Clin Orthop Surg.
2010 Jun;2(2):98-104. 10.4055/cios.2010.2.2.98.
Prognostic Factors That Affect the Surgical Outcome of the Laminoplasty in Cervical Spondylotic Myelopathy
- Affiliations
-
- 1Department of Orthopaedic Surgery, Chungnam National University School of Medicine, Daejeon, Korea. jsahn@cnu.ac.kr
- KMID: 1719336
- DOI: http://doi.org/10.4055/cios.2010.2.2.98
Abstract
- BACKGROUND
This study examined the prognostic factors that affect the surgical outcome of laminoplasty in cervical spondylotic myelopathy patients by comparative analysis.
METHODS
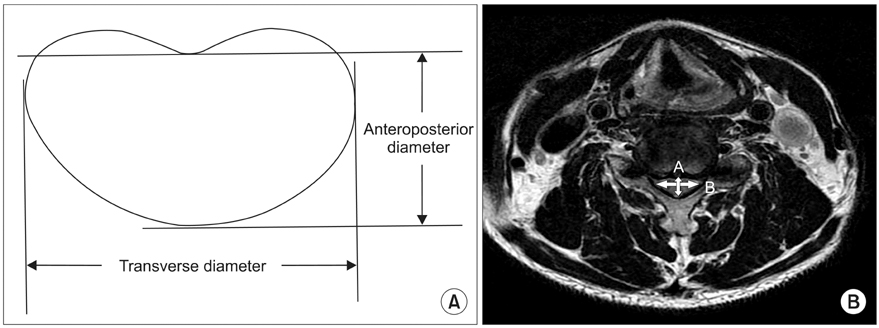
Thirty nine patients, 26 males and 13 females, who were treated with laminoplasty for cervical myelopathy from September 2004 to March 2008 and followed up for 12 months or longer, were enrolled in this study. The mean age of the subjects was 62.4 years (range, 37 to 77 years). The patients' age, number of surgical segments, spinal cord compression ratio, segment number, level, localized marginal pattern of high signal intensity within the spinal cord in the T2 image, preoperative Japanese Orthopaedic Association Scoring System (JOA) score with the recovery ratio were compared respectively. The JOA score was used for an objective assessment of the patients' preoperative and postoperative clinical status. The recovery ratios of surgery were graded using the Hirabayashi equation. Statistical analysis was carried out using Pearson correlation analysis.
RESULTS
The patients' JOA score increased from a preoperative score of 11.1 (range, 5 to 16) to a postoperative score of 14.9 (range, 7 to 17). The average recovery ratio was 65.8% (range, 0 to 100%). The number of segments with high signal changes in the T2 image, a localized marginal pattern with high signal change, signal intensity changes in the upper cervical spinal cord were inversely associated with the recovery ratio, whereas the spinal cord compression ratio showed a significant positive correlation. However, the currently known prognostic factors, such as number of surgical segment, age, and preoperative JOA score, showed no statistically significant correlation.
CONCLUSIONS
The number of segments, localized marginal pattern, rostral location of signal intensity c hanges with a high signal change in the T2 image and a low spinal cord compression ratio in cervical spondylotic myelopathy patients treated by laminoplasty can indicate a poor prognosis.
MeSH Terms
Figure
Reference
-
1. Al-Mefty O, Harkey HL, Marawi I, et al. Experimental chronic compressive cervical myelopathy. J Neurosurg. 1993. 79(4):550–561.
Article2. Kohno K, Kumon Y, Oka Y, Matsui S, Ohue S, Sakaki S. Evaluation of prognostic factors following expansive laminoplasty for cervical spinal stenotic myelopathy. Surg Neurol. 1997. 48(3):237–245.
Article3. Koyanagi T, Hirabayashi K, Satomi K, Toyama Y, Fujimura Y. Predictability of operative results of cervical compression myelopathy based on preoperative computed tomographic myelography. Spine (Phila Pa 1976). 1993. 18(14):1958–1963.
Article4. Hirabayashi K, Watanabe K, Wakano K, Suzuki N, Satomi K, Ishii Y. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine (Phila Pa 1976). 1983. 8(7):693–699.
Article5. Fujiwara K, Yonenobu K, Ebara S, Yamashita K, Ono K. The prognosis of surgery for cervical compression myelopathy: an analysis of the factors involved. J Bone Joint Surg Br. 1989. 71(3):393–398.
