Korean J Gastroenterol.
2013 Dec;62(6):370-374. 10.4166/kjg.2013.62.6.370.
A Case of Intestinal Tuberculosis with Perianal Fistula Diagnosed after 30 Years
- Affiliations
-
- 1Department of Internal Medicine, Kosin University College of Medicine, Busan, Korea. moonone70@hanmail.net
- KMID: 1711294
- DOI: http://doi.org/10.4166/kjg.2013.62.6.370
Abstract
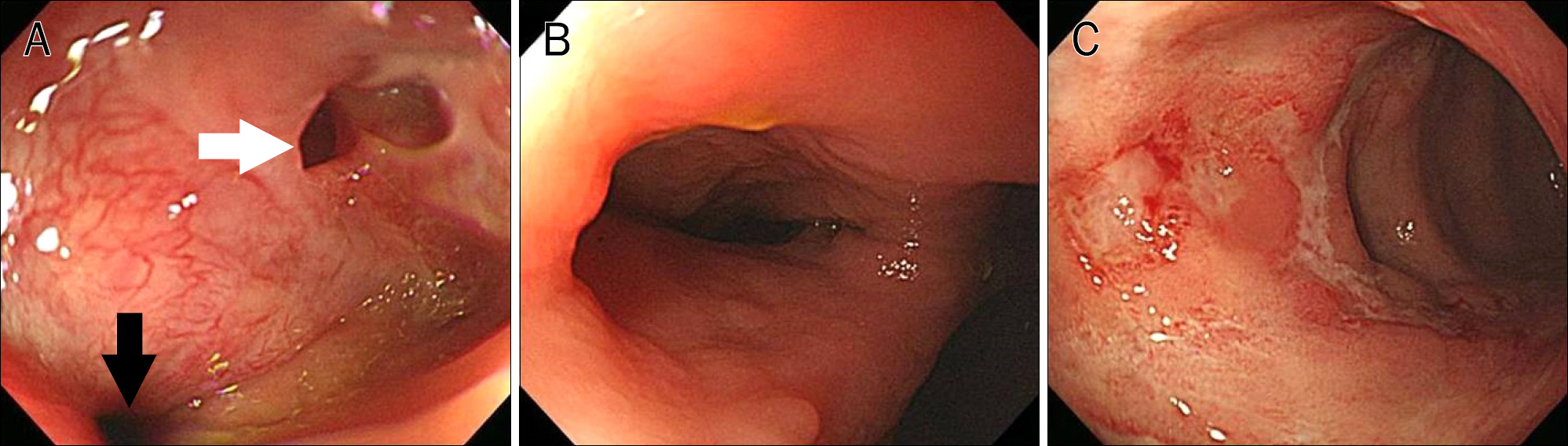
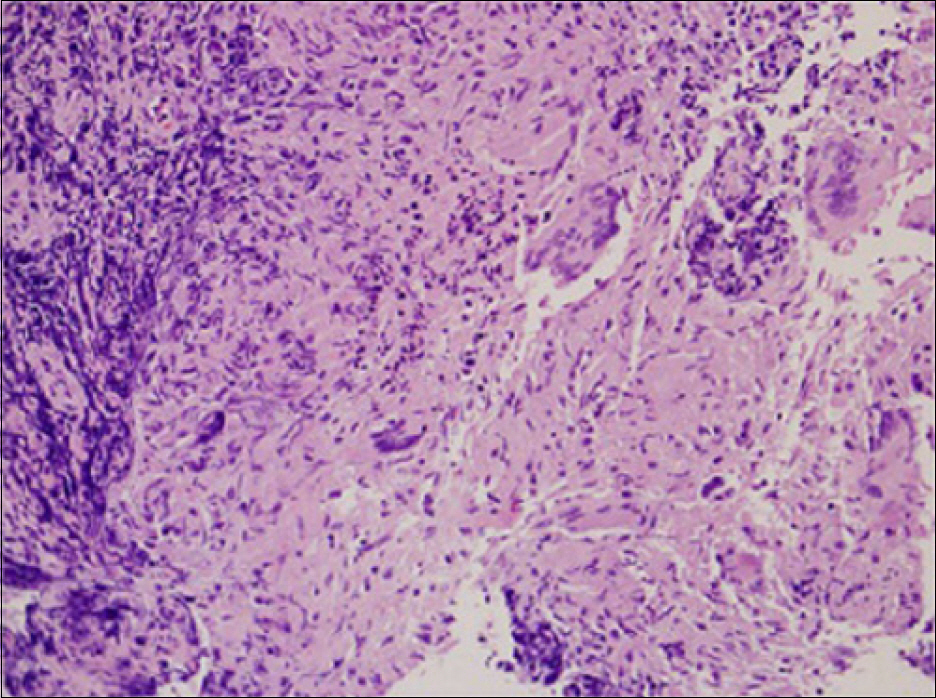
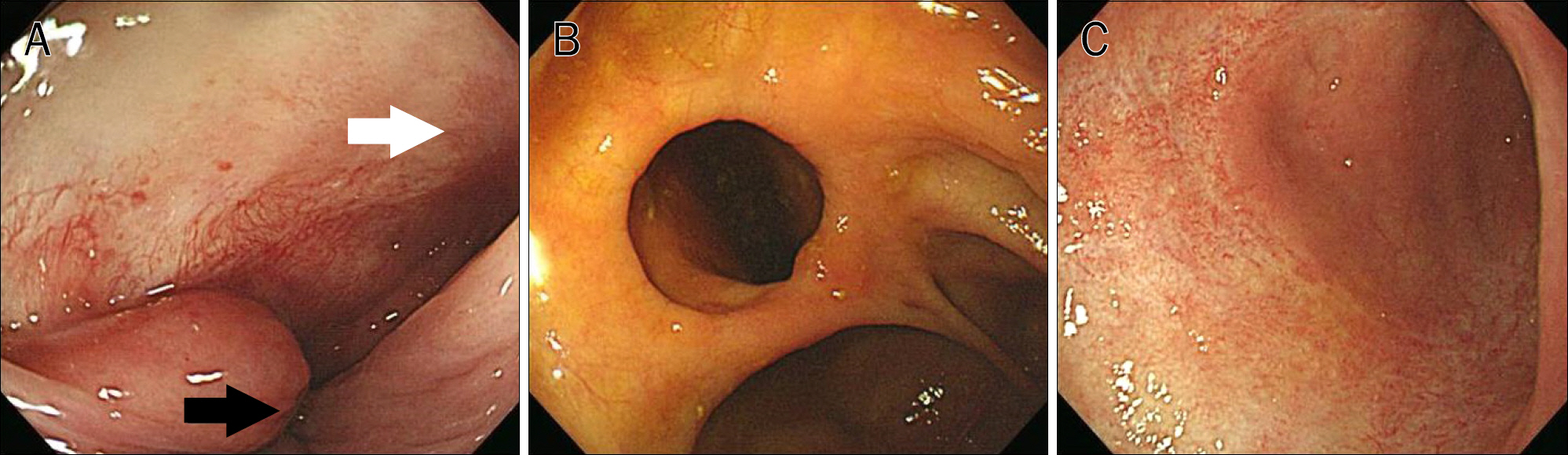
- Tuberculosis can occur anywhere in the gastrointestinal tract. However, anorectal tuberculosis has rarely been reported. A 46-years-old male presented with abdominal pain and perianal discharge of 30 years' duration. The patient had received operations for anal fistula and inflammation three times. Although he had been taking mesalazine for the past three years after being diagnosed with Crohn's disease, his symptoms persisted. Colonoscopy performed at our hospital revealed cicatricial change of ileocecal valve and diffuse ulcer scar with mild luminal narrowing of the ascending, transverse, and descending colon without active lesions. Multiple large irregular active ulcers were observed in the distal sigmoid and