Endocrinol Metab.
2012 Jun;27(2):142-146. 10.3803/EnM.2012.27.2.142.
A Case of Graves' Disease Presented as Generalized Seizure Attack
- Affiliations
-
- 1Department of Internal Medicine, Dong-A University College of Medicine, Busan, Korea. pmk02@dau.ac.kr
- 2Department of Neurology, Dong-A University College of Medicine, Busan, Korea.
- KMID: 1497654
- DOI: http://doi.org/10.3803/EnM.2012.27.2.142
Abstract
- Hyperthyroidism is diagnosed when a patient is presented with typical symptoms, such as weight loss, palpitation, and hand tremor. However, early diagnosis is difficult in elders, because they have no typical symptoms, but only cardiovascular or muscular symptoms. In hyperthyroidism, there are often with neurologic changes, leading to various neurologic symptoms. Generalized or focal seizures are rarely reported in thyrotoxicosis and thyrotoxic crisis. Further, cases of hyperthyroidism presented as generalized seizure attack are extremely rare. We report a case of hyperthyroidism. A patient is presented at the hospital with mental change, as well as generalized seizure, who was finally diagnosed to have Graves' disease. A 56-year-old male was admitted to the hospital because of mental change with generalized seizure attack. Initial neurologic evaluations, including a brain magnetic resonance imaging and electroencephalogram proved to be normal. But, thyroid function test showed abnormal results. We diagnosed him as Graves' disease and prescribed anti-thyroid drug. Thereafter, there has been no recurrence of neurologic symptoms for 12 months.
Keyword
MeSH Terms
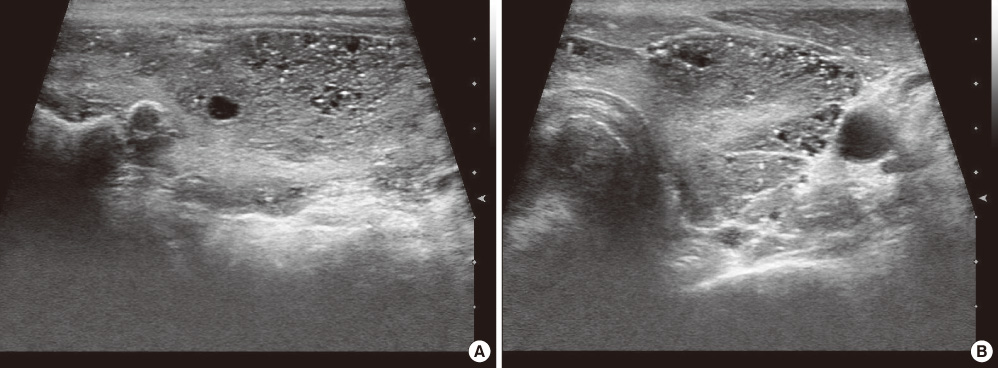
Figure
Reference
-
1. Cho BY. Clinical thyroidology. 2010. 3rd ed. Seoul: Korea Medical Book Publisher;307–309.2. Jameson JL, Anthony PW. Anthony SF, Dennis LK, Dan LL, Eugene B, Stephen LH, Jameson JL, Joseph L, editors. Disorders of thyroid grand. Harrison's Principles of Internal Medicine. 2008. 17th ed. McGraw-Hill;2234–2235.3. Skanse B, Nyman GE. Thyrotoxicosis as a cause of cerebral dysrhythmia and convulsive seizures. Acta Endocrinol (Copenh). 1956. 22:246–263.4. Lin CS, Yiin KT, Lin WH, Huang SY. Thyrotoxicosis accompanied with periodic seizure attacks a case report and review of literature. Zhonghua Yi Xue Za Zhi (Taipei). 1992. 50:335–337.5. Vergely N, Garnier P, Guy C, Khalfallah Y, Estour B. Seizure during Graves' disease. Epileptic Disord. 2009. 11:136–137.6. Yang JW, Lee JG, Oh SH, Lee HJ, Kim WJ. A case of seizure induced by levothyroxine intoxication in euthyroidism. J Korean Neurol Assoc. 2001. 19:550–552.7. Choi SH, Kang SH, Kim CY. Seizure and thyroid dysfunction associated with high dose of quetiapine: case report. J Korean Neuropsychiatr Assoc. 2006. 45:481–483.8. Boyages SC. Werner SC, Ingbar SH, Braverman LE, Utiger RD, editors. The neuromuscular system and brain in thyrotoxicosis. Werner and Ingbar's the Thyroid: A Fundamental and Clinical Text. 2005. 9th ed. Lippincott Williams & Wilkins;637–643.9. Beaumont A, Vespa P. Varelas PN, editor. Seizures in fulminant hepatic failure, multiorgan failure, and endocrine crisis. Seizures in Critical Care: A Guide to Diagnosis and Therapeutics. 2010. 2nd ed. New York: Humana Press;179–202.10. Jabbari B, Huott AD. Seizures in thyrotoxicosis. Epilepsia. 1980. 21:91–96.11. Smith DL, Looney TJ. Seizures secondary to thyrotoxicosis and high-dosage propranolol therapy. Arch Neurol. 1983. 40:457–458.12. Song TJ, Kim SJ, Kim GS, Choi YC, Kim WJ. The prevalence of thyrotoxicosis-related seizures. Thyroid. 2010. 20:955–958.13. Maeda T, Izumi T. Generalized convulsions with diffuse spike and wave bursts emerging with Graves' disease. Neuropediatrics. 2006. 37:305–307.14. Siegert CE, Smelt AH, de Bruin TW. Superior sagittal sinus thrombosis and thyrotoxicosis. Possible association in two cases. Stroke. 1995. 26:496–497.15. Sinn DI, Kwon SJ, Hong YH, Lee KW. A case of cerebral venous thrombosis associated with increased factor VIII in hyperthyroidism. J Korean Neurol Assoc. 2006. 24:472–474.16. Wan RQ, Noguera EC, Weiss SR. Anticonvulsant effects of intra-hippocampal injection of TRH in amygdala kindled rats. Neuroreport. 1998. 9:677–682.17. Pekary AE, Sattin A. Regulation of TRH and TRH-related peptides in rat brain by thyroid and steroid hormones. Peptides. 2001. 22:1161–1173.18. Deng PY, Porter JE, Shin HS, Lei S. Thyrotropin-releasing hormone increases GABA release in rat hippocampus. J Physiol. 2006. 577(Pt 2):497–511.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Surgical Effect of Callosotomy in the Treatment of Intractable Seizure
- Two Cases of Graves' Disease Presented with Atypical Symptoms
- Callosotomy for Intractable Epilepsy in Children
- A Case of Idiopathic Hypoparathyroidism Associated with Graves' Disease
- Generalized Tonic-Clonic Seizure following Myelography with Iohexol (Omnipaque.): A Case Report