J Korean Diabetes Assoc.
2007 May;31(3):261-273. 10.4093/jkda.2007.31.3.261.
Activation of NF-kappaB and AP-1 in Peripheral Blood Mononuclear Cells Isolated from Patients with Diabetic Nephropathy
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University College of Medicine, Korea.
- 2Department of Internal Medicine, Ewha Womans University, Pharmacy, Korea.
- KMID: 1523015
- DOI: http://doi.org/10.4093/jkda.2007.31.3.261
Abstract
-
BACKGROUND: We evaluated the role of oxidative stress in diabetic nephropathy by measuring intracellular reactive oxygen species (ROS) and redox-sensitive transcription factors in isolated peripheral mononuclear cells (PBMC).
METHODS
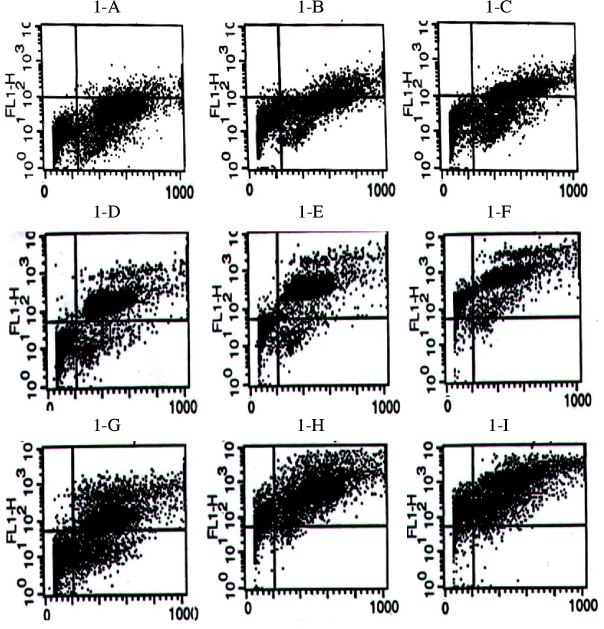
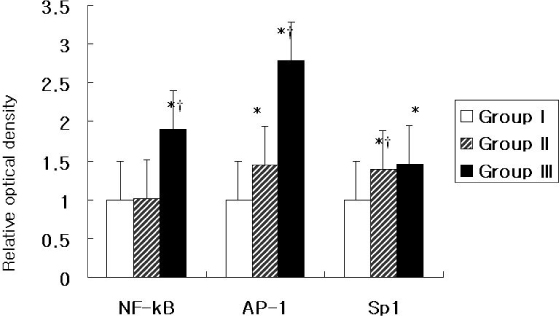
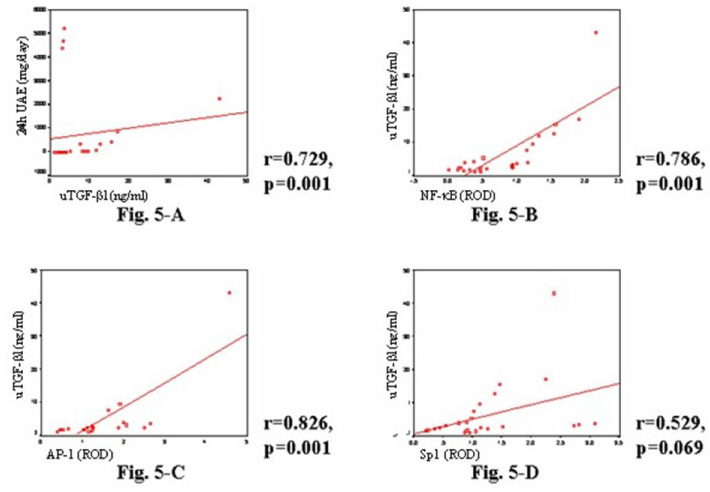
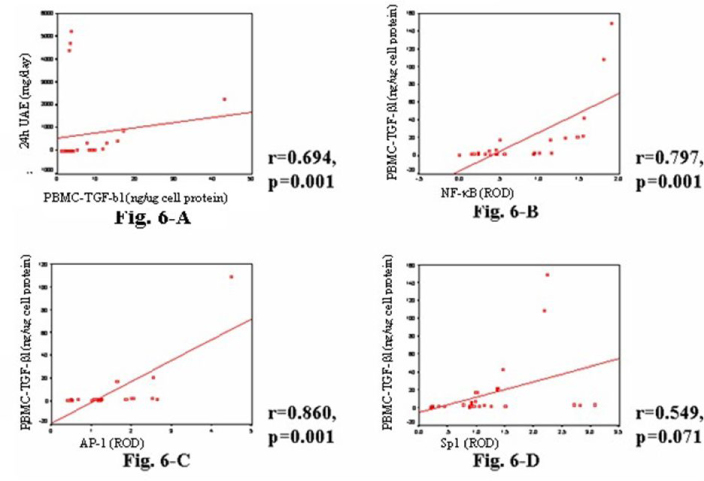
From 66 diabetic patients with or without diabetic nephropathy (Group III and II, respectively) and 49 normal control subjects (Group I), spontaneous and stimulated ROS levels, activities of nuclear factor-kappa B (NF-kappaB), activator protein-1 (AP-1), and specificity protein1 (Sp1) in PBMC, urinary and PBMC TGF-beta1 (transforming growth factor-beta1), and 24-hour urinary albumin excretion (UAE) were measured.