proximal rectum. An anal fistula opening with much yellowish discharge and background ulcer scar was observed in the anal canal. However, cobble-stone appearance and pseudopolyposis were not present. Therefore, we clinically diagnosed him as having intestinal tuberculosis with anal fistula and prescribed antituberculosis medications. Follow-up colonoscopy performed 3 months later showed much improved multiple large irregular ulcers in the distal sigmoid colon and proximal rectum along with completely resolved anal fistula without evidence of pus discharge.
MeSH Terms
-
Anal Canal
Anti-Inflammatory Agents, Non-Steroidal/therapeutic use
Antitubercular Agents/therapeutic use
Colon/pathology
Colonoscopy
Crohn Disease/diagnosis/drug therapy
Diagnosis, Differential
Fistula/*diagnosis/pathology
Humans
Ileocecal Valve/physiopathology
Male
Mesalamine/therapeutic use
Middle Aged
Protein C/analysis
Tuberculosis, Gastrointestinal/*diagnosis/drug therapy
Anti-Inflammatory Agents, Non-Steroidal
Antitubercular Agents
Mesalamine
Protein C
Figure
Reference
-
References
1. Bargalló N, Nicolau C, Luburich P, Ayuso C, Cardenal C, Gimeno F. Intestinal tuberculosis in AIDS. Gastrointest Radiol. 1992; 17:115–118.
