J Korean Soc Transplant.
2014 Sep;28(3):154-159. 10.4285/jkstn.2014.28.3.154.
Ex Vivo Lung Perfusion of Cardiac-death Donor Lung in Pigs
- Affiliations
-
- 1Department of Thoracic and Cardiovascular Surgery, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. hcpaik@yuhs.ac
- 2Department of Thoracic and Cardiovascular Surgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 3Division of Pulmonology, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 1727519
- DOI: http://doi.org/10.4285/jkstn.2014.28.3.154
Abstract
- BACKGROUND
Lung transplantation (LTx) is a life-saving treatment for patients with end-stage lung disease; however, the shortage of donor lungs has been a major limiting factor to increasing the number of LTx. Growing experience following LTx using donor lungs after cardiac death (DCD) has been promising, although concerns remain. The purpose of this study was to develop a DCD lung harvest model using an ex vivo lung perfusion (EVLP) system and to assess the function of presumably damaged lungs harvested from the DCD donor in pigs.
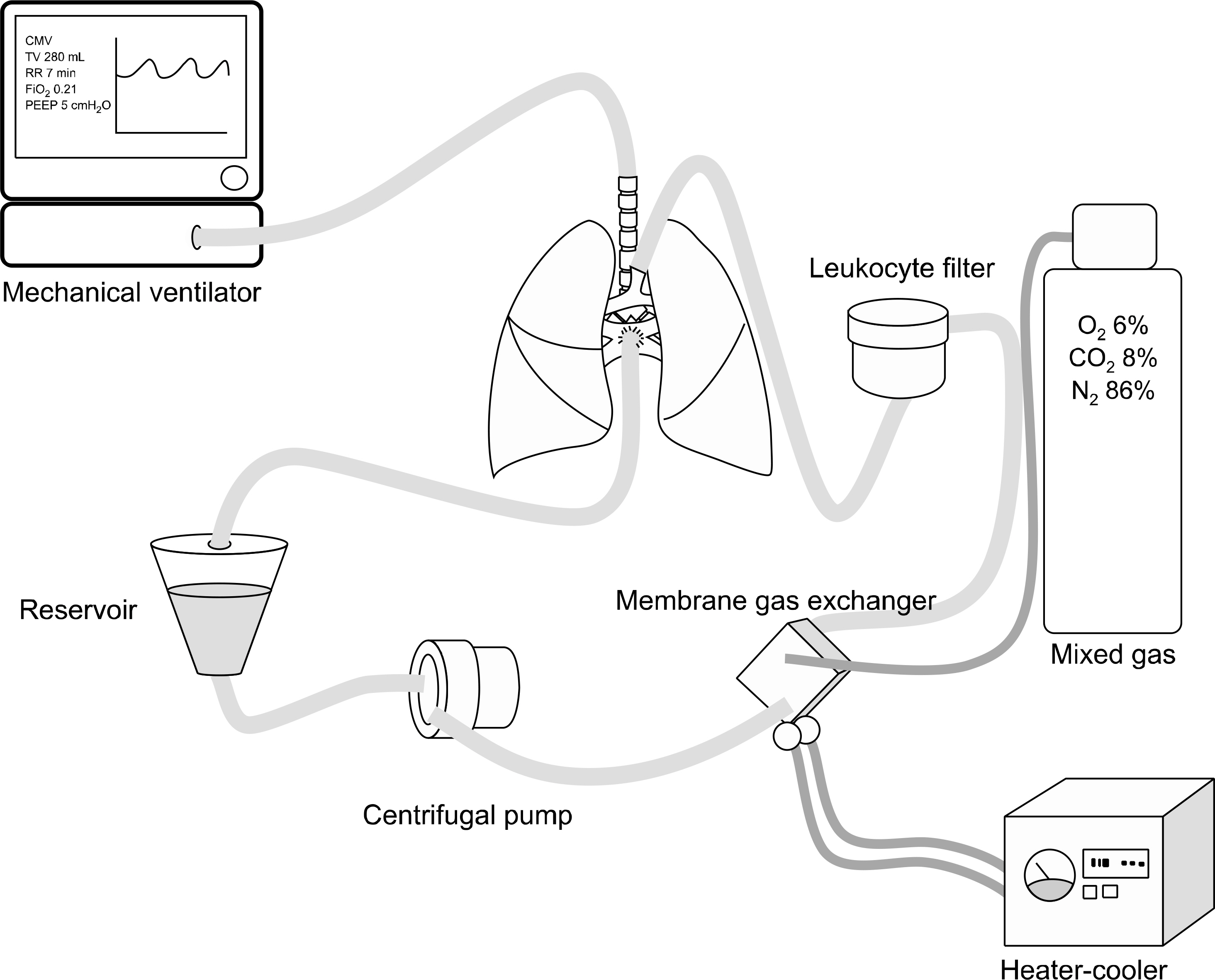
METHODS
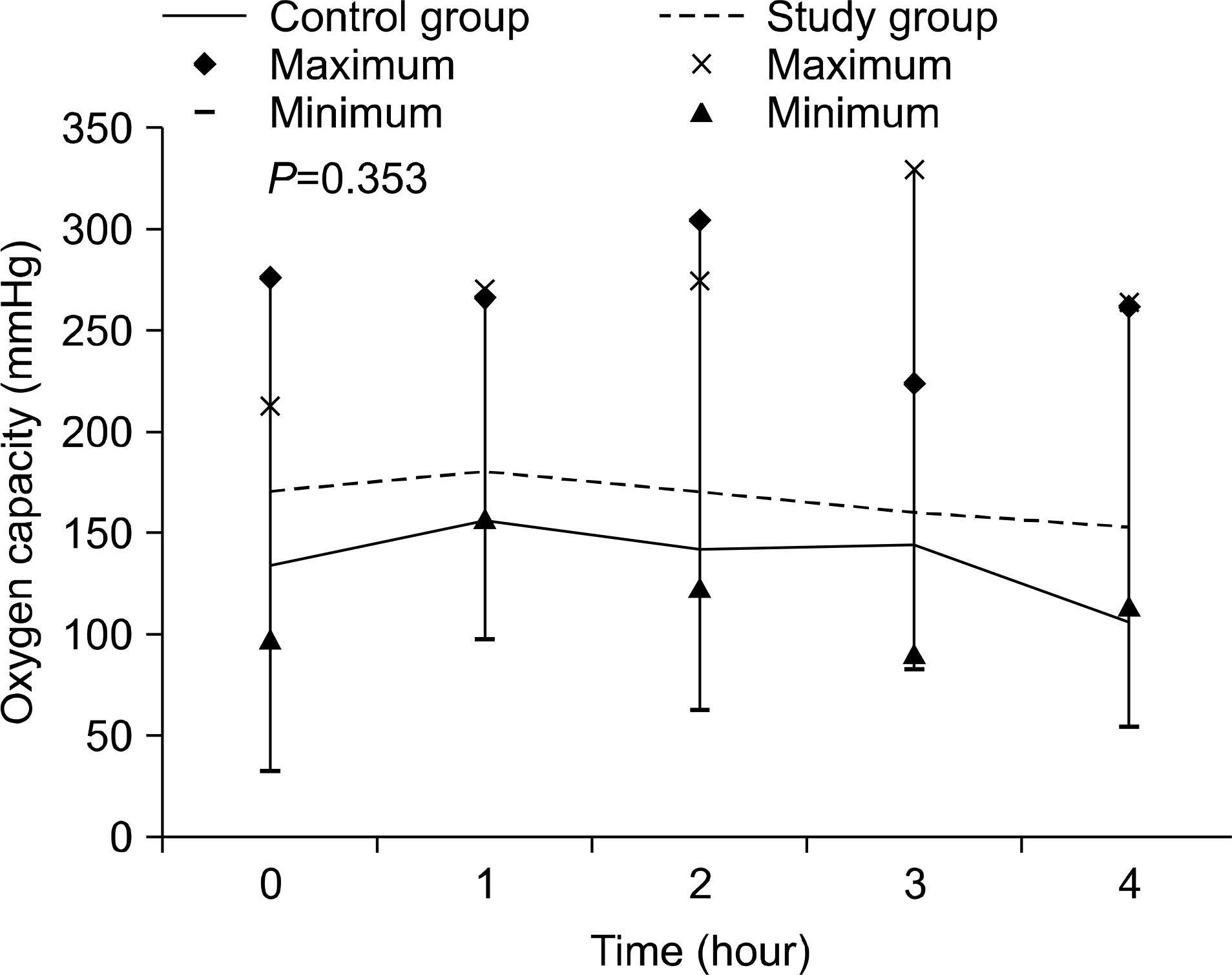
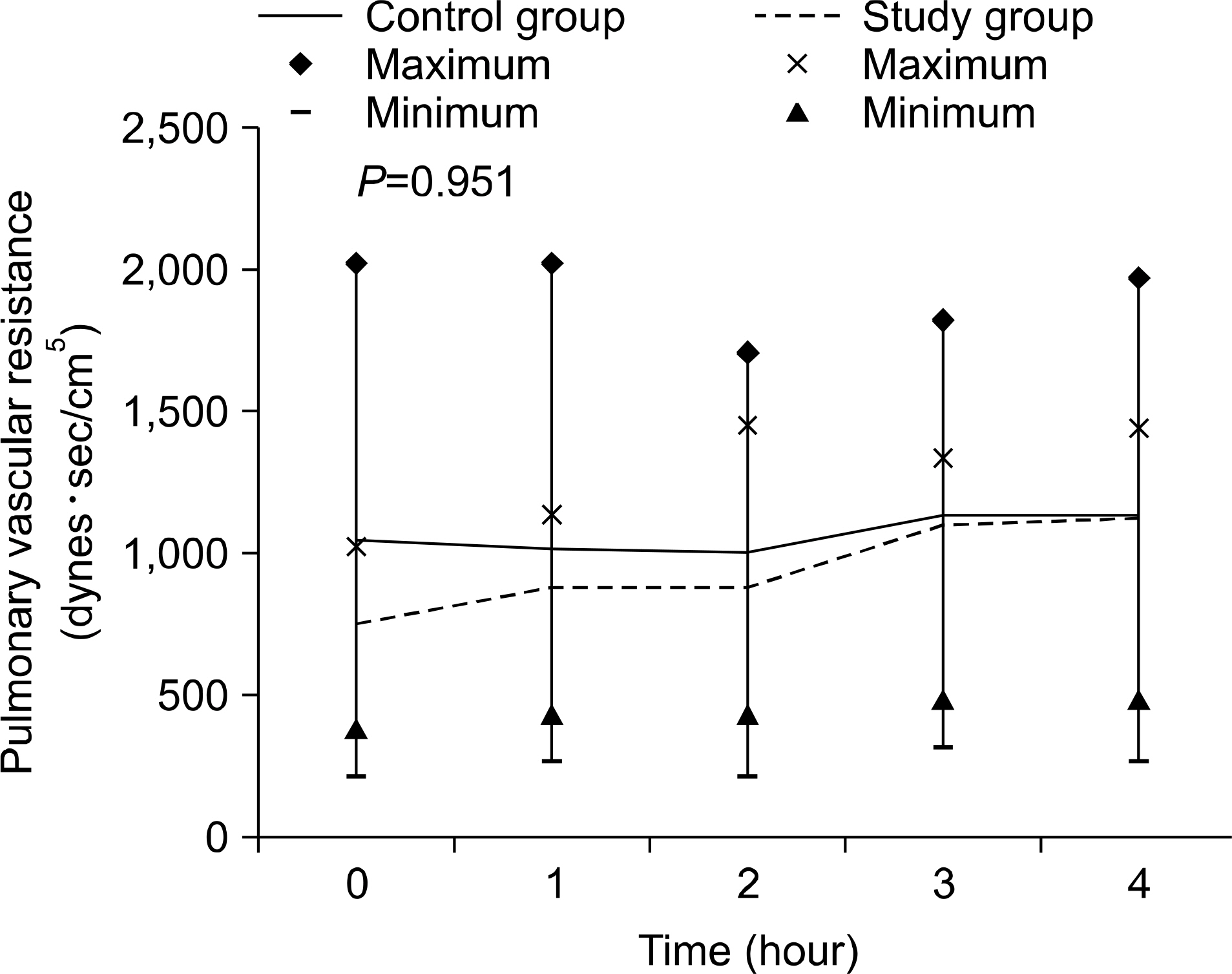
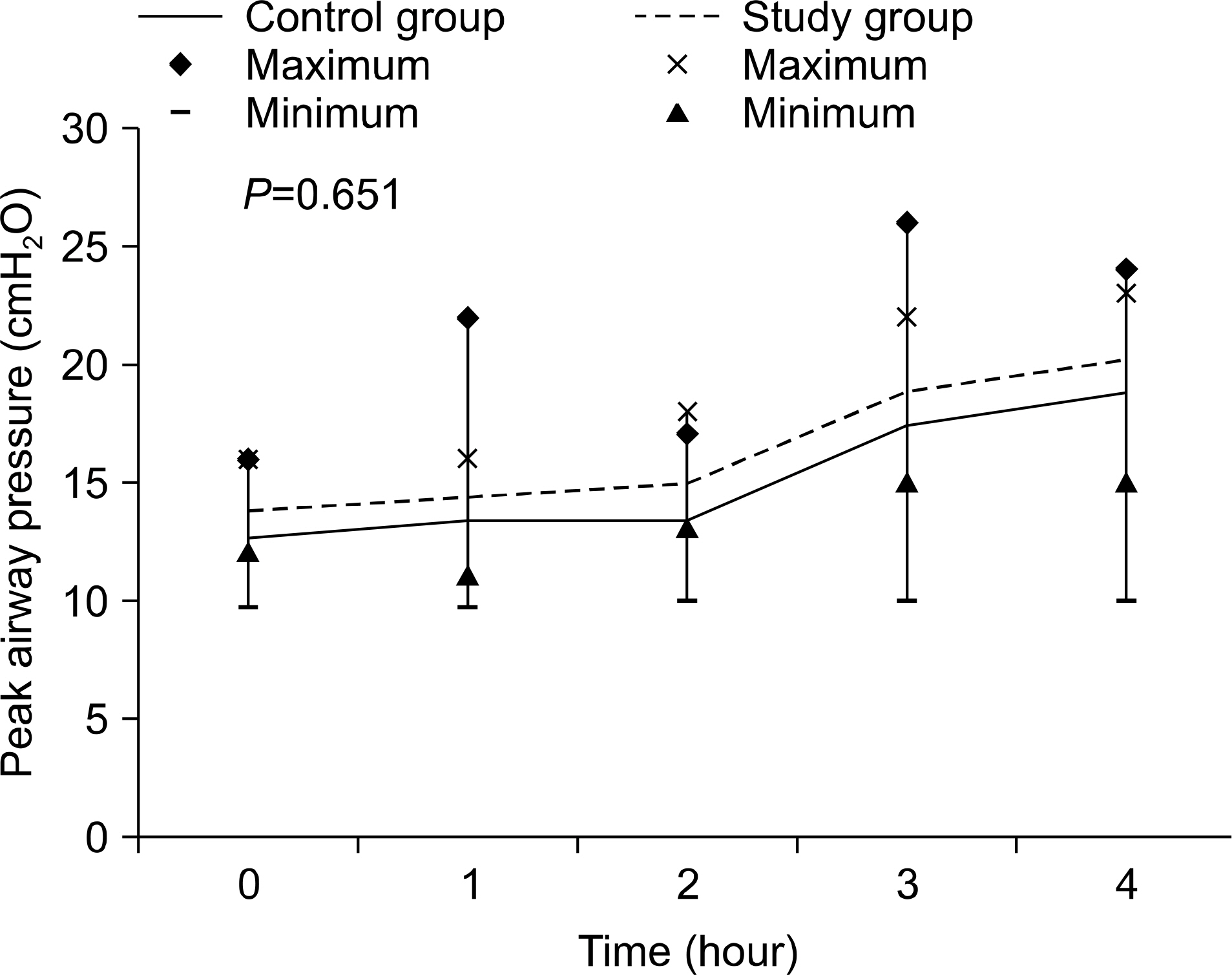
The 40 kg pigs were randomly divided into the control group with no ischemic lung injury (n=5) and the study group (n=5), which had 1 hour of