Yonsei Med J.
2013 May;54(3):732-738. 10.3349/ymj.2013.54.3.732.
Comparison of Emergence Time in Children Undergoing Minor Surgery According to Anesthetic: Desflurane and Sevoflurane
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Anesthesia and Pain Research Institute, Yonsei University College of Medicine, Seoul, Korea. koobn@yuhs.ac
- KMID: 1727891
- DOI: http://doi.org/10.3349/ymj.2013.54.3.732
Abstract
- PURPOSE
In earlier analyses, desflurane has been shown to reduce average extubation time and the variability of extubation time by 20% to 25% relative to sevoflurane in adult patients. We undertook this study to determine which agents prompt less recovery time in pediatric patients undergoing minor surgery.
MATERIALS AND METHODS
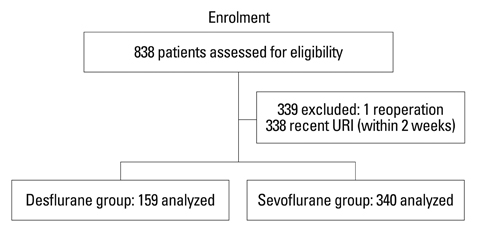
After obtaining Institutional Review Board approval, we retrospectively reviewed the anesthesia records of 499 patients, with an average age of 5 years, who underwent minor surgeries at Severance Eye and Ear, Nose and Throat Hospital between May 2010 and April 2011. Anesthesia was induced with propofol and rocuronium. Anesthesia was maintained with sevoflurane (n=340) or desflurane (n=159) with 50% air/O2. Time from cessation of anesthetics to recovery of self-respiration, eye opening on verbal command and extubation were compared between the two groups. Additionally, the incidences of postoperative respiratory adverse events were also compared.
RESULTS
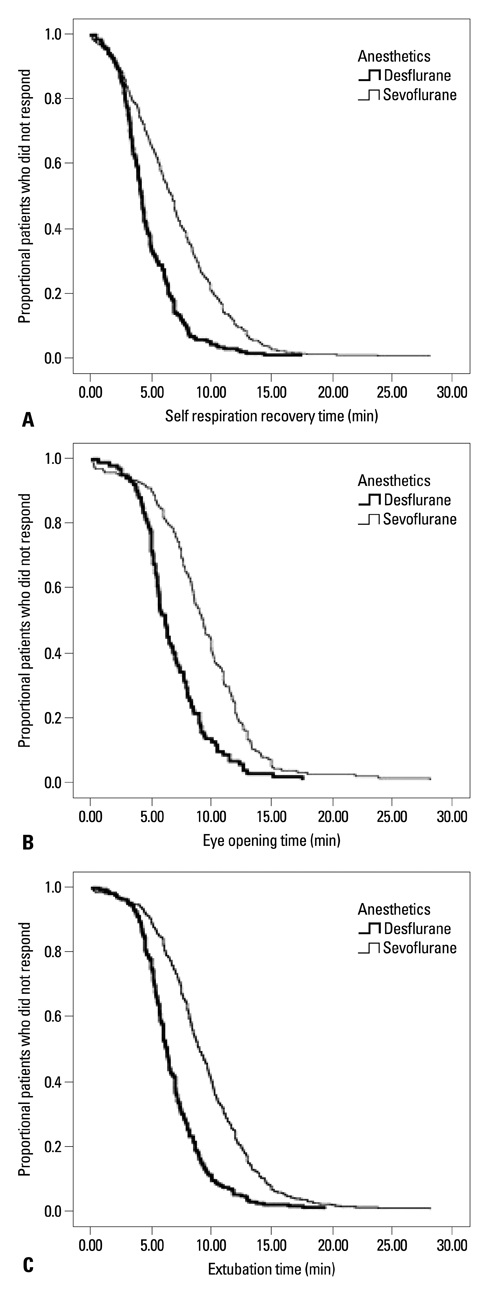
Times to self-respiration recovery, eye opening on verbal command, and extubation were significantly faster in the desflurane group than the sevoflurane group (4.6+/-2.5 min vs. 6.9+/-3.8 min, 6.6+/-3.0 min vs. 9.2+/-3.6 min, and 6.2+/-2.7 min vs. 9.3+/-3.7 min, respectively, p<0.005). There were no statistically significant differences between the two groups with respect to adverse respiratory events during the peri-operative period (38.2% vs. 34.6%, p=0.468).
