J Korean Endocr Soc.
2009 Dec;24(4):281-286. 10.3803/jkes.2009.24.4.281.
A Case of Insulin Autoimmune Syndrome in a Patient with Partial Hypopituitarism
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 1468549
- DOI: http://doi.org/10.3803/jkes.2009.24.4.281
Abstract
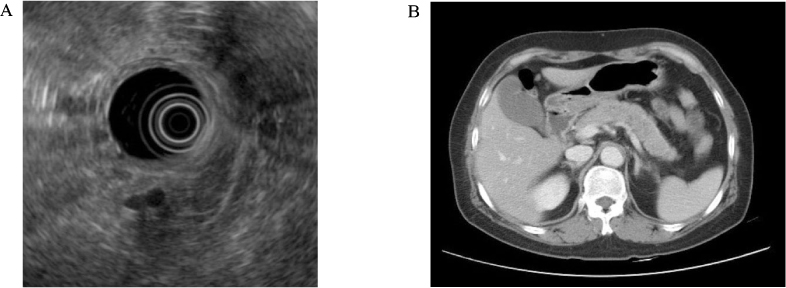
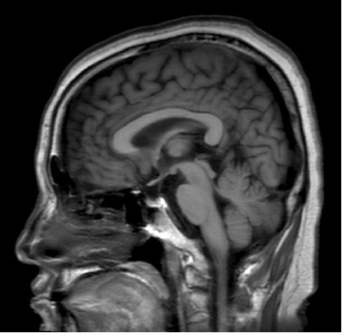
- Insulin autoimmune syndrome is one of the rare causes of hypoglycemia, and characterized by hyperinsulinemic hypoglycemia associated with high titer of antibodies to endogenous insulin. We report a case of insulin autoimmune syndrome in a 57-year-old woman, presenting with mental changes due to hypoglycemia. She had no history of diabetes or insulin administration. The serum C-peptide level was 4.69 ng/mL and the insulin concentration was 229.55 microU/mL, when fasting plasma glucose level was 32 mg/dL. The insulin-to-glucose ratio was 7.17, while there was no radiologic evidence of insulinoma. The insulin antibody level was over 100 microU/mL, resulting in the diagnosis of insulin autoimmune syndrome. Hormonal studies revealed partial hypopituitarism and a lack of glucagon-response to hypoglycemia. Hypoglycemia disappeared with replacement of prednisolone with levothyroxine therapy. Under secretion of growth hormone and of adrenocorticotropic hormone due to hypopituitarism were associated with insufficient counterregulation to hypoglycemia. One should keep in mind that insulin autoimmune syndrome or hypopituitarism is one cause of hypoglycemia in patients with no history of diabetes, and corticosteroid can be an effective treatment for both diseases.
MeSH Terms
Figure
Reference
-
1. Hirata Y, Ishizu H, Ouchi N, Motomura S, Abe M, Hara Y, Wakasugi H, Takahashi I, Takano M, Kawano H, Kanesaki T. Insulin autoimmunity in a case of spontaneous hypoglycemia. J Jpn Diabet Soc. 1970. 13:312–320.2. Uchigata Y, Hirata Y. Insulin autoimmune syndrome (IAS, Hirata disease). Ann Med Interne (Paris). 1999. 150:245–253.3. Lupsa BC, Chong AY, Cochran EK, Soos MA, Semple RK, Gorden P. Autoimmune forms of hypoglycemia. Medicine (Baltimore). 2009. 88:141–153.4. Uchigata Y, Eguchi Y, Takayama-Hasumi S, Omori Y. Insulin autoimmune syndrome (Hirata disease): clinical features and epidemiology in Japan. Diabetes Res Clin Pract. 1994. 22:89–94.5. McLean AM, Fairclough PD. Endoscopic ultrasound in the localisation of pancreatic islet cell tumours. Best Pract Res Clin Endocrinol Metab. 2005. 19:177–193.6. Fanelli C, Porcellati F, Rossetti P, Bolli GB. Glucagon: the effects of its excess and deficiency on insulin action. Nutr Metab Cardiovasc Dis. 2006. 16:S28–S34.7. Yoshikawa H, Kawai K, Inoue S, Murayama Y, Fujieda K, Kuzuya N, Fujita T, Koide Y, Yamashita K. Hyperglucagonemia of insulin autoimmune syndrome induced by methimazole in a patient with Graves' disease. Endocrinol Jpn. 1989. 36:125–134.8. Young A. Inhibition of glucagon secretion. Adv Pharmacol. 2005. 52:151–171.9. Boyle PJ, Cryer PE. Growth hormone, cortisol, or both are involved in defense against, but are not critical to recovery from, hypoglycemia. Am J Physiol. 1991. 260:E395–E402.10. Davis MR, Shamoon H. Counterregulatory adaptation to recurrent hypoglycemia in normal humans. J Clin Endocrinol Metab. 1991. 73:995–1001.11. Heller SR, Cryer PE. Reduced neuroendocrine and symptomatic responses to subsequent hypoglycemia after 1 episode of hypoglycemia in nondiabetic humans. Diabetes. 1991. 40:223–226.12. Arlt W. The approach to the adult with newly diagnosed adrenal insufficiency. J Clin Endocrinol Metab. 2009. 94:1059–1067.13. Tahrani AA, West TE, Macleod AF. An unusual cause of severe hypoglycaemia in type 1 diabetes mellitus. Antepartum pituitary failure: a case report and literature review. Exp Clin Endocrinol Diabetes. 2007. 115:136–138.14. Ghigo E, Aimaretti G, Corneli G. Diagnosis of adult GH deficiency. Growth Horm IGF Res. 2008. 18:1–16.15. Eguchi Y, Uchigata Y, Yao K, Yokoyama H, Hirata Y, Omori Y. Longitudinal changes of serum insulin concentration and insulin antibody features in persistent insulin autoimmune syndrome (Hirata's disease). Autoimmunity. 1994. 19:279–284.16. Virally ML, Guillausseau PJ. Hypoglycemia in adults. Diabetes Metab. 1999. 25:477–490.17. Schneider HJ, Aimaretti G, Kreitschmann-Andermahr I, Stalla GK, Ghigo E. Hypopituitarism. Lancet. 2007. 369:1461–1470.18. Hofeldt FD, Dippe S, Forsham PH. Diagnosis and classification of reactive hypoglycemia based on hormonal changes in response to oral and intravenous glucose administration. Am J Clin Nutr. 1972. 25:1193–1201.19. Samaan NA. Hypoglycemia secondary to endocrine deficiencies. Endocrinol Metab Clin North Am. 1989. 18:145–154.20. Regal M, Paramo C, Sierra SM, Garcia-Mayor RV. Prevalence and incidence of hypopituitarism in an adult Caucasian population in northwestern Spain. Clin Endocrinol (Oxf). 2001. 55:735–740.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anti-tuberculosis Treatment-Induced Insulin Autoimmune Syndrome
- A case of insulin autoimmune syndrome
- Insulin Autoimmune Syndrome with Diabetic Ketoacidosis
- A case of insulin autoimmune syndrome related to alpha-lipoic acid
- A Case of Primary Insulin Autoimmune Syndrome in a Patient Suspected of Having an Insulinoma