Clin Transplant Res.
2024 Mar;38(1):23-36. 10.4285/ctr.23.0057.
Ex vivo lung perfusion and the Organ Care System: a review
- Affiliations
-
- 1Institute of Heart and Lung Transplant, Krishna Institute of Medical Sciences (KIMS) Hospital, Secunderabad, India
- KMID: 2555994
- DOI: http://doi.org/10.4285/ctr.23.0057
Abstract
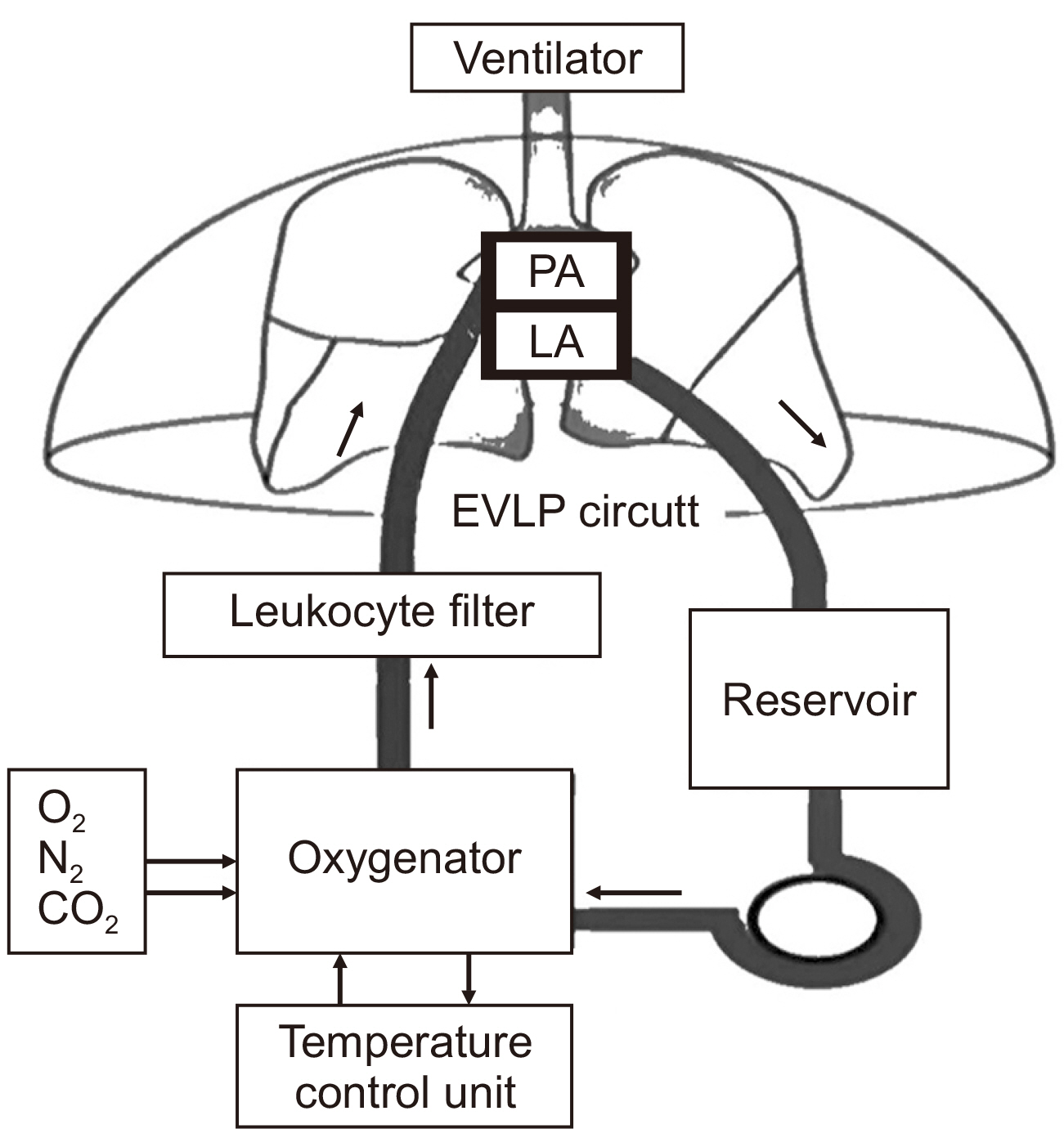
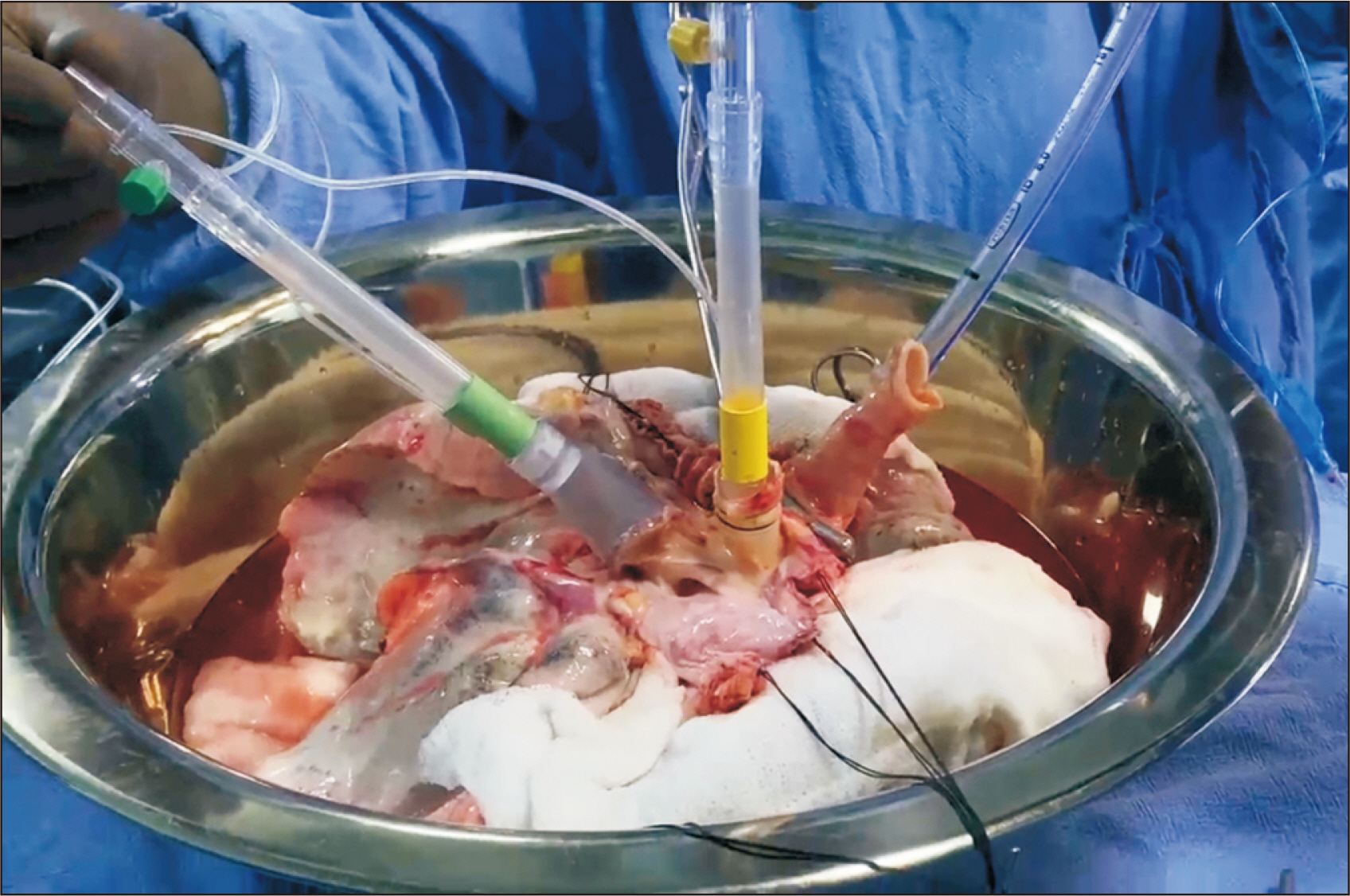
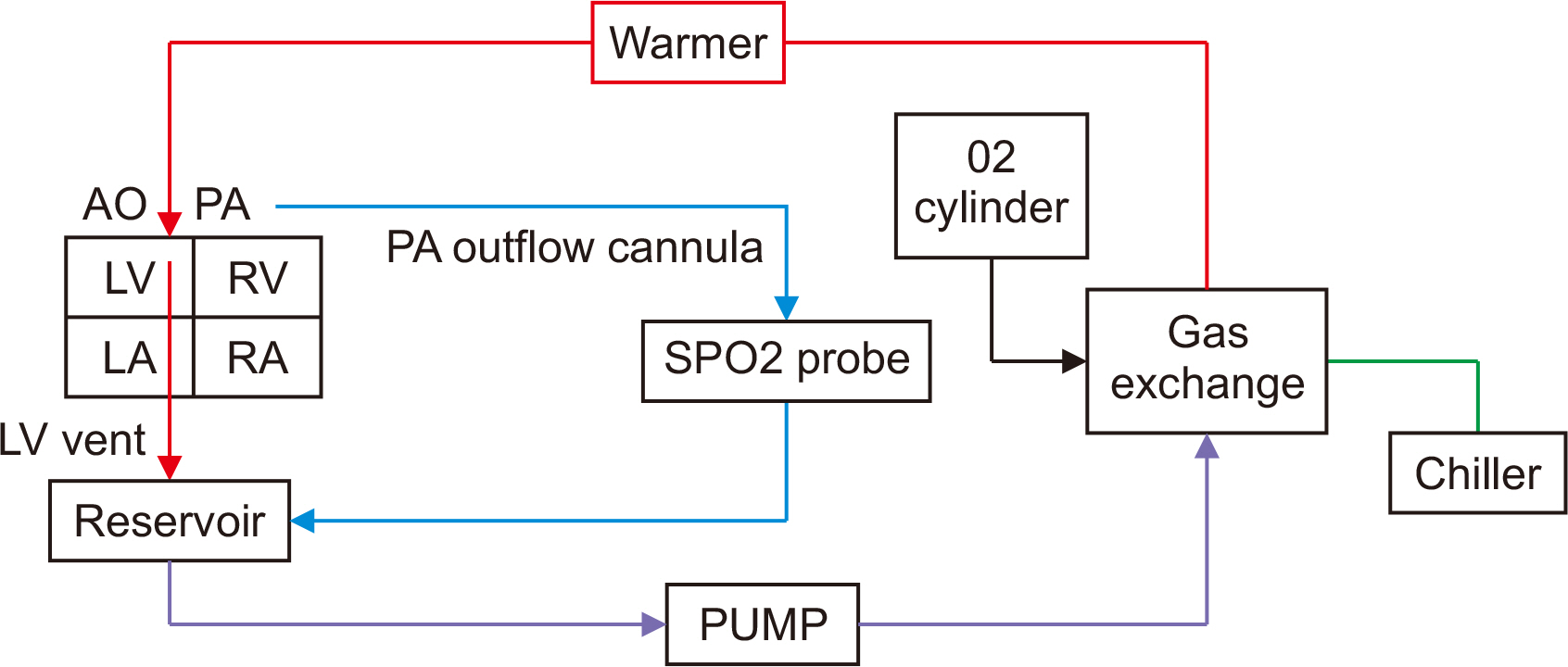
- With the increasing prevalence of heart failure and end-stage lung disease, there is a sustained interest in expanding the donor pool to alleviate the thoracic organ shortage crisis. Efforts to extend the standard donor criteria and to include donation after circulatory death have been made to increase the availability of suitable organs. Studies have demonstrated that outcomes with extended-criteria donors are comparable to those with standard-criteria donors. Another promising approach to augment the donor pool is the improvement of organ preservation techniques. Both Ex vivo lung perfusion (EVLP) for the lungs and the Organ Care System (OCS, TransMedics) for the heart have shown encouraging results in preserving organs and extending ischemia time through the application of normothermic regional perfusion. EVLP has been effective in improving marginal or borderline lungs by preserving and reconditioning