Article6. Lee KB, Park IH, Song KW, Lee EJ, Lee JS. Surgical treatment of cervical spondylotic myelopathy. J Korean Orthop Assoc. 1997. 32(5):1181–1188.
Article7. Kim YT, Lee CS, Lee SW, Choi DS, Lee SW. Prognostic factors affecting the results of the surgery for cervical spondylotic myelopathy. J Korean Soc Spine Surg. 2005. 12(4):255–261.
Article8. Handa Y, Kubota T, Ishii H, Sato K, Tsuchida A, Arai Y. Evaluation of prognostic factors and clinical outcome in elderly patients in whom expansive laminoplasty is performed for cervical myelopathy due to multisegmental spondylotic canal stenosis. A retrospective comparison with younger patients. J Neurosurg. 2002. 96:2 Suppl. 173–179.
Article9. Tanaka J, Seki N, Tokimura F, Doi K, Inoue S. Operative results of canal-expansive laminoplasty for cervical spondylotic myelopathy in elderly patients. Spine (Phila Pa 1976). 1999. 24(22):2308–2312.
Article10. Hamburger C, Buttner A, Uhl E. The cross-sectional area of the cervical spinal canal in patients with cervical spondylotic myelopathy: correlation of preoperative and postoperative area with clinical symptoms. Spine (Phila Pa 1976). 1997. 22(17):1990–1994.
Article11. Fujimura Y, Nishi Y, Nakamura M. Dorsal shift and expansion of the spinal cord after expansive open-door laminoplasty. J Spinal Disord. 1997. 10(4):282–287.
Article12. Ogino H, Tada K, Okada K, et al. Canal diameter, anteroposterior compression ratio, and spondylotic myelopathy of the cervical spine. Spine (Phila Pa 1976). 1983. 8(1):1–15.
Article13. Nakamura M, Fujimura Y. Magnetic resonance imaging of the spinal cord in cervical ossification of the posterior longitudinal ligament: can it predict surgical outcome? Spine (Phila Pa 1976). 1998. 23(1):38–40.
Article14. Ramanauskas WL, Wilner HI, Metes JJ, Lazo A, Kelly JK. MR imaging of compressive myelomalacia. J Comput Assist Tomogr. 1989. 13(3):399–404.
Article15. Matsuda Y, Miyazaki K, Tada K, et al. Increased MR signal intensity due to cervical myelopathy: analysis of 29 surgical cases. J Neurosurg. 1991. 74(6):887–892.16. Okada Y, Ikata T, Yamada H, Sakamoto R, Katoh S. Magnetic resonance imaging study on the results of surgery for cervical compression myelopathy. Spine (Phila Pa 1976). 1993. 18(14):2024–2029.
Article17. Morio Y, Yamamoto K, Kuranobu K, Murata M, Tuda K. Does increased signal intensity of the spinal cord on MR images due to cervical myelopathy predict prognosis? Arch Orthop Trauma Surg. 1994. 113(5):254–259.
Article18. Yone K, Sakou T, Yanase M, Ijiri K. Preoperative and postoperative magnetic resonance image evaluations of the spinal cord in cervical myelopathy. Spine (Phila Pa 1976). 1992. 17:10 Suppl. S388–S392.
Article19. Morio Y, Teshima R, Nagashima H, Nawata K, Yamasaki D, Nanjo Y. Correlation between operative outcomes of cervical compression myelopathy and mri of the spinal cord. Spine (Phila Pa 1976). 2001. 26(11):1238–1245.
Article20. Chen CJ, Lyu RK, Lee ST, Wong YC, Wang LJ. Intramedullary high signal intensity on T2-weighted MR images in cervical spondylotic myelopathy: prediction of prognosis with type of intensity. Radiology. 2001. 221(3):789–794.
Article21. Flanders AE, Spettell CM, Friedman DP, Marino RJ, Herbison GJ. The relationship between the functional abilities of patients with cervical spinal cord injury and the severity of damage revealed by MR imaging. AJNR Am J Neuroradiol. 1999. 20(5):926–934.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Factors Affecting Surgical Results in Cervical Spondylotic Myelopathy
- Cervical spondylotic myelopathy and radiculopathy: a stepwise approach and comparative analysis of surgical outcomes: a narrative review of recent literature
- Predictors of Outcome in Patients with Cervical Spondylotic Myelopathy Undergoing Unilateral Open-Door Laminoplasty
- Prognostic Factors Affecting the Surgical Outcome of the Cervical Myelopathy
- Changes in Cervical Spine Range of Motion after Laminoplasty in Cervical Spondylotic Myelopathy