J Korean Endocr Soc.
2007 Apr;22(2):135-141. 10.3803/jkes.2007.22.2.135.
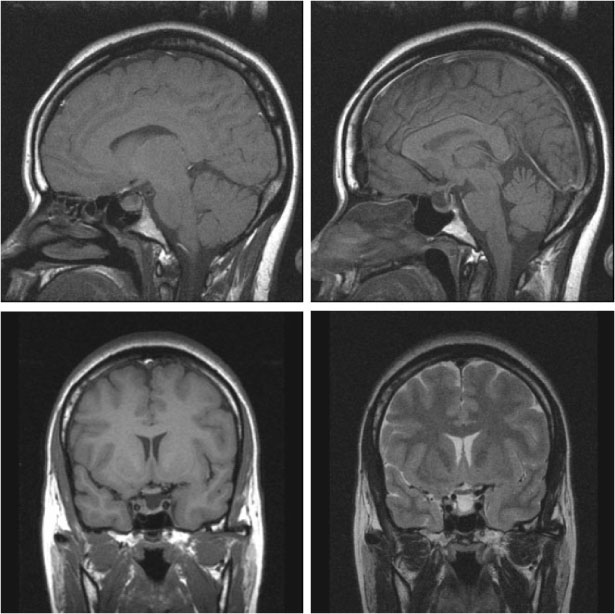
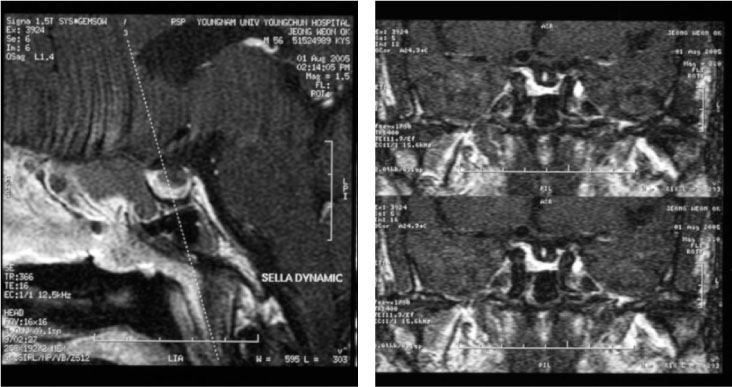
Two Cases of Acromegaly with Empty Sella Syndrome Treated by Long-Acting Release Octreotide
- Affiliations
-
- 1Department of Internal Medicine, Korea University College of Medicine, Korea.
- KMID: 1523095
- DOI: http://doi.org/10.3803/jkes.2007.22.2.135
Abstract
- Two cases of typical acromegaly with empty sella syndrome presented to our institution. In the natural course of untreated pituitary adenoma, empty sella syndrome may result from necrosis by infarction or from hemorrhage of the pituitary gland. In our patients, the secretion of growth hormone continued in spite of the existence of empty sella syndrome. In one case, we confirmed the hypersecretion of growth hormone from sella by jugular vein sampling. Medical therapy with somatostatin analogue was attempted because there was no obvious mass in the sella. After 6~12 months of treatment with long-acting release octreotide, clinical features in our patients were improved, and the level of growth hormone and IGF-1 were also normalized.