RESULTS
Spontaneous ROS was significantly higher in group III and II than group I (60.7 +/- 3.3 vs. 60.0 +/- 3.0 vs. 41.1 +/- 2.4%, respectively), and stimulated ROS were significantly higher in Group III compared to Group II (Increment of H2O2-induced ROS production: 21.8 +/- 2.2 vs. 11.1 +/- 2.0%, respectively; increment of PMA-induced ROS production 23.5 +/- 4.5 vs. 21.6 +/- 2.2%, respectively). The activities of NF-kappaB and AP-1, but not of Sp1, were significantly higher in Group III than in Group II (2.53 vs. 2.0 vs. 1.43-fold, respectively). Both PBMC- and urinary TGF-beta1 levels were higher in Group III than Group II (3.23 +/- 0.39 vs. 1.99 +/- 0.68 ng/mg in PBMCs, 16.88 +/- 6.84 vs. 5.61 +/- 1.57 ng/mL in urine, both respectively), and they were significantly correlated with activities of NF-kappaB and AP-1 and 24-hour UAE.
CONCLUSIONS
Increased intracellular ROS generation in PBMCs of diabetic patients is involved in the pathogenesis of diabetic nephropathy through activation of NF-kappaB and AP-1, but not Sp1, and increased expression of TGF-beta1.