them. The use of OCS is associated with excellent short-term outcomes for cardiac allografts and has improved utilization rates of hearts from extended-criteria donors. While both EVLP and OCS have successfully transitioned from research to clinical practice, the costs associated with commercially available systems and consumables must be considered. The Ex vivo perfusion platform, which includes both EVLP and OCS, holds the potential for diverse and innovative therapies, thereby transforming the landscape of thoracic organ transplantation.
Figure
Reference
-
1. Lund LH, Khush KK, Cherikh WS, Goldfarb S, Kucheryavaya AY, Levvey BJ, et al. 2017; The registry of the International Society for Heart and Lung Transplantation: thirty-fourth adult heart transplantation report-2017; focus theme: allograft ischemic time. J Heart Lung Transplant. 36:1037–46. DOI: 10.1016/j.healun.2017.07.019. PMID: 28779893.
Article2. Chambers DC, Yusen RD, Cherikh WS, Goldfarb SB, Kucheryavaya AY, Khusch K, et al. 2017; The registry of the International Society for Heart and Lung Transplantation: thirty-fourth adult lung and heart-lung transplantation report-2017; focus theme: allograft ischemic time. J Heart Lung Transplant. 36:1047–59. DOI: 10.1016/j.healun.2017.07.016. PMID: 28784324.3. Barnard CN. 1967; The operation. A human cardiac transplant: an interim report of a successful operation performed at Groote Schuur Hospital, Cape Town. S Afr Med J. 41:1271–4.4. Hardy JD, Eraslan S, Webb WR. 1964; Transplantation of the lung. Ann Surg. 160:440–8. DOI: 10.1097/00000658-196409000-00008. PMID: 14206849. PMCID: PMC1408772.
Article5. Paik HC, Hwang JJ, Kim DH, Joung EK, Kim HK, Lee DY. 2006; The 10 years experience of lung transplantation. Korean J Thorac Cardiovasc Surg. 39:822–7.6. Korean Network for Organ Sharing (KONOS). 2019. 2019 Annual data report [Internet]. KONOS;Available from: http://konos.go.kr. cited 2023 Dec 23.7. Jung SH, Kim JJ, Choo SJ, Yun TJ, Chung CH, Lee JW. 2011; Long-term mortality in adult orthotopic heart transplant recipients. J Korean Med Sci. 26:599–603. DOI: 10.3346/jkms.2011.26.5.599. PMID: 21532848. PMCID: PMC3082109.
Article8. Korea Organ Donation Agency (KODA). 2023. Transplant status: deceased donor organ transplantation status (2000-2022) [Internet]. KODA;Available from: https://www.koda1458.kr/info/transplant.do. cited 2023 Dec 23.9. Englbrecht JS, Schrader D, Kraus H, Schäfer M, Schedler D, Bach F, et al. 2023; How large is the potential of brain dead donors and what prevents utilization? A multicenter retrospective analysis at seven university hospitals in North Rhine-Westphalia. Transpl Int. 36:11186. DOI: 10.3389/ti.2023.11186. PMID: 37252613. PMCID: PMC10211426.