CONCLUSION
Emergence and recovery from anesthesia were significantly faster in the desflurane group of children undergoing minor surgery. Desflurane did not result in any differences in respiratory adverse events during recovery compared to sevoflurane.
MeSH Terms
Figure
Cited by 3 articles
-
Kidney Function in Living Donors Undergoing Nephrectomy by Sevoflurane or Desflurane Anesthesia
Min-Soo Kim, Jeong-Rim Lee, Myoung-Soo Kim, Sung-Yeon Ham, Seung-Ho Choi
Yonsei Med J. 2013;54(5):1266-1272. doi: 10.3349/ymj.2013.54.5.1266.Effect of Dexmedetomidine on Sevoflurane Requirements and Emergence Agitation in Children Undergoing Ambulatory Surgery
Na Young Kim, So Yeon Kim, Hye Jin Yoon, Hae Keum Kil
Yonsei Med J. 2014;55(1):209-215. doi: 10.3349/ymj.2014.55.1.209.Sex Differences in Remifentanil Requirements for Preventing Cough during Anesthetic Emergence
Sarah Soh, Wyun Kon Park, Sang Wook Kang, Bo Ra Lee, Jeong Rim Lee
Yonsei Med J. 2014;55(3):807-814. doi: 10.3349/ymj.2014.55.3.807.
Reference
-
1. Chen X, Zhao M, White PF, Li S, Tang J, Wender RH, et al. The recovery of cognitive function after general anesthesia in elderly patients: a comparison of desflurane and sevoflurane. Anesth Analg. 2001. 93:1489–1494.
Article2. Dexter F, Bayman EO, Epstein RH. Statistical modeling of average and variability of time to extubation for meta-analysis comparing desflurane to sevoflurane. Anesth Analg. 2010. 110:570–580.
Article3. McKay RE, Large MJ, Balea MC, McKay WR. Airway reflexes return more rapidly after desflurane anesthesia than after sevoflurane anesthesia. Anesth Analg. 2005. 100:697–700.
Article4. Lele E, Petak F, Fontao F, Morel DR, Habre W. Protective effects of volatile agents against acetylcholine-induced bronchoconstriction in isolated perfused rat lungs. Acta Anaesthesiol Scand. 2006. 50:1145–1151.
Article5. McKay RE, Bostrom A, Balea MC, McKay WR. Airway responses during desflurane versus sevoflurane administration via a laryngeal mask airway in smokers. Anesth Analg. 2006. 103:1147–1154.
Article6. Klock PA Jr, Czeslick EG, Klafta JM, Ovassapian A, Moss J. The effect of sevoflurane and desflurane on upper airway reactivity. Anesthesiology. 2001. 94:963–967.
Article7. Goff MJ, Arain SR, Ficke DJ, Uhrich TD, Ebert TJ. Absence of bronchodilation during desflurane anesthesia: a comparison to sevoflurane and thiopental. Anesthesiology. 2000. 93:404–408.8. Dikmen Y, Eminoglu E, Salihoglu Z, Demiroluk S. Pulmonary mechanics during isoflurane, sevoflurane and desflurane anaesthesia. Anaesthesia. 2003. 58:745–748.
Article9. Chung F. Discharge criteria--a new trend. Can J Anaesth. 1995. 42:1056–1058.10. Merkel SI, Voepel-Lewis T, Shayevitz JR, Malviya S. The FLACC: a behavioral scale for scoring postoperative pain in young children. Pediatr Nurs. 1997. 23:293–297.11. Lerman J. Inhalational anesthetics. Paediatr Anaesth. 2004. 14:380–383.
