Prog Med Phys.
2014 Jun;25(2):100-109. 10.14316/pmp.2014.25.2.100.
Development of New 4D Phantom Model in Respiratory Gated Volumetric Modulated Arc Therapy for Lung SBRT
- Affiliations
-
- 1Department of Radiation Oncology, Asan Medical Center, University of Ulsan College of Medicine, Korea. jwkwak0301@gmail.com
- 2Department of Biomedical Engineering, Inje University, Kyongnam, Korea.
- KMID: 1708177
- DOI: http://doi.org/10.14316/pmp.2014.25.2.100
Abstract
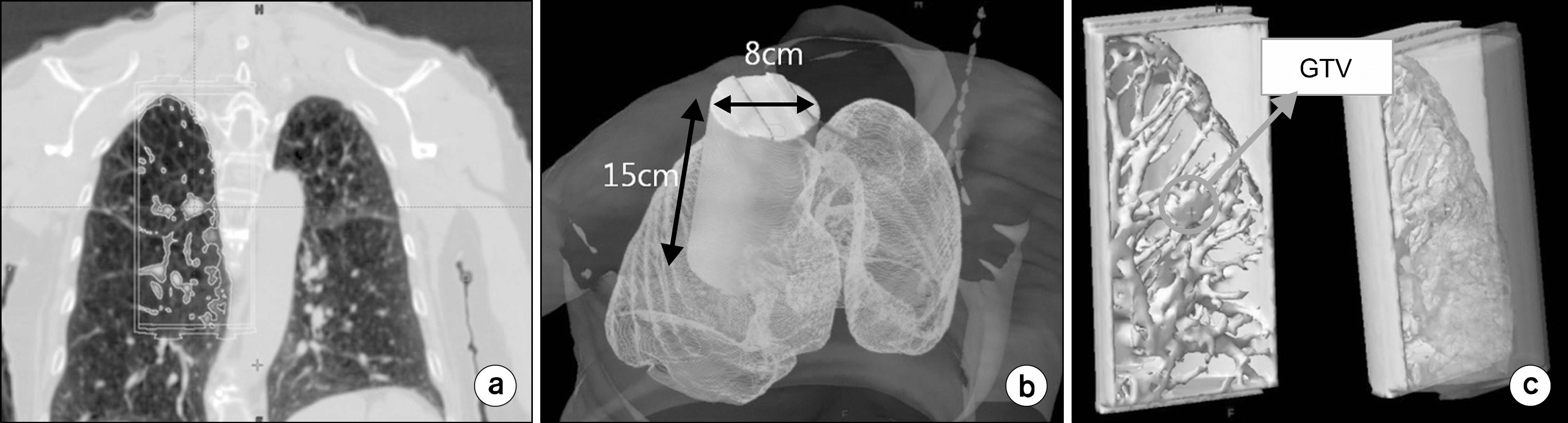
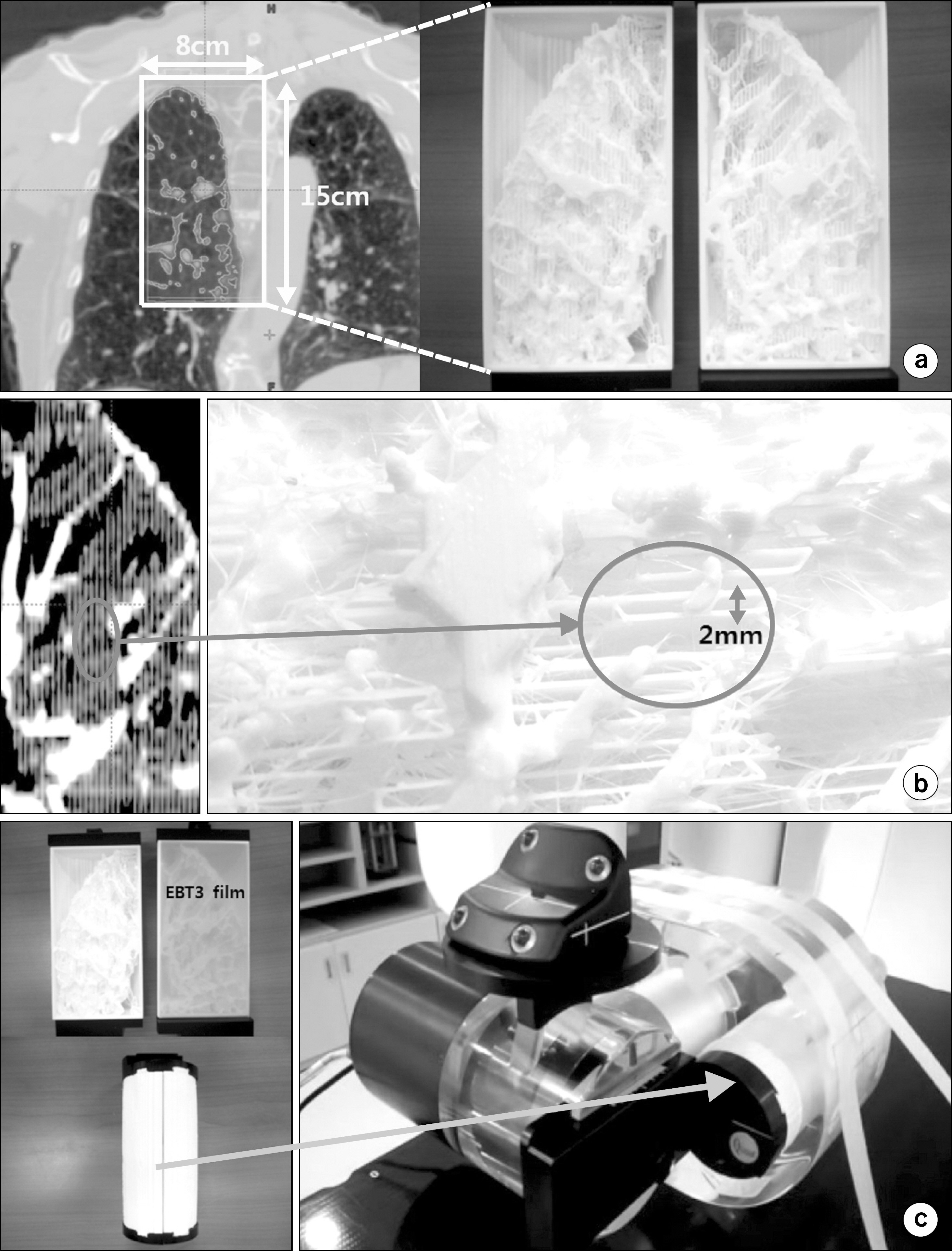
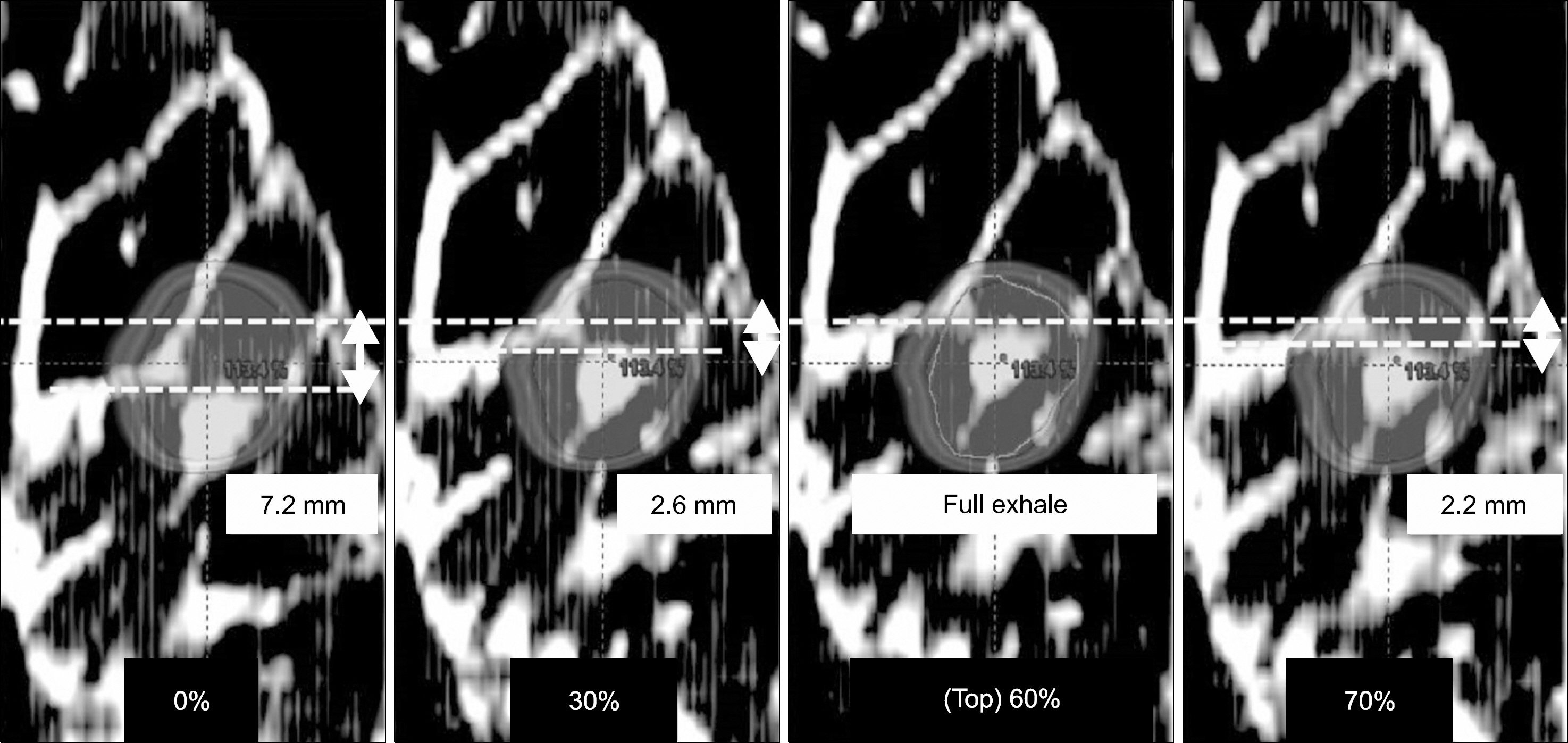
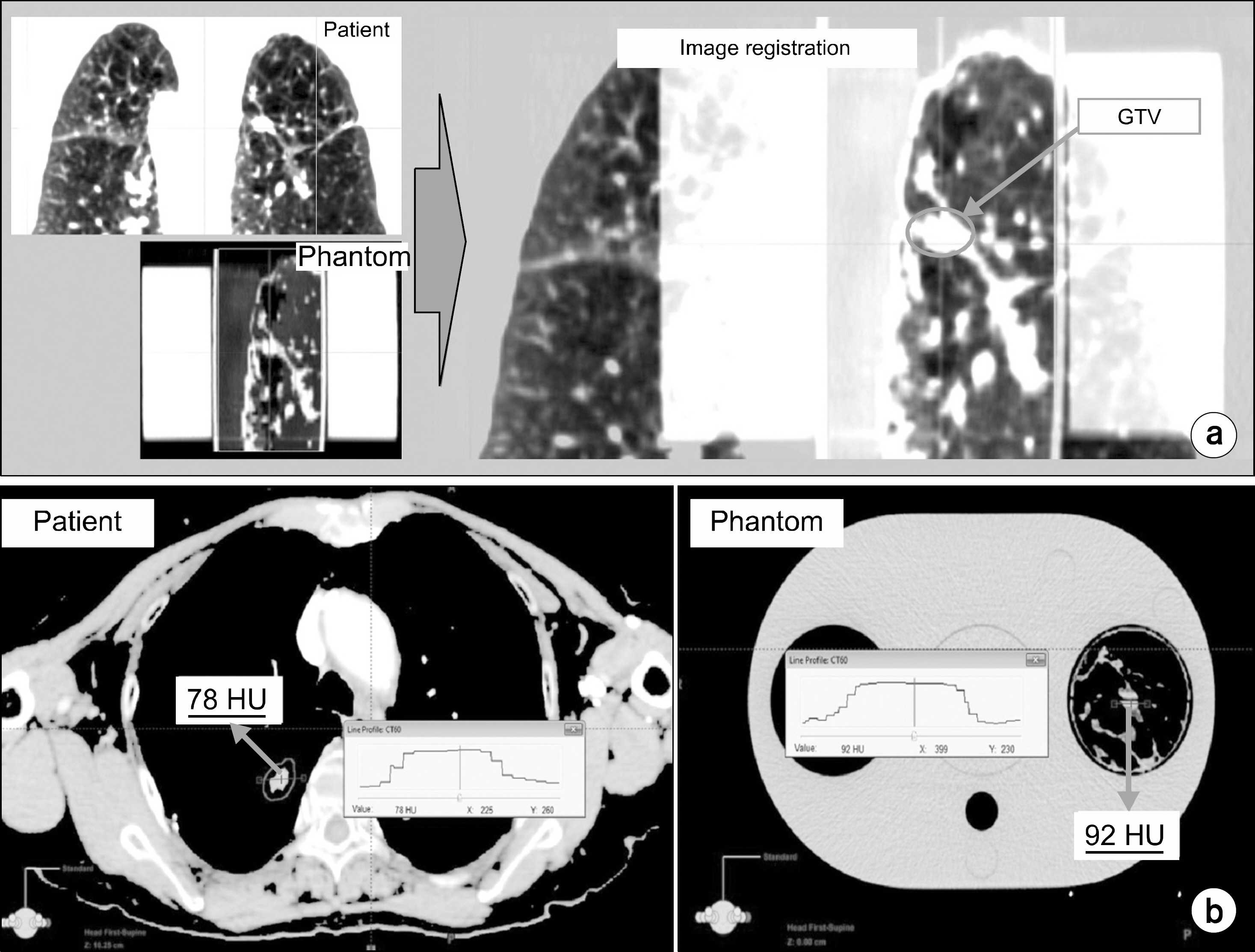