Keyword
MeSH Terms
Figure
Reference
-
1. The Diabetes Control and Complication Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin dependent diabetes mellitus. N Eng J Med. 1993. 329:977–986.2. United Kingdom Prospective Diabetes Study 33. Intensive blood glucose control with sulphonylurea and insulin compared with conventional treatment and the risk of complication in the patients with type 2 diabetes. Lancet. 1998. 352:837–853.3. Baynes JW. Role of oxidative stress in development of complications in diabetes. Diabetes. 1991. 40:405–412.4. Nourooz-Zadeh J, Rahimi A, Tajaddini-Sarmadi J, Tritschler H, Rosen P, Halliwell B, Betteridge DJ. Relationship between plasmameasures of oxidative stress and metabolic control in non-insulin-dependent diabetes mellitus. Diabetologia. 1997. 40:647–654.5. Godin DV, Wohaieb SA, Garnett ME, Goumeniouk AD. Antioxidant enzyme alterations in experimental and clinical diabetes. Mol Cell Biochem. 1988. 84:223–231.6. Giugliano D, Ceriello A, Paolisso G. Diabetes mellitus, hypertension, and cardiovascular disease: which role for oxidative stress? Metabolism. 1995. 44:363–368.7. Rema M, Mohan V, Bhaskar A, Shanmugasundaram KR. Does oxidant stress play a role in diabetic retinopathy? Indian J Opthalmol. 1995. 43:17–21.8. Ha H, Kim KH. Role of oxidative stress in the development of diabetic nephropathy. Kidney Int. 1995. 51:S18–S21.9. Baynes JW. Role of oxidative stress in development of complication of diabetes. Diabetes. 1991. 40:405–412.10. Lee HB, Yu MR, Yang Y, Jiang Z, Ha H. Reactive oxygen species-regulated signaling pathways in diabetic nephropathy. J Am Soc Nephrol. 2003. 14:S241–S245.11. Chung FM, Shin SJ, Tsai JC, Lee YJ, Chang DM. Peripheral total and differential leukocyte count in diabetic nephropathy. Diabetes care. 2005. 28:1710–1717.12. Galkina E, Ley K. Leukocyte recruitment and vascular injury in diabetic nephropathy. J Am Soc Nephrol. 2006. 17:368–377.13. Sassy-Prigent C, Heudes D, Mandet C, Belair MF, Michel O, Perdereau B, Bariety J, Bruneval P. Early glomerular macrophage recruitement in streptozocin-induced diabetic rats. Diabetes. 2000. 49:466–475.14. Takahashi T, Hato F, Yamane T, Inaba M, Okuno Y, Nishizawa Y, Kitagawa S. Increased spontaneous adherence of neutrophils from type 2 diabetic patients with overt proteinuria: Possible role of the progression of diabetic nephropathy. Diabetes Care. 2000. 23:417–418.15. Dhindsa S, Tripathy D, Mohanty P, Ghanim H, Syed T, Aljada A, Dandona P. Differential effects of glucose and alcohol on reactive oxygen speciesgeneration and intranuclear nuclear factor-kappaB in mononuclear cells. Metab Clin Exp. 2004. 53:330–334.16. Du X, Stockklauser-Farber K, Ames NB. Generation of reactive oxygen intermediates, activation of NF-B, and induction of apoptosis in human endothelial cells by glucose: Role of nitric oxide synthase? Free Rad Biol Med. 1999. 27:752–763.17. Baeuerle PA, Baltimore D. NF-κB. ten years after. Cell. 1996. 87:13–20.18. Pinkus R, Weiner R, Daniel V. Role of oxidnats and antioxidants in the induction of AP-1, NF-B, and gluthatione S-transferase gene expression. J Biol Chem. 1996. 271:13422–13429.19. Kim SJ, Angel P, Lavatis R, Hattori K, Kim YK, Sporn MB, Karin M, Roberts AB. Autoinduction of transforming growth factor-β1 is mediated by the AP-1 complex. Mol Cell Biol. 1990. 10:1492–1497.20. Ueda A, Okuda K, Ohno S, Shirai A, Igarashi T, Matsunage K, Fukushima J, Kawamoto S, Ishigatsubo Y, Okubo T. NF-κB and Sp1 regulates transcription of the human monocyte chemoattractant protein-1 gene. J Immunol. 