J Korean Med Sci.
2007 Oct;22(5):832-838. 10.3346/jkms.2007.22.5.832.
Easy Diagnosis of Asthma: Computer-Assisted, Symptom-Based Diagnosis
- Affiliations
-
- 1Department of Internal Medicine, Chung-Ang University College of Medicine, Seoul, Korea.
- 2Department of Internal Medicine, Konkuk University College of Medicine, Seoul, Korea.
- 3Department of Internal Medicine, Ilsan-paik Hospital, Inje University College of Medicine, Goyang, Korea.
- 4Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea.
- 5Department of Pediatrics, Konkuk University College of Medicine, Seoul, Korea.
- 6Department of Pediatrics, Inje University College of Medicine, Seoul, Korea.
- 7Department of Pediatrics, Hanyang University College of Medicine, Hanyang University Guri Hospital, Guri, Korea.
- 8Department of Pediatrics, Kyunghee University College of Medicine, Seoul, Korea.
- 9Department of Pediatrics, Soonchunhyang University College of Medicine, Seoul, Korea.
- 10Department of Internal Medicine, Sungae General Hospital, Seoul, Korea.
- 11Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 12Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea. shcho@plaza.snu.ac.kr
- KMID: 1713289
- DOI: http://doi.org/10.3346/jkms.2007.22.5.832
Abstract
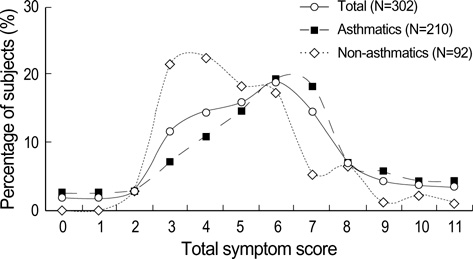
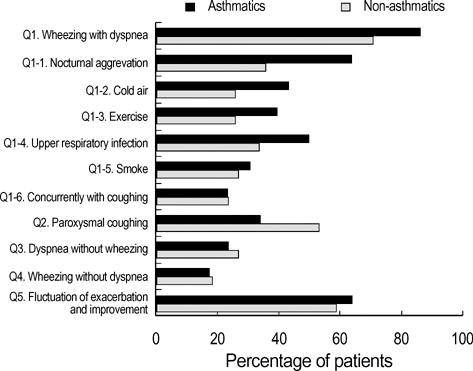
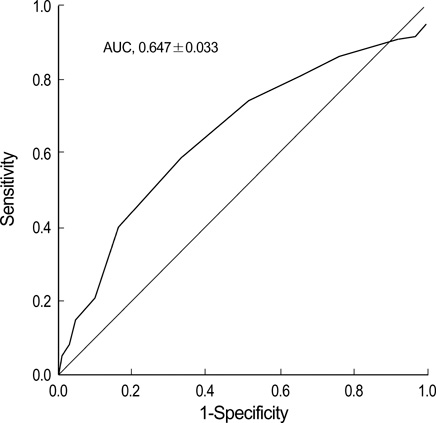
- Diagnosis of asthma is often challenging in primary-care physicians due to lack of tools measuring airway obstruction and variability. Symptom-based diagnosis of asthma utilizing objective diagnostic parameters and appropriate software would be useful in clinical practice. A total of 302 adult patients with respiratory symptoms responded to a questionnaire regarding asthma symptoms and provoking factors. Questions were asked and recorded by physicians into a computer program. A definite diagnosis of asthma was made based on a positive response to methacholine bronchial provocation or bronchodilator response (BDR) testing. Multivariate logistic regression analysis was used to evaluate the significance of questionnaire responses in terms of discriminating asthmatics. Asthmatic patients showed higher total symptom scores than non-asthmatics (mean 5.93 vs. 4.93; p<0.01). Multivariate logistic regression analysis identified that response to questions concerning the following significantly discriminated asthmatics; wheezing with dyspnea, which is aggravated at night, and by exercise, cold air, and upper respiratory infection. Moreover, the presence of these symptoms was found to agree significantly with definite diagnosis of asthma (by kappa statistics). Receiver-operating characteristic curve analysis revealed that the diagnostic accuracy of symptom-based diagnosis was high with an area under the curve of 0.647+/-0.033. Using a computer-assisted symptom-based diagnosis program, it is possible to increase the accuracy of diagnosing asthma in general practice, when the facilities required to evaluate airway hyperresponsiveness or BDR are unavailable.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Past, Present, and Future of Allergy in Korea
You-Young Kim
Allergy Asthma Immunol Res. 2010;2(3):155-164. doi: 10.4168/aair.2010.2.3.155.
Reference
-
1. The International Study of Asthma and Allergies in Childhood (ISAAC) Steering Committee. Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC. Lancet. 1998. 351:1225–1232.2. Kim YK, Kim SH, Tak YJ, Jee YK, Lee BJ, Kim SH, Park HW, Jung JW, Bahn JW, Chang YS, Choi DC, Chang SI, Min KU, Kim YY, Cho SH. High prevalence of current asthma and active smoking effect among the elderly. Clin Exp Allergy. 2002. 32:1706–1712.