Article10. Blackstone EH, Rajeswaran J, Cruz VB, Hsich EM, Koprivanac M, Smedira NG, et al. 2018; Continuously updated estimation of heart transplant waitlist mortality. J Am Coll Cardiol. 72:650–9. DOI: 10.1016/j.jacc.2018.05.045. PMID: 30071995. PMCID: PMC6298792.
Article11. Valapour M, Lehr CJ, Schladt DP, Smith JM, Goff R, Mupfudze TG, et al. 2023; OPTN/SRTR 2021 annual data report: lung. Am J Transplant. 23(2 Suppl 1):S379–442. DOI: 10.1016/j.ajt.2023.02.009. PMID: 37132345. PMCID: PMC9970343.
Article12. Yeung JC, Keshavjee S. 2014; Overview of clinical lung transplantation. Cold Spring Harb Perspect Med. 4:a015628. DOI: 10.1101/cshperspect.a015628. PMID: 24384816. PMCID: PMC3869283.
Article13. Kilic A, Emani S, Sai-Sudhakar CB, Higgins RS, Whitson BA. 2014; Donor selection in heart transplantation. J Thorac Dis. 6:1097–104.14. Roselli EE, Smedira NG. 2004; Surgical advances in heart and lung transplantation. Anesthesiol Clin North Am. 22:789–807. DOI: 10.1016/j.atc.2004.06.011. PMID: 15541936.
Article15. Weingarten N, Iyengar A, Herbst DA, Helmers M, Meldrum D, Guevara-Plunkett S, et al. 2023; Extended criteria donor organ use for heart-lung transplantation in the modern era. Clinics (Sao Paulo). 78:100205. DOI: 10.1016/j.clinsp.2023.100205. PMID: 37120982. PMCID: PMC10172855.
Article16. Van Raemdonck D, Rega F, Rex S, Neyrinck A. 2018; Machine perfusion of thoracic organs. J Thorac Dis. 10(Suppl 8):S910–23. DOI: 10.21037/jtd.2018.02.85. PMID: 29744218. PMCID: PMC5934115.
Article17. A definition of irreversible coma. 1968; Report of the Ad Hoc Committee of the Harvard Medical School to Examine the Definition of Brain Death. JAMA. 205:337–40. DOI: 10.1001/jama.1968.03140320031009.18. Kootstra G, Daemen JH, Oomen AP. 1995; Categories of non-heart-beating donors. Transplant Proc. 27:2893–4.19. Egan TM, Lambert CJ Jr, Reddick R, Ulicny KS Jr, Keagy BA, Wilcox BR. 1991; A strategy to increase the donor pool: use of cadaver lungs for transplantation. Ann Thorac Surg. 52:1113–20. DOI: 10.1016/0003-4975(91)91290-C. PMID: 1953132.
Article20. Love RB, Stringham J, Chomiak PN, Pellet JR, Mentzer RM. 1995; First successful lung transplantation using a nonheart-beating donor. J Heart Lung Transplant. 14:S88.21. Ruttens D, Martens A, Ordies S, Verleden SE, Neyrinck AP, Vos R, et al. 2017; Short- and long-term outcomes after lung transplantation from circulatory-dead donors: a single-center experience. Transplantation. 101:2691–4. DOI: 10.1097/TP.0000000000001678. PMID: 28207629.22. Krutsinger D, Reed RM, Blevins A, Puri V, De Oliveira NC, Zych B, et al. 2015; Lung transplantation from donation after cardiocirculatory death: a systematic review and meta-analysis. J Heart Lung Transplant. 34:675–84. DOI: 10.1016/j.healun.2014.11.009. PMID: 25638297.
Article23. Cypel M, Levvey B, Van Raemdonck D, Erasmus M, Dark J, Love R, et al. 2015; International Society for Heart and Lung Transplantation Donation After Circulatory Death Registry report. J Heart Lung Transplant. 34:1278–82. DOI: 10.1016/j.healun.2015.08.015. PMID: 26454741.
Article24. Carrel A, Lindbergh CA. 1935; The culture of whole organs. Science. 81:621–3. DOI: 10.1126/science.81.2112.621. PMID: 17733174.
Article25. Jirsch DW, Fisk RL, Couves CM. 1970; Ex vivo evaluation of stored lungs. Ann Thorac Surg. 10:163–8. DOI: 10.1016/S0003-4975(10)65582-8. PMID: 4913761.
Article26. Cypel M, Yeung JC, Liu M, Anraku M, Chen F, Karolak W, et al. 2011; Normothermic ex vivo lung perfusion in clinical lung transplantation. N Engl J Med. 364:1431–40. DOI: 10.1056/NEJMoa1014597. PMID: 21488765.