warm ischemic lung injury after cardiac arrest. Harvested lungs were placed in the EVLP circuit and oxygen capacities (OC), pulmonary vascular resistance (PVR), and peak airway pressure (PAP) were evaluated every hour for 4 hours. At the end of EVLP, specimens were excised for pathologic review and wet/dry ratio.
RESULTS
No statistically significant difference in OC (P=0.353), PVR (P=0.951), and PAP (P=0.651) was observed in both groups. Lung injury severity score (control group vs. study group: 0.700+/-0.303 vs. 0.870+/-0.130; P=0.230) and wet/dry ratio (control group vs. study group: 5.89+/-0.97 vs. 6.20+/-0.57; P=0.560) also showed no statistically significant difference between the groups.
CONCLUSIONS
The function of DCD lungs assessed using EVLP showed no difference from that of control lungs without ischemic injury; therefore, utilization of DCD lungs can be a new option to decrease the number of deaths on the waiting list.
MeSH Terms
Figure
Reference
-
References
1). Paik HC, Haam SJ, Lee DY, Yi GJ, Song SW, Kim YT, et al. Donor evaluation for lung transplantation in Korea. Transplant Proc. 2012; 44:870–4.
Article2). De Meester J, Smits JM, Persijn GG, Haverich A. Listing for lung transplantation: life expectancy and transplant effect, stratified by type of end-stage lung disease, the Eurotransplant experience. J Heart Lung Transplant. 2001; 20:518–24.