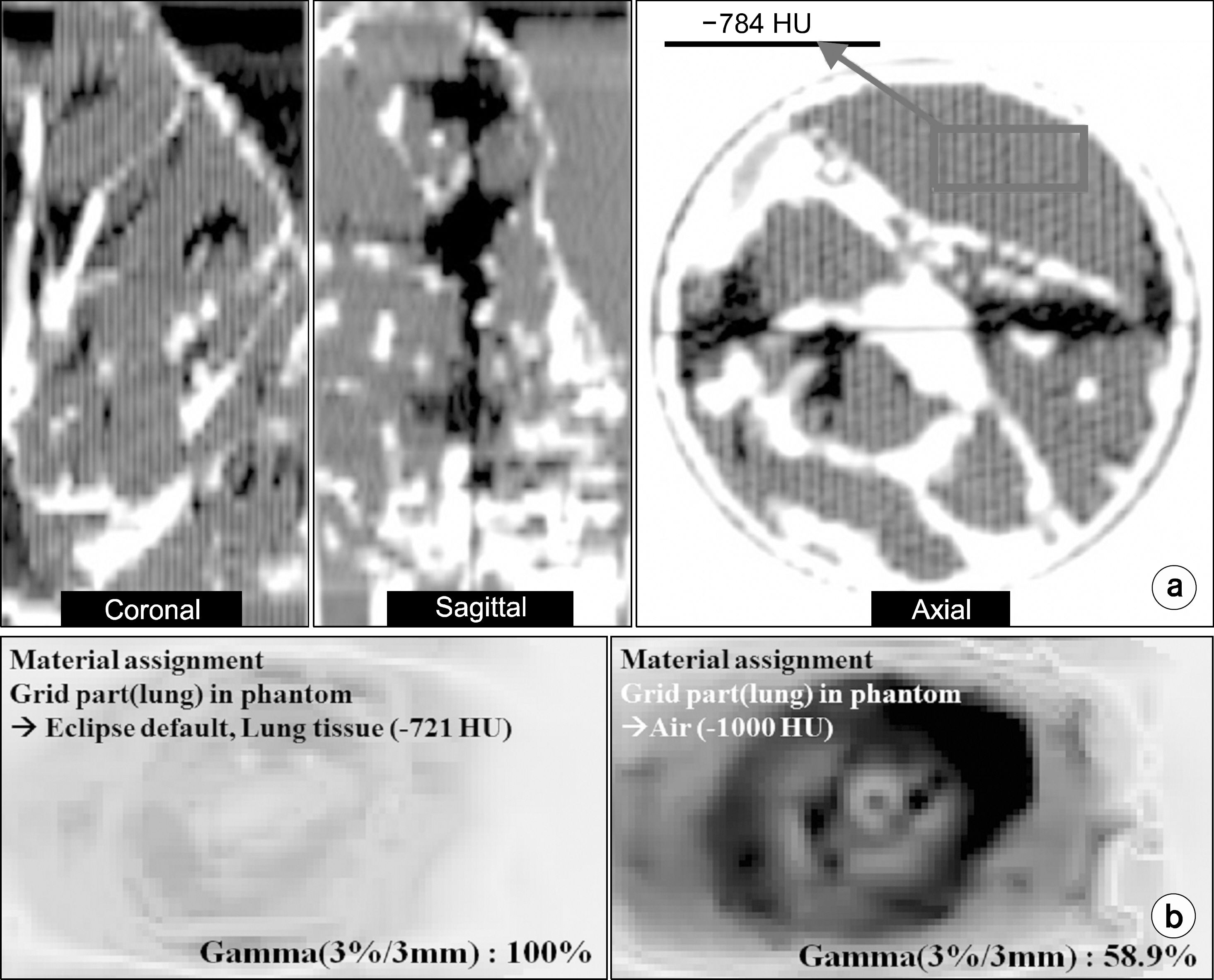
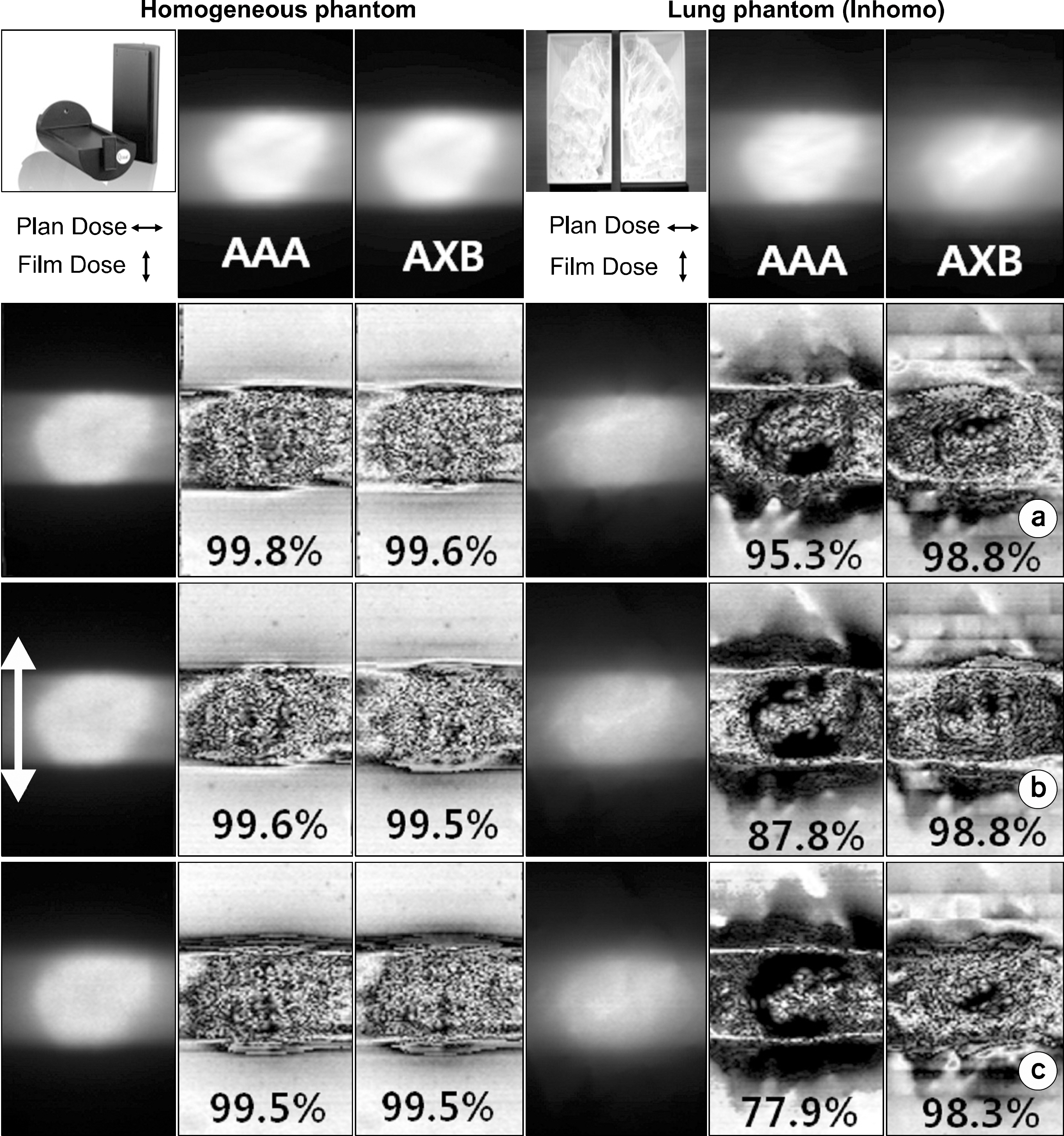
- In stereotactic body radiotherapy (SBRT), the accurate location of treatment sites should be guaranteed from the respiratory motions of patients. Lots of studies on this topic have been conducted. In this letter, a new verification method simulating the real respiratory motion of heterogenous treatment regions was proposed to investigate the accuracy of lung SBRT for Volumetric Modulated Arc Therapy. Based on the CT images of lung cancer patients, lung phantoms were fabricated to equip in QUASAR(TM) respiratory