Korean J Gastroenterol.
2013 Mar;61(3):155-159. 10.4166/kjg.2013.61.3.155.
A Case of Double Primary Neuroendocrine Tumor from Duodenum and Pancreas
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. hjpark21@yuhs.ac
- 2Department of Pathology, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Surgery, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 1501638
- DOI: http://doi.org/10.4166/kjg.2013.61.3.155
Abstract
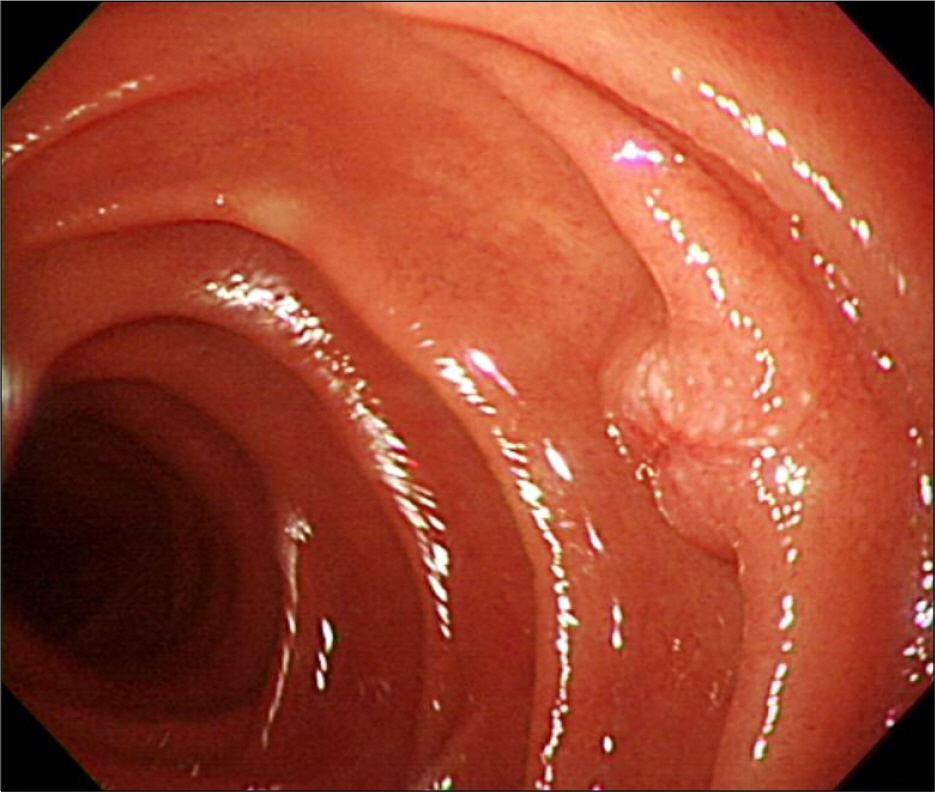
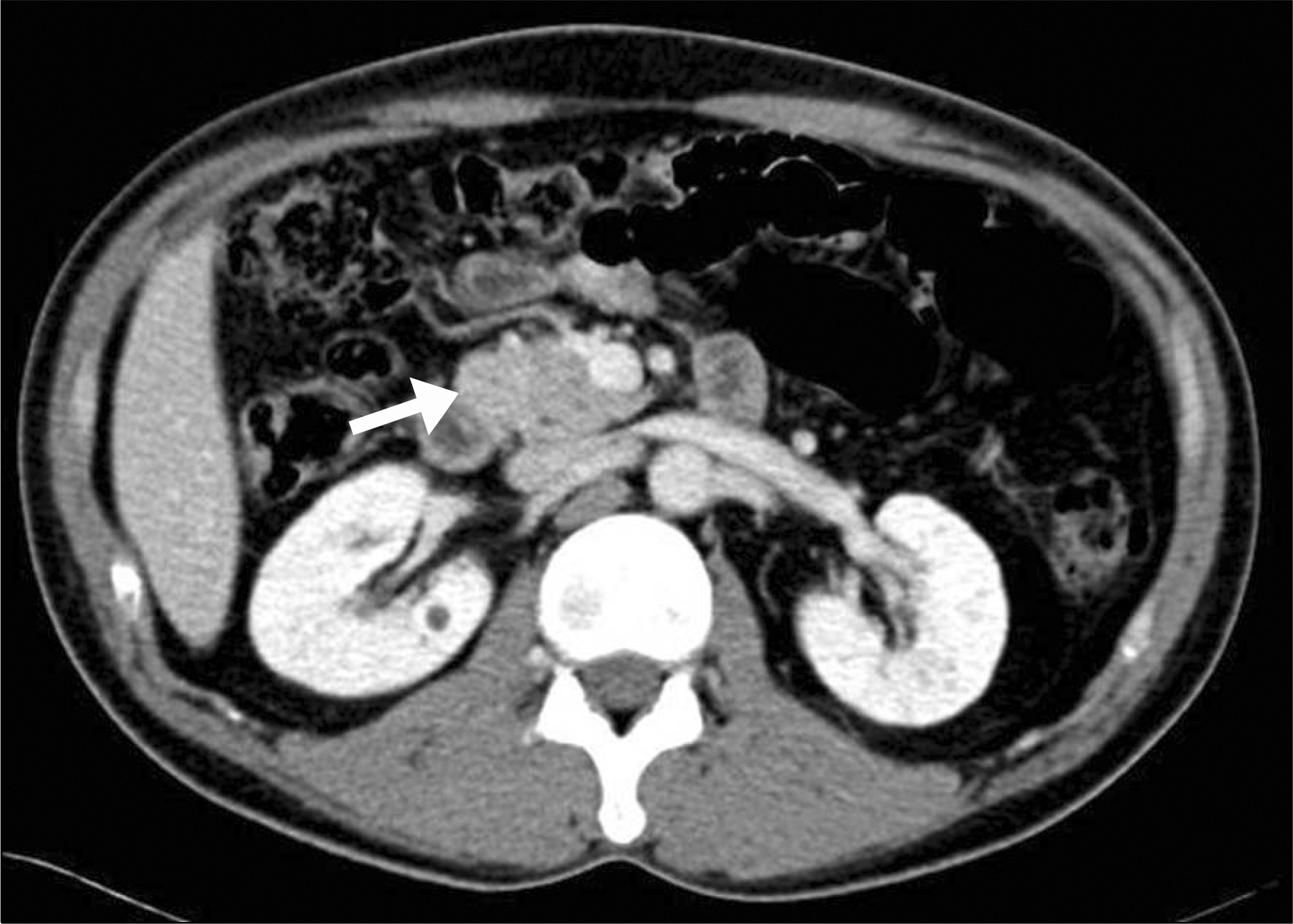
- Gastrointestinal neuroendocrine tumors arise from cells of the diffuse neuroendocrine system and can take place almost anywhere within the gastrointestinal tract. A 40-year-old man admitted to evaluate a duodenal subepithelial lesion which was incidentally found at health check-up. The polypoid duodenal subepithelial lesion, measuring about 7 mm, was removed by the endoscopic mucosal resection and the pathology confirmed a neuroendocrine tumor. Abdominopelvic computed tomography, done for staging work up, revealed a mass in the pancreatic head and the patient received pylorus preserving pancreaticoduodenectomy. Mass at the pancreas also found out to be neuroendocrine tumor but showed different histopathologic traits under immunohistochemical staining. The patient was also diagnosed as hyperparathyroidism and pituitary microadenoma. Finally, multiple endocrine neoplasia type 1 was confirmed, which was accompanied by duodenal neuroendocrine tumor.