Article3. Singh M. The burden of asthma in children: an Asian perspective. Paediatr Respir Rev. 2005. 6:14–19.
Article4. Sennhauser FH, Braun-Fahrlander C, Wildhaber JH. The burden of asthma in children: a european perspective. Paediatr Respir Rev. 2005. 6:2–7.
Article5. Beasley R. The burden of asthma with specific reference to the united states. J Allergy Clin Immunol. 2002. 109:5 suppl. S482–S489.
Article6. Helms PJ. Issues and unmet needs in pediatric asthma. Pediatr Pulmonol. 2000. 30:159–165.
Article7. Enright PL, McClelland RL, Newman AB, Gottlieb DJ, Lebowitz MD. Underdiagnosis and undertreatment of asthma in the elderly. Cardiovascular health study research group. Chest. 1999. 116:603–613.8. Global initiative for asthma 2002. Update from: Global strategy for asthma management and prevention nhlbi/who workshop report 1995. 2002. Bethesda, md.: National institutes of health;(dhhs publication no. (NIH) 02-3659.).9. Van Schoor J, Joos GF, Pauwels RA. Indirect bronchial hyperresponsiveness in asthma: Mechanisms, pharmacology and implications for clinical research. Eur Respir J. 2000. 16:514–533.
Article10. Burney P, Chinn S. Developing a new questionnaire for measuring the prevalence and distribution of asthma. Chest. 1987. 91:6 suppl. 79S–83S.
Article11. Burney PG, Laitinen LA, Perdrizet S, Huckauf H, Tattersfield AE, Chinn S, Poisson N, Heeren A, Britton JR, Jones T. Validity and repeatability of the IUATLD (1984) bronchial symptoms questionnaire: An international comparison. Eur Respir J. 1989. 2:940–945.12. Venables KM, Farrer N, Sharp L, Graneek BJ, Newman Taylor AJ. Respiratory symptoms questionnaire for asthma epidemiology: Validity and reproducibility. Thorax. 1993. 48:214–219.
Article13. Bai J, Peat JK, Berry G, Marks GB, Woolcock AJ. Questionnaire items that predict asthma and other respiratory conditions in adults. Chest. 1998. 114:1343–1348.
Article14. Toren K, Brisman J, Jarvholm B. Asthma and asthma-like symptoms in adults assessed by questionnaires. A literature review. Chest. 1993. 104:600–608.15. Shaw RA, Crane J, Pearce N, Burgess CD, Bremner P, Woodman K, Beasley R. Comparison of a video questionnaire with the iuatld written questionnaire for measuring asthma prevalence. Clin Exp Allergy. 1992. 22:561–568.
Article16. Kable S, Henry R, Sanson-Fisher R, Ireland M, Corkrey R, Cockburn J. Childhood asthma: can computers aid detection in general practice? Br J Gen Pract. 2001. 51:112–116.17. Juniper EF, O'Byrne PM, Guyatt GH, Ferrie PJ, King DR. Development and validation of a questionnaire to measure asthma control. Eur Respir J. 1999. 14:902–907.
Article18. Juniper EF, Norman GR, Cox FM, Roberts JN. Comparison of the standard gamble, rating scale, aqlq and sf-36 for measuring quality of life in asthma. Eur Respir J. 2001. 18:38–44.
Article19. Frank TL, Frank PI, McNamee R, Wright T, Hannaford P, Morrison J, Hirsch S, Pickering CA. Assessment of a simple scoring system applied to a screening questionnaire of asthma in children aged 5-15 yrs. Eur Respir J. 1999. 14:1190–1197.20. Hirsch S, Frank TL, Shapiro JL, Hazell ML, Frank PI. Development of a questionnaire weighted scoring system to target diagnostic examinations for asthma in adults: A modelling study. BMC Fam Pract. 2004. 5:30.
Article21. Frank PI, Frank TL, Cropper J, Hirsch S, Niven RM, Hannaford P, McNamee R. The use of a screening questionnaire to identify children with likely asthma. Br J Gen Pract. 2001. 51:117–120.22. Crapo RO, Casaburi R, Coates AL, Enright PL, Hankinson JL, Irvin CG, MacIntyre NR, McKay RT, Wanger JS, Anderson SD, Cockcroft DW, Fish JE, Sterk PJ. Guidelines for methacholine and exercise challenge testing-1999. This official statement of the American Thoracic Society was adopted by the ATS board of directors, July 1999. Am J Respir Crit Care Med. 2000. 161:309–329.23. American thoracic society. Lung function testing: Selection of reference values and interpretative strategies. Am Rev Respir Dis. 1991. 144:1202–1218.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Computer-aided polyp characterization in colonoscopy: sufficient performance or not?
- The Recent Progress in Quantitative Medical Image Analysis for Computer Aided Diagnosis Systems
- Validation of a smartphone-based, computer-assisted sperm analysis system compared with laboratory-based manual microscopic semen analysis and computer-assisted semen analysis
- Computer-Assisted Total Hip Arthroplasty
- A Case of Spontaneous Pneumomediastinum during an Acute Asthma Attack