Article27. Cypel M, Yeung JC, Machuca T, Chen M, Singer LG, Yasufuku K, et al. 2012; Experience with the first 50 ex vivo lung perfusions in clinical transplantation. J Thorac Cardiovasc Surg. 144:1200–6. DOI: 10.1016/j.jtcvs.2012.08.009. PMID: 22944089.28. Machuca TN, Cypel M. 2014; Ex vivo lung perfusion. J Thorac Dis. 6:1054–62.
Article29. Lindstedt S, Eyjolfsson A, Koul B, Wierup P, Pierre L, Gustafsson R, et al. 2011; How to recondition ex vivo initially rejected donor lungs for clinical transplantation: clinical experience from lund university hospital. J Transplant. 2011:754383. DOI: 10.1155/2011/754383. PMID: 21876780. PMCID: PMC3163037.30. Warnecke G, Moradiellos J, Tudorache I, Kühn C, Avsar M, Wiegmann B, et al. 2012; Normothermic perfusion of donor lungs for preservation and assessment with the Organ Care System Lung before bilateral transplantation: a pilot study of 12 patients. Lancet. 380:1851–8. DOI: 10.1016/S0140-6736(12)61344-0. PMID: 23063317.
Article31. Loor G. 2019; EVLP: ready for prime time? Semin Thorac Cardiovasc Surg. 31:1–6. DOI: 10.1053/j.semtcvs.2018.05.005. PMID: 29935227.
Article32. Lindstedt S, Hlebowicz J, Koul B, Wierup P, Sjögren J, Gustafsson R, et al. 2011; Comparative outcome of double lung transplantation using conventional donor lungs and non-acceptable donor lungs reconditioned ex vivo. Interact Cardiovasc Thorac Surg. 12:162–5. DOI: 10.1510/icvts.2010.244830. PMID: 21123199.
Article33. Fisher A, Andreasson A, Chrysos A, Lally J, Mamasoula C, Exley C, et al. 2016; An observational study of donor ex vivo lung perfusion in UK lung transplantation: DEVELOP-UK. Health Technol Assess. 20:1–276. DOI: 10.3310/hta20850.
Article34. Slama A, Schillab L, Barta M, Benedek A, Mitterbauer A, Hoetzenecker K, et al. 2017; Standard donor lung procurement with normothermic ex vivo lung perfusion: a prospective randomized clinical trial. J Heart Lung Transplant. 36:744–53. DOI: 10.1016/j.healun.2017.02.011. PMID: 28314503.
Article35. Loor G, Warnecke G, Villavicencio MA, Smith MA, Kukreja J, Ardehali A, et al. 2019; Portable normothermic ex-vivo lung perfusion, ventilation, and functional assessment with the Organ Care System on donor lung use for transplantation from extended-criteria donors (EXPAND): a single-arm, pivotal trial. Lancet Respir Med. 7:975–84. DOI: 10.1016/S2213-2600(19)30200-0. PMID: 31378427.
Article36. Loor G, Warnecke G, Villavicencio MA, Smith MA, Kukreja J, Ardehali A, et al. 2022; Long-term results of the OCS Lung EXPAND international trial using Organ Care System Lung Perfusion System (OCS) in extended-criteria donor (ECD) and donation after circulatory death (DCD) donor lungs. J Heart Lung Transplant. 41(4 Suppl):S43. DOI: 10.1016/j.healun.2022.01.097.
Article37. Hsin M, Au T. 2018; Ex vivo lung perfusion: a potential platform for molecular diagnosis and ex vivo organ repair. J Thorac Dis. 10(Suppl 16):S1871–83. DOI: 10.21037/jtd.2018.04.119. PMID: 30026974. PMCID: PMC6035934.
Article38. Renne J, Gutberlet M, Voskrebenzev A, Kern A, Kaireit T, Hinrichs J, et al. 2018; Multiparametric MRI for organ quality assessment in a porcine ex-vivo lung perfusion system. PLoS One. 13:e0209103. DOI: 10.1371/journal.pone.0209103. PMID: 30589907. PMCID: PMC6307703.
Article39. Ayyat KS, Okamoto T, Niikawa H, Sakanoue I, Dugar S, Latifi SQ, et al. 2020; A CLUE for better assessment of donor lungs: novel technique in clinical ex vivo lung perfusion. J Heart Lung Transplant. 39:1220–7. DOI: 10.1016/j.healun.2020.07.013. PMID: 32773324.
Article40. Iske J, Hinze CA, Salman J, Haverich A, Tullius SG, Ius F. 2021; The potential of ex vivo lung perfusion on improving organ quality and ameliorating ischemia reperfusion injury. Am J Transplant. 21:3831–9. DOI: 10.1111/ajt.16784. PMID: 34355495. PMCID: PMC8925042.
Article41. Bunsow E, Los-Arcos I, Martin-Gómez MT, Bello I, Pont T, Berastegui C, et al. 2020; Donor-derived bacterial infections in lung transplant recipients in the era of multidrug resistance. J Infect. 80:190–6. DOI: 10.1016/j.jinf.2019.12.006. PMID: 31843689.
Article42. Snell G, Hiho S, Levvey B, Sullivan L, Westall G. 2019; Consequences of donor-derived passengers (pathogens, cells, biological molecules and proteins) on clinical outcomes. J Heart Lung Transplant. 38:902–6. DOI: 10.1016/j.healun.2019.06.019. PMID: 31307786.