Article12. White PF, Tang J, Wender RH, Yumul R, Stokes OJ, Sloninsky A, et al. Desflurane versus sevoflurane for maintenance of outpatient anesthesia: the effect on early versus late recovery and perioperative coughing. Anesth Analg. 2009. 109:387–393.
Article13. Welborn LG, Hannallah RS, Norden JM, Ruttimann UE, Callan CM. Comparison of emergence and recovery characteristics of sevoflurane, desflurane, and halothane in pediatric ambulatory patients. Anesth Analg. 1996. 83:917–920.
Article14. McKay RE, Malhotra A, Cakmakkaya OS, Hall KT, McKay WR, Apfel CC. Effect of increased body mass index and anaesthetic duration on recovery of protective airway reflexes after sevoflurane vs desflurane. Br J Anaesth. 2010. 104:175–182.
Article15. von Ungern-Sternberg BS, Saudan S, Petak F, Hantos Z, Habre W. Desflurane but not sevoflurane impairs airway and respiratory tissue mechanics in children with susceptible airways. Anesthesiology. 2008. 108:216–224.
Article16. Lee J, Oh Y, Kim C, Kim S, Park H, Kim H. Fentanyl reduces desflurane-induced airway irritability following thiopental administration in children. Acta Anaesthesiol Scand. 2006. 50:1161–1164.
Article17. Kong CF, Chew ST, Ip-Yam PC. Intravenous opioids reduce airway irritation during induction of anaesthesia with desflurane in adults. Br J Anaesth. 2000. 85:364–367.
Article18. Aouad MT, Nasr VG. Emergence agitation in children: an update. Curr Opin Anaesthesiol. 2005. 18:614–619.
Article19. Pieters BJ, Penn E, Nicklaus P, Bruegger D, Mehta B, Weatherly R. Emergence delirium and postoperative pain in children undergoing adenotonsillectomy: a comparison of propofol vs sevoflurane anesthesia. Paediatr Anaesth. 2010. 20:944–950.
Article20. Aouad MT, Yazbeck-Karam VG, Nasr VG, El-Khatib MF, Kanazi GE, Bleik JH. A single dose of propofol at the end of surgery for the prevention of emergence agitation in children undergoing strabismus surgery during sevoflurane anesthesia. Anesthesiology. 2007. 107:733–738.
Article21. Dong YX, Meng LX, Wang Y, Zhang JJ, Zhao GY, Ma CH. The effect of remifentanil on the incidence of agitation on emergence from sevoflurane anaesthesia in children undergoing adenotonsillectomy. Anaesth Intensive Care. 2010. 38:718–722.
Article22. Przybylo HJ, Martini DR, Mazurek AJ, Bracey E, Johnsen L, Coté CJ. Assessing behaviour in children emerging from anaesthesia: can we apply psychiatric diagnostic techniques? Paediatr Anaesth. 2003. 13:609–616.
Article23. Dexter F, Macario A, Manberg PJ, Lubarsky DA. Computer simulation to determine how rapid anesthetic recovery protocols to decrease the time for emergence or increase the phase I postanesthesia care unit bypass rate affect staffing of an ambulatory surgery center. Anesth Analg. 1999. 88:1053–1063.
Article24. Macario A, Dexter F. Effect of compensation and patient scheduling on OR labor costs. AORN J. 2000. 71:860863–869.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of emergence agitation between sevoflurane, desflurane, and propofol with bispectral index monitoring in pediatric anesthesia
- The change of sevoflurane to desflurane after anesthesia induction induces rapid emergence without increased cardiovascular responses and emergence delirium in pediatric strabismus surgery patients
- The Effects of Anesthetic Agents on Emergence Delirium in Pediatric Strabismus Surgery
- A Comparative Study of Emergence Agitation between Sevoflurane and Desflurane Anesthesia in Children
- Comparison of Isoflurane, Sevoflurane and Desflurane Anesthesia on Potentiation of Muscle Relaxation, Recovery Profile and Cost according to Consumed Amount