1994. 153:2052–2063.21. Baeuerle PA. The inducible transcription factor NF-κB: regulation by distinct protein subunits. Biochim Biophys Acta. 1991. 1072:63–80.22. Baeuerle PA, Baltimore D. I-κB: a specific inhibitor of the NF-κB transcription factor. Science. 1988. 242:540–546.23. Lenardo MJ, Baltimore D. NF-κB: a pleiotropic mediator of inducible and tissue-specific gene control. Cell. 1989. 58:227–229.24. Liao F, Andalibi A, DeBeer FC, Fogelman AM, Lusis AJ. Genetic control of inflammatory gene induction and NF-κB-like transcription factor activation in response to an atherogenic diet in mice. J Clin Invest. 1993. 91:2572–2579.25. Baeuerle PA, Henkel T. Function and activation of NF-κB in immune system. Ann Rev Immunol. 1994. 12:141–179.26. Robbesyn F, Salvayre R, Negre-Salvayre A. Dual role of oxidized LDL on the NF-kappa B signaling pathway. Free Radic Res. 2004. 38:541–551.27. Hofmann MA, Schiekofer S, Isermann B, Kanitz M, Henkels M, Joswig M, Treusch A, Morcos M, Weiss T, Borcea V, Abdel Khalek AK, Amiral J, Tritschler H, Ritz E, Wahl P, Ziegler R, Bierhaus A, Nawroth PP. Peripheral blood mononuclear cells isolated from patients with diabetic nephropathy show increased activation of the oxidative-stress sensitive transcription factor NF-κB. Diabetologia. 1999. 42(2):222–232.28. Hofmann MA, Schiekofer S, Kanitz MS, Joswig M, Lee V, Morcos M, Tritschler H, Ziegler R, Wahl P, Bierhaus A, Nawroth PP. Insufficient glycaemic control increases NF-κB binding activity in peripheral blood mononuclear cells isolated from patients with type 1 diabetes. Diabetes Care. 1998. 21:1–7.29. Ziyadeh FN, Sharma K, Ericksen M, Wolf G. Stimulation of collagen gene expression and protein synthesis in murine mesangial cells by high glucose is mediated by activation of transforming growth factor-β. J Clin Invest. 1994. 93:536–542.30. Miyazono K, Olofsson A, Colosetti P, Heldin CH. A role of the latent TGF-β1-binding protein in the assembly and secretion of TGF-β1. EMBO J. 1991. 10:1091–1101.31. Franza BR, Rauscher FJ, Josephs SF, Curran T. The fos complex and fos-related antigens recognize elements that contain AP-1 binding sites. Science. 1988. 239:1150–1153.32. Stein B, Baldwin AS, Ballard DW, Greene WC, Angel P, Herrlich P. Cross-coupling of the NF-κB p65 and Fos/Jun transcription factor produces potentiated biological function. EMBO J. 1993. 12:3879–3891.33. Sen CK, Packer L. Antioxidant and redox regulation of gene transcription. FASEB J. 1996. 10:709–720.34. Du XL, Edelstein D, Rossetti L, Fantus IG, Goldberg H, Ziyadeh F, Wu J, Brownlee M. Hyperglycemia-Induced Mitochondrial Superoxide Overproduction Activates the Hexosamine Pathway and Induces PAI-1 and TGF-β Expression by Increasing Sp1 Glycosylation. Proc Natl Acad Sci U S A. 2000. 97:12222–12226.35. Goldberg HJ, Scholey J, Fantus IG. Glucosamine activates the plasminogen activator inhibitor 1 gene promoter through Sp1 DNA binding sites in glomerular mesangial cells. Diabetes. 2000. 49:863–871.36. Mller GA, Schettler V, Mller CA, Strutz F. Prevention of progression of renal fibrosis: How far are we? Kidney International. 1996. 49:Suppl54. S75–S82.37. Wolf G, Sharma K, Chen Y, Ericksen M, Ziyadeh FN. High glucose-induced proliferation in mesangial cells is reversed by autocrine TGF-β. Kidney Int. 1992. 42:647–656.38. Rocco M, Chen Y, Goldfarb S, Ziyadeh FN. Elevated glucose stimulates TGF-β gene expression and bioactivity in proximal tubule. Kidney Int. 1992. 