–1219.2. Patz EF Jr, Goodman PC, Bepler G. Screening for lung cancer. N Engl J Med. 2000. 343:1627–1633.3. Jeong HC, Lee SY, Oh YH, In KH, Kim HG, Yoo SH. An adenocarcinoma of lung with unusual very slow growth: a case report. J Lung Cancer. 2006. 5:51–54.4. Kwon KD, Kim JH, Kim DY, Choi MH, Choi JH, Shin DW, et al. A case of adenocarcinoma presenting a solitary pulmonary nodule that grows slowly over 10 years. Tuberc Respir Dis. 2008. 64:318–323.5. Yoon BK, Kim EJ, Kim DI, Lee KH, Ryu JS, Kwak SM, et al. A case of adenocarcinoma presenting a solitary pulmonary nodule that showed no growth over 4 years. Tuberc Respir Dis. 2005. 59:326–329.6. Detterbeck FC, Gibson CJ. Turning gray: the natural history of lung cancer over time. J Thorac Oncol. 2008. 3:781–792.7. Hasegawa M, Sone S, Takashima S, Li F, Yang ZG, Maruyama Y, et al. Growth rate of small lung cancers detected on mass CT screening. Br J Radiol. 2000. 73:1252–1259.8. Lindell RM, Hartman TE, Swensen SJ, Jett JR, Midthun DE, Tazelaar HD, et al. Five-year lung cancer screening experience: CT appearance, growth rate, location, and histologic features of 61 lung cancers. Radiology. 2007. 242:555–562.9. Hillerdal G. Indolent lung cancers: time for a paradigm shift: a review. J Thorac Oncol. 2008. 3:208–211.10. Goldstraw P, Crowley J, Chansky K, Giroux DJ, Groome PA, Rami-Porta R, et al. The IASLC Lung Cancer Staging Project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM Classification of malignant tumours. J Thorac Oncol. 2007. 2:706–714.11. Joseph WL, Morton DL, Adkins PC. Prognostic significance of tumor doubling time in evaluating operability in pulmonary metastatic disease. J Thorac Cardiovasc Surg. 1971. 61:23–32.12. Aoki T, Nakata H, Watanabe H, Nakamura K, Kasai T, Hashimoto H, et al. Evolution of peripheral lung adenocarcinomas: CT findings correlated with histology and tumor doubling time. AJR Am J Roentgenol. 2000. 174:763–768.13. Marcus PM, Bergstralh EJ, Fagerstrom RM, Williams DE, Fontana R, Taylor WF, et al. Lung cancer mortality in the Mayo Lung Project: impact of extended follow-up. J Natl Cancer Inst. 2000. 92:1308–1316.14. Bach PB, Jett JR, Pastorino U, Tockman MS, Swensen SJ, Begg CB. Computed tomography screening and lung cancer outcomes. JAMA. 2007. 297:953–961.15. Bepler G, Goodridge Carney D, Djulbegovic B, Clark RA, Tockman M. A systematic review and lessons learned from early lung cancer detection trials using low-dose computed tomography of the chest. Cancer Control. 2003. 10:306–314.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Palliative Radiotherapy in a Patient with Pulmonary Adenoid Cystic Carcinoma
- A Case of Adenocarcinoma Presenting a Solitary Pulmonary Nodule that Grows Slowly Over 10 Years
- An Adenocarcinoma of Lung with Unusual Very Slow Growth : A case report
- Slowly growing lung mass in the right upper lobe in simple chest X-ray
- Inducing of Complete Necrosis of Recurred Lung Cancer by Cryoablation: A Case Report