moving phantom using 3D printer. The phantom was bisected in order to measure 2D dose distributions by the insertion of EBT3 film. To ensure the dose calculation accuracy in heterogeneous condition, The homogeneous plastic phantom were also utilized. Two dose algorithms; Analytical Anisotropic Algorithm (AAA) and AcurosXB (AXB) were applied in plan dose calculation processes. In order to evaluate the accuracy of treatments under respiratory motion, we analyzed the gamma index between the plan dose and film dose measured under various moving conditions; static and moving target with or without gating. The CT number of GTV region was 78 HU for real patient and 92 HU for the homemade lung phantom. The gamma pass rates with 3%/3 mm criteria between the plan dose calculated by AAA algorithm and the film doses measured in heterogeneous lung phantom under gated and no gated beam delivery with respiratory motion were 88% and 78%. In static case, 95% of gamma pass rate was presented. In the all cases of homogeneous phantom, the gamma pass rates were more than 99%. Applied AcurosXB algorithm, for heterogeneous phantom, more than 98% and for homogeneous phantom, more than 99% of gamma pass rates were achieved. Since the respiratory amplitude was relatively small and the breath pattern had the longer exhale phase than inhale, the gamma pass rates in 3%/3 mm criteria didn't make any significant difference for various motion conditions. In this study, the new phantom model of 4D dose distribution verification using patient-specific lung phantoms moving in real breathing patterns was successfully implemented. It was also evaluated that the model provides the capability to verify dose distributions delivered in the more realistic condition and also the accuracy of dose calculation.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Clinical Implementation of 3D Printing in the Construction of Patient Specific Bolus for Photon Beam Radiotherapy for Mycosis Fungoides
Sung-woo Kim, Jungwon Kwak, Byungchul Cho, Si Yeol Song, Sang-wook Lee, Chiyoung Jeong
Prog Med Phys. 2017;28(1):33-38. doi: 10.14316/pmp.2017.28.1.33.Discrepancies between Calculated and Delivered Dose Distributions of Respiratory Gated IMRT Fields according to the Target Motion Ranges for Lung and Liver Cancer Patients
Youngkuk Kim, Sangwook Lim, Ji Hoon Choi, Sun Young Ma, Tae Sig Jeung, Tae Ik Ro
Prog Med Phys. 2014;25(4):242-247. doi: 10.14316/pmp.2014.25.4.242.