Article43. Tanaka S, Gauthier JM, Terada Y, Takahashi T, Li W, Hashimoto K, et al. 2021; Bacterial products in donor airways prevent the induction of lung transplant tolerance. Am J Transplant. 21:353–61. DOI: 10.1111/ajt.16256. PMID: 32786174. PMCID: PMC7775268.
Article44. Nakajima D, Cypel M, Bonato R, Machuca TN, Iskender I, Hashimoto K, et al. 2016; Ex vivo perfusion treatment of infection in human donor lungs. Am J Transplant. 16:1229–37. DOI: 10.1111/ajt.13562. PMID: 26730551.
Article45. Zinne N, Krueger M, Hoeltig D, Tuemmler B, Boyle EC, Biancosino C, et al. 2018; Treatment of infected lungs by ex vivo perfusion with high dose antibiotics and autotransplantation: a pilot study in pigs. PLoS One. 13:e0193168. DOI: 10.1371/journal.pone.0193168. PMID: 29505574. PMCID: PMC5837087.
Article46. Michaelsen VS, Ribeiro RV, Ali A, Wang A, Gazzalle A, Keshavjee S, et al. 2022; Safety of continuous 12-hour delivery of antimicrobial doses of inhaled nitric oxide during ex vivo lung perfusion. J Thorac Cardiovasc Surg. 163:841–9. DOI: 10.1016/j.jtcvs.2020.11.150. PMID: 33478833.47. Galasso M, Feld JJ, Watanabe Y, Pipkin M, Summers C, Ali A, et al. 2019; Inactivating hepatitis C virus in donor lungs using light therapies during normothermic ex vivo lung perfusion. Nat Commun. 10:481. DOI: 10.1038/s41467-018-08261-z. PMID: 30696822. PMCID: PMC6351537.
Article48. Lin H, Chen M, Tian F, Tikkanen J, Ding L, Cheung HY, et al. 2018; α1-Anti-trypsin improves function of porcine donor lungs during ex-vivo lung perfusion. J Heart Lung Transplant. 37:656–66. DOI: 10.1016/j.healun.2017.09.019. PMID: 29153638.49. Ku TJ, Ribeiro RV, Ferreira VH, Galasso M, Keshavjee S, Kumar D, et al. 2020; Ex-vivo delivery of monoclonal antibody (rituximab) to treat human donor lungs prior to transplantation. EBioMedicine. 60:102994. DOI: 10.1016/j.ebiom.2020.102994. PMID: 32950000. PMCID: PMC7501077.
Article50. Haam S, Noda K, Philips BJ, Harano T, Sanchez PG, Shigemura N. 2020; Cyclosporin A administration during ex vivo lung perfusion preserves lung grafts in rat transplant model. Transplantation. 104:e252–9. DOI: 10.1097/TP.0000000000003237. PMID: 32217944.
Article51. van Zanden JE, Leuvenink HG, Verschuuren EA, Veldhuis ZJ, Ottens PJ, Erasmus ME, et al. 2021; Ex vivo perfusion with methylprednisolone attenuates brain death-induced lung injury in rats. Transplant Direct. 7:e682. DOI: 10.1097/TXD.0000000000001141. PMID: 33748411. PMCID: PMC7969243.
Article52. Yeung JC, Wagnetz D, Cypel M, Rubacha M, Koike T, Chun YM, et al. 2012; Ex vivo adenoviral vector gene delivery results in decreased vector-associated inflammation pre- and post-lung transplantation in the pig. Mol Ther. 20:1204–11. DOI: 10.1038/mt.2012.57. PMID: 22453765. PMCID: PMC3369301.
Article53. Figueiredo C, Carvalho Oliveira M, Chen-Wacker C, Jansson K, Höffler K, Yuzefovych Y, et al. 2019; Immunoengineering of the vascular endothelium to silence MHC expression during normothermic ex vivo lung perfusion. Hum Gene Ther. 30:485–96. DOI: 10.1089/hum.2018.117. PMID: 30261752.54. Alraies MC, Eckman P. 2014; Adult heart transplant: indications and outcomes. J Thorac Dis. 6:1120–8.55. Brink JG, Hassoulas J. 2009; The first human heart transplant and further advances in cardiac transplantation at Groote Schuur Hospital and the University of Cape Town - with reference to: the operation. A human cardiac transplant: an interim report of a successful operation performed at Groote Schuur Hospital, Cape Town. Cardiovasc J Afr. 20:31–5.56. Hessel FP. 2021; Overview of the socio-economic consequences of heart failure. Cardiovasc Diagn Ther. 11:254–62. DOI: 10.21037/cdt-20-291. PMID: 33708497. PMCID: PMC7944217.57. Lund LH, Edwards LB, Kucheryavaya AY, Dipchand AI, Benden C, Christie JD, et al. 2013; The registry of the International Society for Heart and Lung Transplantation: thirtieth official adult heart transplant report-2013; focus theme: age. J Heart Lung Transplant. 32:951–64. DOI: 10.1016/j.healun.2013.08.006. PMID: 24054804.