Keyword
MeSH Terms
Figure
Reference
-
1. Wright AD, Hill DM, Lowy C, Fraser TR. Mortality in acromegaly. Q J Med. 1970. 39:1–16.2. Lim EM, Pullan P. Biochemical assessment and long-term monitoring in patients with acromegaly: statement from a joint consensus conference of the Growth Hormone Research Society and the Pituitary Society. Clin Biochem Rev. 2005. 26:41–43.3. Login I, Santen RJ. Empty sella syndrome. Sequela of the spontaneous remission of acromegaly. Arch Intern Med. 1975. 135:1519–1521.4. Melmed S. Acromegaly. N Engl J Med. 1990. 322:966–977.5. Degli Uberti EC, Teodori V, Trasforini G, Tamarozzi R, Margutti A, Bianconi M, Rossi R, Ambrosio MR, Pansini R. The empty sella syndrome. Clinical, radiological and endocrinologic analysis in 20 cases. Minerva Endocrinol. 1989. 14:1–18.6. De Marinis L, Bonadonna S, Bianchi A, Maira G, Giustina A. Primary empty sella. J Clin Endocrinol Metab. 2005. 90:5471–5477.7. Gallardo E, Schachter D, Caceres E, Becker P, Colin E, Martinez C, Henriquez C. The empty sella: results of treatment in 76 successive cases and high frequency of endocrine and neurological disturbances. Clin Endocrinol (Oxf). 1992. 37:529–533.8. Jordan RM, Kendall JW, Kerber CW. The primary empty sella syndrome: analysis of the clinical characteristics, radiographic features, pituitary function and cerebrospinal fluid adenohypophysial hormone concentrations. Am J Med. 1977. 62:569–580.9. Molitch ME, Hieshima GB, Marcovitz S, Jackson IM, Wolpert S. Coexisting primary empty sella syndrome and acromegally. Clin Endocrinol (Oxf). 1977. 7:261–263.10. Bjerre P, Lindholm J, Videbaek H. The spontaneous course of pituitary adenomas and occurrence of an empty sella in untreated acromegaly. J Clin Endocrinol Metab. 1986. 63:287–291.11. Bjerre P, Gyldensted C, Riishede J, Lindholm J. The empty sella and pituitary adenomas. A theory on the causal relationship. Acta Neurol Scand. 1982. 66:82–92.12. Findling JW, Tyrrell JB, Aron DC, Fitzgerald PA, Wilson CB, Forsham PH. Silent pituitary apoplexy: subclinical infarction of an adrenocorticotropin-producing pituitary adenoma. J Clin Endocrinol Metab. 1981. 52:95–97.13. Wakai S, Fukushima T, Teramoto A, Sano K. Pituitary apoplexy: its incidence and clinical significance. J Neurosurg. 1981. 55:187–193.14. Yarman S, Minareci O. Value of petrosal sinus sampling: coexisting acromegaly, empty sella and meningioma. Neuroradiology. 2004. 46:1027–1030.15. Doppman JL, Miller DL, Patronas NJ, Oldfield EH, Merriam GR, Frank SJ, Flack MR, Weintraub BD, Gorden P. The diagnosis of acromegaly: value of inferior petrosal sinus sampling. AJR Am J Roentgenol. 1990. 154:1075–1077.16. Merola B, Colao A, Rossi E, La Tessa G, Spaziante R, Lombardi G. Hormonal gradients between inferior petrosal sinuses in various pituitary diseases. Acta Endocrinol (Copenh). 1992. 126:419–424.17. Sturrock ND, Jeffcoate WJ. A neurological complication of inferior petrosal sinus sampling during investigation for Cushing's disease: a case report. J Neurol Neurosurg Psychiatry. 1997. 62:527–528.18. Miller DL, Doppman JL, Peterman SB, Nieman LK, Oldfield EH, Chang R. Neurologic complications of petrosal sinus sampling. Radiology. 1992. 185:143–147.19. Obuobie K, Davies JS, Ogunko A, Scanlon MF. Venous thrombo-embolism following inferior petrosal sinus sampling in Cushing\'s disease. J Endocrinol Invest. 2000. 23:542–544.20. Ilias I, Chang R, Pacak K, Oldfield EH, Wesley R, Doppman J, Nieman LK. Jugular venous sampling: an alternative to petrosal sinus sampling for the diagnostic evaluation of adrenocorticotropic hormone-dependent Cushing's syndrome. J Clin Endocrinol Metab. 2004. 89:3795–3800.21. Bates AS, Van't Hoff W, Jones JM, Clayton RN. An audit of outcome of treatment in acromegaly. Q J Med. 1993. 86:293–299.22. Melmed S, Casanueva FF, Cavagnini F, Chanson P, Frohman L, Grossman A, Ho K, Kleinberg D, Lamberts S, Laws E, Lombardi G, Vance ML, Werder KV, Wass J, Giustina A. Guidelines for acromegaly management. J Clin Endocrinol Metab. 2002. 87:4054–4058.23. Cozzi R, Montini M, Attanasio R, Albizzi M, Lasio G, Lodrini S, Doneda P, Cortesi L, Pagani G. Primary treatment of acromegaly with octreotide LAR: a long-term (up to nine years) prospective study of its efficacy in the control of disease activity and tumor shrinkage. J Clin Endocrinol Metab. 2006. 91:1397–1403.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of acromegaly with empty sella syndrome associated with colonic neoplasm
- Two Cases of Graves Disease Associated The Empty Sella Syndrome
- Two Cases of Acromegaly with Empty Sella
- A case of primary empty sella syndrome combined with Cushing's disease
- A Case of Empty Sella Syndrome with Cerebrospinal Fluid Rhinorrhea