Reference
-
References
1. McNair HA, et al. Active Breathing Contr ol (ABC) in R adical Radiotherapy of Non-small Cell Lung Canc er (NS CLC). Clin Oncol (R Coll Radiol) 19: S 39 (. 2007.2. Ko YE, et al. Effectiveness of breath hold with a ABC for SRS of lung ca nc er. J Lung Ca nc er. 4:42–47. 2005.3. D'Souza WD, et al. The use of gated and 4D CT imaging in planning for ste reota ctic body radiation the rapy. Me d Dosim. 32:92–101. 2007.4. Wurm RE, et al. Image guided respiratory gated hypofractionated stereotactic body radiation therapy (H-SBRT) for liver and lung tumors: initial exper ience. Ac ta Onc ol. 45:881–889. 2006.5. Otto K, et al. Volumetric modula ted ar c the rapy: IM RT in a single gantry arc. Med P hys. 35(1):310–317. 2008.6. Ulmer W, et al. A 3D photon superposition/convolution algorithm and its foundation on r esul t s of Monte Ca rlo calculations. Phys Med Biol. 50(8):1767–1790. 2005.7. Gifford KA, et al. Comparison of a finite-element multigroup discrete-ordinates code with Monte Carlo for radiothera py ca l-culations. Phys Me d Biol. 51(9):2253. 2006.8. Vassiliev ON, et al. Validation of a new grid-based Boltzmann equation solver for dose calculation in radiothera py with photon b e a ms. Phys Me d Biol. 55(3):581–598. 2010.9. Keall P, et al. The management of respiratory motion in radiation oncology rep ort of AAPM Task Group 76. Med P hys. 33:3874–3900. 2006.10. Li XA, et al. Point/counterpoint. Respiratory gating for r ad i ation the rapy is not rea dy for prime time. Med Phys. 34:867–870. 2007.11. Andriy Fedorov, et al. 3D Slicer as an image computing platform for the Quantitative Imaging Network. Magnetic Resonance Ima ging. 30:1323–1341. 2012.12. A. Sam Beddar, et al: Correlation be twee n internal fiducial tumor motion and external ma rke r motion for liver tumors imaged with 4D-CT. International Journal of Ra diation Onc ology and Biology a nd P hysi c s. 67:630–638. 2008.13. Thomas SJ, et al. Relative electron density calibration of CT scanners for radiotherapy treatment planning. Br J Radiol. 72:781–786. 1999.
Article14. Kilby W, Sage J, Rabett V, et al. Tolerance levels for quality assura nce of electron de nsity values generated from CT in radiotherapy treatme nt pla nn i n g. Phys Med Biol. 47:1485–1492. 2002.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Strategy of Respiratory Gated Radiation Therapy for Lung Cancer Patient in Stereotactic Radiosurgery : Phantom Study
- Feasibility Study of Mobius3D for Patient-Specific Quality Assurance in the Volumetric Modulated Arc Therapy
- Dosimetric Evaluation of Amplitude-based Respiratory Gating for Delivery of Volumetric Modulated Arc Therapy
- Selection of Proper Modality in Stereotactic Body Radiation Therapy for Hepatocellular Carcinoma
- Comparison of the Dose Distributions with Beam Arrangements in the Stereotactic Body Radiotherapy (SBRT) for Primary Lung Cancer