MeSH Terms
-
Adult
Antigens, CD56/metabolism
Duodenum/*pathology
Endoscopy, Digestive System
Humans
Immunohistochemistry
Magnetic Resonance Imaging
Male
Neoplasms, Multiple Primary
Neuroendocrine Tumors/*diagnosis/metabolism/surgery
Pancreas/*pathology
Synaptophysin/metabolism
Tomography, X-Ray Computed
Antigens, CD56
Synaptophysin
Figure
Reference
-
References
1. Chang JH, Kim SW, Chung WC, et al. Clinical review of gastrointestinal carcinoid tumor and analysis of the factors predicting metastasis. Korean J Gastroenterol. 2007; 50:19–25.2. Sun JM, Jung HC. Gastrointestinal carcinoid tumor. Korean J Gastroenterol. 2004; 44:59–65.3. Falconi M, Plockinger U, Kwekkeboom DJ, et al. Frascati Consensus Conference; European Neuroendocrine Tumor Society. Well-differentiated pancreatic nonfunctioning tumors/carcinoma. Neuroendocrinology. 2006; 84:196–211.
Article4. Yao JC, Eisner MP, Leary C, et al. Population-based study of islet cell carcinoma. Ann Surg Oncol. 2007; 14:3492–3500.
Article5. Metz DC, Jensen RT. Gastrointestinal neuroendocrine tumors: pancreatic endocrine tumors. Gastroenterology. 2008; 135:1469–1492.
Article6. Yoon JH, Lee OY, Cho SC, et al. A case of small duodenal carcinoid tumor with liver metastasis. Korean J Gastroenterol. 2009; 53:246–250.7. Yazawa K, Kuroda T, Watanabe H, et al. Multiple carcinoids of the duodenum accompanied by type I familial multiple endocrine neoplasia. Surg Today. 1998; 28:636–639.
Article8. Basu B, Sirohi B, Corrie P. Systemic therapy for neuroendocrine tumours of gastroenteropancreatic origin. Endocr Relat Cancer. 2010; 17:R75–R90.
Article9. Campana D, Brocchi E, Tomassetti P. Multiple gastric endocrine tumours and gastrinomas of the duodenum in a patient with ZES MEN 1. Dig Liver Dis. 2008; 40:476.
Article10. Kageyama K, Sakihara S, Yamashita M, et al. A case of multiple endocrine neoplasia type II accompanied by thyroid medullary carcinoma and pheochromocytomas expressing corticotropinreleasing factor and urocortins. Am J Med Sci. 2008; 335:398–402.
Article11. Sugihara H, Shibasaki T, Tatsuguchi A, et al. A non-acromegalic case of multiple endocrine neoplasia type 1 accompanied by a growth hormone-releasing hormone-producing pancreatic tumor. J Endocrinol Invest. 2007; 30:421–427.
Article12. Sugimoto K, Oosawa S, Furuta T, et al. Multiple endocrine neoplasia type 1 accompanied by duodenal carcinoid tumors and hypergastrinemia: a familial case. Intern Med. 1995; 34:649–653.
Article13. Obara T, Fujimoto Y, Oka A, et al. Medullary thyroid carcinoma and pheochromocytoma accompanied with nodular hyperplasia in multiple endocrine neoplasia type 2. Jpn J Surg. 1977; 7:235–245.
Article14. Kim SY, Jung SW, Lee SW. A case of easily overlooked small duodenal carcinoid tumor. Korean J Gastroenterol. 2009; 54:265–267.
Article15. Paik WH, Yoon YB, Lee SH, et al. Pancreatic endocrine tumors: clinical manifestations and predictive factors associated with survival. Korean J Gastroenterol. 2008; 52:171–178.16. Han JH, Kim MH, Moon SH, et al. Clinical characteristics and malignant predictive factors of pancreatic neuroendocrine tumors. Korean J Gastroenterol. 2009; 53:98–105.17. Thakker RV, Newey PJ, Walls GV, et al. Endocrine Society. Clinical practice guidelines for multiple endocrine neoplasia type 1 (MEN1). J Clin Endocrinol Metab. 2012; 97:2990–3011.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Duodenal Neuroendocrine Tumor: a Diagnostic Surprise during Workup for Anemia
- Nonfunctioning Neuroendocrine Tumor of the Pancreas in a 15-year-old Girl: a Case Report
- Endoscopic Treatment for Early Foregut Neuroendocrine Tumors
- Synchronous Double Primary Cancer of the Stomach and Duodenum
- Islet Cell Tumor Arising from Heterotopic Pancreas in the Duodenum: A Case Report