41:107–114.39. Diep QN, Benkirane K, Amiri F, Cohn JS, Endemann D, Schiffrin EL. PPAR alpha activator fenofibrate inhibits myocardial inflammation and fibrosis in angiotensin II-infused rats. J Mol Cell Cardiol. 2004. 36:295–304.40. Rothbarth HP, Hendriks-Sturkenboom I, Ploem J. Identification of monocytes in suspension of mononuclear cells. Blood. 1976. 48:139–147.41. Holschermann H, Durfeld F, Maus U, Bierhaus A, Heidinger K, Lohmeyer J, Nawroth PP, Tillmanns H, Haberbosch W. Cyclosporine a inhibits tissue factor expression in monocytes/macrophages. Blood. 1996. 88:3837–3845.42. Bradford MM. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem. 1976. 72:248–254.43. Bierhaus A, Zhang Y, Quehenberger P, Luther T, Haase M, Muller M, Mackman N, Ziegler R, Nawroth PP. The dietary pigmentcurcumin reduces endothelial tissue factor gene expression by inhibiting binding of AP-1 to the DNA and activation of NF-κB. Thromb Haemost. 1997. 77:772–782.44. Niwa Y, Ozaki Y, Kanoh T, Akamatsu H, Kurisaka M. Role of cytokines, tyrosine kinase and protein kinase C on production of superoxide and induction ofscavenging enzymes in human leukocytes. Clin Immunopathol. 1996. 79:303–313.45. Koya D, King GL. Protein kinase C activation and the development of diabetic complications. Diabetes. 1998. 47:859–866.46. Ha H, Lee HB. Reactive oxygen species as glucose signaling molecules in mesangial cells cultured under high glucose. Kidney Int. 2000. 77:S19–S25.47. Ha H, Lee HB. Reactive oxygen species amplify glucose signaling in renal cells cultured under high glucose and in diabetic kidney. Nephrology. 2005. 10:S7–S10.48. Iwasaki Y, Kambayashi M, Asai M, Yoshida M, Nigawara T, Hashimoto K. High glucose alone, as well as in combination with proinflammatory cytoines, stimulates nuclear factor kappa-B-mediated transcription in hepatocytesin vitro. J Diabetes Complicat. 2007. 21:56–62.49. Weigert C, Sauer U, Brodbeck K, Pfeiffer A, Haring HU, Schleicher ED. AP-1 proteins mediate hyperglycemia-induced activation of the human TGF-β1 promoter in mesangial cells. J Am Soc Nephrol. 2000. 11:2007–2016.50. Hill C, Flyvbjerg A, Grnbk H, Petrik J, Hill DJ, Thomas CR, Sheppard MC, Logan A. The Renal Expression of Transforming Growth Factor-Isoforms and Their Receptors in Acute and Chronic Experimental Diabetes in Rats. Endocrinology. 2000. 141(3):196–208.51. Weier Q, Chen X, Holian J, Mreich E, Twigg S, Gilbert RE, Pollock CA. Transforming growth factor-β1 differentially mediates fibronectin and inflammatory cytokine expression in kidney tubular cells. Am J Physiol. 2006. 291:F1070–F1077.52. Chuang LY, Guh JY. Extracellular signals and intracellular pathways in diabetic nephropathy. Nephrology. 2001. 6:154–172.53. Han DC, Ziyadeh FN. Favorable treatment outcome with neutralizing anti-transforming growth factor-β antibodies in experimental diabetic kidney disease. Perit Dial Int. 1999. 19:S234–S237.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- NF-kappaB Activation in T Helper 17 Cell Differentiation
- beta-Lapachone suppresses radiation-induced activation of nuclear factor-kappaB
- Activation of Transcription Factor NF-kappaB and c-Jun/AP-1 by Various Compositions of Particles in Osteoclast Precursor Cells
- Regulation of B cell activating factor (BAFF) receptor expression by NF-kappaB signaling in rheumatoid arthritis B cells
- Hyperglycemia-induced Activation of Nuclear Transcription Factor kappaB in Cultured Fibroblasts and Endothelial Cells