Article58. Javier MF, Javier Delmo EM, Hetzer R. 2021; Evolution of heart transplantation since Barnard's first. Cardiovasc Diagn Ther. 11:171–82. DOI: 10.21037/cdt-20-289. PMID: 33708490. PMCID: PMC7944212.
Article59. Park JJ, Lee CJ, Park SJ, Choi JO, Choi S, Park SM, et al. 2021; Heart failure statistics in Korea, 2020: a report from the Korean Society of Heart Failure. Int J Heart Fail. 3:224–36. DOI: 10.36628/ijhf.2021.0023. PMID: 36262554. PMCID: PMC9536683.
Article60. Kim IC, Youn JC, Kobashigawa JA. 2018; The past, present and future of heart transplantation. Korean Circ J. 48:565–90. DOI: 10.4070/kcj.2018.0189. PMID: 29968430. PMCID: PMC6031715.
Article61. Jacob S, Garg P, Wadiwala I, Yazji JH, Alomari M, Alamouti-fard E, et al. 2022; Strategies for expanding donors pool in heart transplantation. Rev Cardiovasc Med. 23:285. DOI: 10.31083/j.rcm2308285.
Article62. Hameed AM, Hawthorne WJ, Pleass HC. 2017; Advances in organ preservation for transplantation. ANZ J Surg. 87:976–80. DOI: 10.1111/ans.13713. PMID: 27490874.
Article63. Hicks M, Hing A, Gao L, Ryan J, Macdonald PS. 2006; Organ preservation. Methods Mol Biol. 333:331–74. DOI: 10.1385/1-59745-049-9:331. PMID: 16790859.
Article64. Banner NR, Thomas HL, Curnow E, Hussey JC, Rogers CA, Bonser RS, et al. 2008; The importance of cold and warm cardiac ischemia for survival after heart transplantation. Transplantation. 86:542–7. DOI: 10.1097/TP.0b013e31818149b9. PMID: 18724223.
Article65. Russo MJ, Iribarne A, Hong KN, Ramlawi B, Chen JM, Takayama H, et al. 2010; Factors associated with primary graft failure after heart transplantation. Transplantation. 90:444–50. DOI: 10.1097/TP.0b013e3181e6f1eb. PMID: 20622755.
Article66. Ali AA, White P, Xiang B, Lin HY, Tsui SS, Ashley E, et al. 2011; Hearts from DCD donors display acceptable biventricular function after heart transplantation in pigs. Am J Transplant. 11:1621–32. DOI: 10.1111/j.1600-6143.2011.03622.x. PMID: 21749639.
Article67. Boucek MM, Kanakriyeh MS, Mathis CM, Trimm RF 3rd, Bailey LL. 1990; Cardiac transplantation in infancy: donors and recipients. J Pediatr. 116:171–6. DOI: 10.1016/S0022-3476(05)82870-7. PMID: 2299486.
Article68. Pahuja M, Case BC, Molina EJ, Waksman R. 2022; Overview of the FDA's Circulatory System Devices Panel virtual meeting on the TransMedics Organ Care System (OCS) Heart - portable extracorporeal heart perfusion and monitoring system. Am Heart J. 247:90–9. DOI: 10.1016/j.ahj.2022.02.003. PMID: 35150637.
Article69. Fedalen PA, Piacentino V, Popovich DA. 2000; Protection and resuscitation of non-beating hearts: a potential approach to increase the donor pool. J Heart Lung Transplant. 19:97.70. Hassanein WH, Zellos L, Tyrrell TA, Healey NA, Crittenden MD, Birjiniuk V, et al. 1998; Continuous perfusion of donor hearts in the beating state extends preservation time and improves recovery of function. J Thorac Cardiovasc Surg. 116:821–30. DOI: 10.1016/S0022-5223(98)00452-8. PMID: 9806389.
Article71. García Sáez D, Zych B, Sabashnikov A, Bowles CT, De Robertis F, Mohite PN, et al. 2014; Evaluation of the organ care system in heart transplantation with an adverse donor/recipient profile. Ann Thorac Surg. 98:2099–105. DOI: 10.1016/j.athoracsur.2014.06.098. PMID: 25443013.
Article72. Mohite P, Husain M, Saez DG, Penn S, Maunz O, Simon A. 2020. Utilization of TransMedics organ care system for preservation of the donor heart [Internet]. CTSNeT;Available from: https://doi.org/10.25373/ctsnet.13374056. cited 2023 Dec 23. DOI: 10.25373/ctsnet.13374056.
Article73. Bryner BS, Schroder JN, Milano CA. 2021; Heart transplant advances: ex vivo organ-preservation systems. JTCVS Open. 8:123–7. DOI: 10.1016/j.xjon.2021.04.020. PMID: 36004090. PMCID: PMC9390583.
Article74. Rojas SV, Avsar M, Ius F, Schibilsky D, Kaufeld T, Benk C, et al. 2022; Ex-vivo preservation with the organ care system in high risk heart transplantation. Life (Basel). 12:247. DOI: 10.3390/life12020247. PMID: 35207534. PMCID: PMC8877453.