Article3). Botha P, Trivedi D, Weir CJ, Searl CP, Corris PA, Dark JH, et al. Extended donor criteria in lung transplantation: impact on organ allocation. J Thorac Cardiovasc Surg. 2006; 131:1154–60.
Article4). Date H. Update on living-donor lobar lung transplantation. Curr Opin Organ Transplant. 2011; 16:453–7.
Article5). Cypel M, Yeung JC, Liu M, Anraku M, Chen F, Karolak W, et al. Normothermic ex vivo lung perfusion in clinical lung transplantation. N Engl J Med. 2011; 364:1431–40.
Article6). Wigfield CH, Love RB. Donation after cardiac death lung transplantation outcomes. Curr Opin Organ Transplant. 2011; 16:462–8.
Article7). Kootstra G, Daemen JH, Oomen AP. Categories of non-heart-beating donors. Transplant Proc. 1995; 27:2893–4.8). Ingemansson R, Eyjolfsson A, Mared L, Pierre L, Algotsson L, Ekmehag B, et al. Clinical transplantation of initially re-jected donor lungs after reconditioning ex vivo. Ann Thorac Surg. 2009; 87:255–60.
Article9). Fang WF, Cho JH, He Q, Lin MC, Wu CC, Voelkel NF, et al. Lipid A fraction of LPS induces a discrete MAPK activation in acute lung injury. Am J Physiol Lung Cell Mol Physiol. 2007; 293:L336–44.
Article10). Steen S, Sjö berg T, Pierre L, Liao Q, Eriksson L, Algotsson L. Transplantation of lungs from a non-heart-beating donor. Lancet. 2001; 357:825–9.
Article11). De Oliveira NC, Osaki S, Maloney JD, Meyer KC, Kohmoto T, D'Alessandro AM, et al. Lung transplantation with donation after cardiac death donors: longterm follow-up in a single center. J Thorac Cardiovasc Surg. 2010; 139:1306–15.
Article12). Christie JD, Edwards LB, Kucheryavaya AY, Benden C, Dipchand AI, Dobbels F, et al. The Registry of the International Society for Heart and Lung Transplantation: 29th adult lung and heart-lung transplant report-2012. J Heart Lung Transplant. 2012; 31:1073–86.
Article13). United Network for Organ Sharing (UNOS). Donation after cardiac death (DCD) lung donors transplant outcomes [Internet]. Richmond: UNOS;2010. [cited 2014 Mar 3]. Available from:. http://www.unos.org/about/index.php?topic=newsroom&article_id=2631.14). Snell GI, Levvey BJ, Oto T, McEgan R, Pilcher D, Davies A, et al. Early lung transplantation success utilizing controlled donation after cardiac death donors. Am J Transplant. 2008; 8:1282–9.
Article15). Steen S, Liao Q, Wierup PN, Bolys R, Pierre L, Sjö berg T. Transplantation of lungs from non-heart-beating donors after functional assessment ex vivo. Ann Thorac Surg. 2003; 76:244–52.
Article16). Rega FR, Wuyts WA, Vanaudenaerde BM, Jannis NC, Neyrinck AP, Verleden GM, et al. Nebulized N-acetyl cysteine protects the pulmonary graft inside the non-heart-beating donor. J Heart Lung Transplant. 2005; 24:1369–77.
Article17). Cypel M, Liu M, Rubacha M, Yeung JC, Hirayama S, Anraku M, et al. Functional repair of human donor lungs by IL-10 gene therapy. Sci Transl Med. 2009; 1:4ra9.
Article18). Cypel M, Yeung JC, Hirayama S, Rubacha M, Fischer S, Anraku M, et al. Technique for prolonged normothermic ex vivo lung perfusion. J Heart Lung Transplant. 2008; 27:1319–25.
Article19). Mason DP, Brown CR, Murthy SC, Vakil N, Lyon C, Budev MM, et al. Growing singlecenter experience with lung transplantation using donation after cardiac death. Ann Thorac Surg. 2012; 94:406–11.
Article20). Neyrinck AP, Van De Wauwer C, Geudens N, Rega FR, Verleden GM, Wouters P, et al. Comparative study of donor lung injury in heart-beating versus non-heart-beating donors. Eur J Cardiothorac Surg. 2006; 30:628–36.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ex Vivo Lung Perfusion in Lung Transplantation
- Ex vivo lung perfusion and the Organ Care System: a review
- Beating heart and breathing lungs in the box: future of transplant and beyond
- Ex vivo Lung Perfusion Model in Lung Transplantation
- Cost-effective donor lung preservation with high-volume continuous perfusate purification in ex vivo lung perfusion