Article2. Shimamoto H, Hamada K, Higuchi I, et al. Abdominal tuberculosis: peritoneal involvement shown by F-18 FDG PET. Clin Nucl Med. 2007; 32:716–718.
Article3. Lee JN, Ryu DY, Park SH, et al. The usefulness of in vitro interferon-gamma assay for differential diagnosis between intestinal tuberculosis and Crohns disease. Korean J Gastroenterol. 2010; 55:376–383.4. Choi SM, Yang SK, Jung HY, et al. Clinical features of intestinal tuberculosis with special reference to risk factors for complications. Korean J Gastroenterol. 1997; 30:462–471.5. Harland RW, Varkey B. Anal tuberculosis: report of two cases and literature review. Am J Gastroenterol. 1992; 87:1488–1491.6. Yaghoobi R, Khazanee A, Bagherani N, Tajalli M. Gastrointestinal tuberculosis with anal and perianal involvement misdiagnosed as Crohn's disease for 15 years. Acta Derm Venereol. 2011; 91:348–349.7. Dye C. Global epidemiology of tuberculosis. Lancet. 2006; 367:938–940.
Article8. Marshall JB. Tuberculosis of the gastrointestinal tract and peritoneum. Am J Gastroenterol. 1993; 88:989–999.
Article9. Candela F, Serrano P, Arriero JM, Teruel A, Reyes D, Calpena R. Perianal disease of tuberculous origin: report of a case and review of the literature. Dis Colon Rectum. 1999; 42:110–112.10. Chung KM, Kim HS, Park SY, et al. The changes in incidence of Crohn's disease and intestinal tuberculosis in Korea. Korean J Gastroenterol. 2008; 52:351–358.11. Gupta PJ. Ano-perianal tuberculosis. Bratisl Lek Listy. 2005; 106:351–354.12. Ye BD, Yang SK, Kim D, et al. Diagnostic sensitivity of culture and drug resistance patterns in Korean patients with intestinal tuberculosis. Int J Tuberc Lung Dis. 2012; 16:799–804.
Article13. Almadi MA, Ghosh S, Aljebreen AM. Differentiating intestinal tuberculosis from Crohn's disease: a diagnostic challenge. Am J Gastroenterol. 2009; 104:1003–1012.
Article14. Cho JY, Kim YS, Park WW, et al. Clinical features of intestinal tuberculosis in recent ten years (2001–2010). Intest Res. 2011; 9:12–18.
Article15. Lee YJ, Yang SK, Byeon JS, et al. Analysis of colonoscopic findings in the differential diagnosis between intestinal tuberculosis and Crohn's disease. Endoscopy. 2006; 38:592–597.
Article16. Mori T, Sakatani M, Yamagishi F, et al. Specific detection of tuberculosis infection: an interferon-gamma-based assay using new antigens. Am J Respir Crit Care Med. 2004; 170:59–64.17. Kabeer BS, Sikhamani R, Raja A. Comparison of interferon gamma and interferon gamma-inducible protein-10 secretion in HIV-tuberculosis patients. AIDS. 2010; 24:323–325.
Article18. Lee TK, Kim YH, Chang UI, et al. the diagnostic value of polymerase chain reaction in intestinal tuberculosis. Korean J Gastrointest Endosc. 2003; 26:79–83.19. Mukhopadhya A, Samal SC, Mukundan U, et al. Perianal fistulae caused by Mycobacterium fortuitum. J Clin Gastroenterol. 2003; 36:147–148.
Article20. Blumberg HM, Leonard MK Jr, Jasmer RM. Update on the treatment of tuberculosis and latent tuberculosis infection. JAMA. 2005; 293:2776–2784.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- AIDS Diagnosed in the Course of Managing Duodenal Fistula Caused by Tuberculosis: A Case Report
- A Case of Duodenal Fistula Caused by Intestinal Tuberculosis
- A Case of Acute Appendicitis due to Intestinal Stricture after Intestinal Tuberculosis Treatment
- Surgical treatment of perianal fistula in Crohn's disease
- Intestinal Tuberculosis with a Duodenal Fistula