Article75. Beuth J, Falter F, Pinto Ribeiro RV, Badiwala M, Meineri M. 2019; New strategies to expand and optimize heart donor pool: ex vivo heart perfusion and donation after circulatory death: a review of current research and future trends. Anesth Analg. 128:406–13. DOI: 10.1213/ANE.0000000000003919. PMID: 30531220.
Article76. Stamp NL, Shah A, Vincent V, Wright B, Wood C, Pavey W, et al. 2015; Successful heart transplant after ten hours out-of-body time using the TransMedics Organ Care System. Heart Lung Circ. 24:611–3. DOI: 10.1016/j.hlc.2015.01.005. PMID: 25697385.
Article77. Pinnelas R, Kobashigawa JA. 2022; Ex vivo normothermic perfusion in heart transplantation: a review of the TransMedics® Organ Care System. Future Cardiol. 18:5–15. DOI: 10.2217/fca-2021-0030. PMID: 34503344.
Article78. White CW, Messer SJ, Large SR, Conway J, Kim DH, Kutsogiannis DJ, et al. 2018; Transplantation of hearts donated after circulatory death. Front Cardiovasc Med. 5:8. DOI: 10.3389/fcvm.2018.00008. PMID: 29487855. PMCID: PMC5816942.
Article79. Ghodsizad A, Bordel V, Ungerer M, Karck M, Bekeredjian R, Ruhparwar A. 2012; Ex vivo coronary angiography of a donor heart in the organ care system. Heart Surg Forum. 15:E161–3. DOI: 10.1532/HSF98.20111146. PMID: 22698606.
Article80. Bishawi M, Roan JN, Milano CA, Daneshmand MA, Schroder JN, Chiang Y, et al. 2019; A normothermic ex vivo organ perfusion delivery method for cardiac transplantation gene therapy. Sci Rep. 9:8029. DOI: 10.1038/s41598-019-43737-y. PMID: 31142753. PMCID: PMC6541710.
Article81. Radakovic D, Karimli S, Penov K, Schade I, Hamouda K, Bening C, et al. 2020; First clinical experience with the novel cold storage SherpaPak™ system for donor heart transportation. J Thorac Dis. 12:7227–35. DOI: 10.21037/jtd-20-1827. PMID: 33447411. PMCID: PMC7797872.
Article82. D'Alessandro D, Philpott J, Boeve T, Pham S, Zuckermann A. 2021; First report of the GUARDIAN Registry: an international consortium examining the effect of controlled hypothermic preservation in heart transplantation. J Heart Lung Transplant. 40(4 Suppl):S127. DOI: 10.1016/j.healun.2021.01.398.83. Leacche M, Philpott J, Pham S, Shudo Y, Kawabori M, Jacobs J, et al. 2022; US multi-center analysis of the Global Utilization and Registry Database for Improved Heart Preservation (GUARDIAN) registry: 1-year transplant survival analysis. J Heart Lung Transplant. 41(4 Suppl):S30–1. DOI: 10.1016/j.healun.2022.01.067.
Article84. Zuckermann A, Leacche M, Philpott J, Pham S, Shudo Y, Bustamante-Munguira J, et al. 2022; Second report of the GUARDIAN registry: an international consortium examining effect of controlled hypothermic preservation in heart transplantation. J Heart Lung Transplant. 41(4 Suppl):S477. DOI: 10.1016/j.healun.2022.01.1204.85. Isath A, Ohira S, Levine A, Pan S, Aggarwal-Gupta C, Lanier GM, et al. 2023; Ex vivo heart perfusion for cardiac transplantation allowing for prolonged perfusion time and extension of distance traveled for procurement of donor hearts: an initial experience in the United States. Transplant Direct. 9:e1455. DOI: 10.1097/TXD.0000000000001455. PMID: 36845853. PMCID: PMC9949869.
Article86. Schroder JN, Shah A, Pretorius V, Smith J, Daneshmand M, Geirsson A, et al. 2022; Expanding heart transplants from donors after circulatory death (DCD) - results of the first randomized controlled trial using the Organ Care System (OCS™) heart - (OCS DCD heart trial). J Heart Lung Transplant. 41(4 Suppl):S72. DOI: 10.1016/j.healun.2022.01.165.
Article87. Ardehali A, Esmailian F, Deng M, Soltesz E, Hsich E, Naka Y, et al. 2015; Ex-vivo perfusion of donor hearts for human heart transplantation (PROCEED II): a prospective, open-label, multicentre, randomised non-inferiority trial. Lancet. 385:2577–84. DOI: 10.1016/S0140-6736(15)60261-6. PMID: 25888086.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ex Vivo Lung Perfusion in Lung Transplantation
- Ex vivo cholangioscopy in liver grafts: a novel technique to assess the biliary tree during organ preservation and machine perfusion: a experimental non-clinical study
- Ex vivo Lung Perfusion Model in Lung Transplantation
- Cold but not too cold: advances in hypothermic and normothermic organ perfusion
- Ex Vivo Lung Perfusion of Cardiac-death Donor Lung in Pigs