Korean J Pediatr Gastroenterol Nutr.
2011 Dec;14(Suppl 1):S25-S33. 10.5223/kjpgn.2011.14.Suppl1.S25.
Psychosocial Factors and Psychiatric Disorder in Childhood Chronic Abdominal Pain
- Affiliations
-
- 1Department of Psychiatry, Yonsei University College of Medicine, Seoul, Korea. dhsong@yuhs.ac
- KMID: 1451146
- DOI: http://doi.org/10.5223/kjpgn.2011.14.Suppl1.S25
Abstract
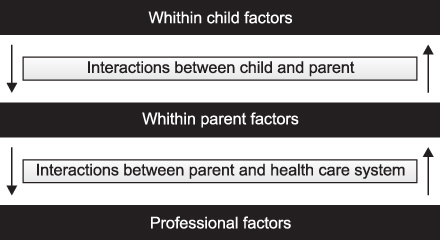
- Childhood chronic abdominal pain usually doesn't have an organic etiology. It may cause social impairment and emotional distress in children as well as their families. In view of cognitive and behavioral aspect, passive coping style, maladaptive social modeling, and reinforced secondary gain could contribute to the development and maintenance of pediatric somatization. Integrative etiological model includes biological factors due to the enteric sensitization process, psychosocial factors which encompass family influences, psychodevelomental vulnerability, and life event-related stress. These factors interact with each other and manifest as various psychosomatic symptoms. In the treatment of childhood chronic abdominal pain, multimodal treatment program, which includes cognitive behavioral therapeutic methods, emotional support, family education, selective serotonin reuptake inhibitor, and so on, is known to be most effective.
MeSH Terms
Figure
Reference
-
1. Di Lorenzo C, Colletti RB, Lehmann HP, Boyle JT, Gerson WT, Hyams JS, et al. Chronic abdominal pain in children: a clinical report of the American Academy of Pediatrics and the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2005. 40:245–248.
Article2. Hyams JS, Burke G, Davis PM, Rzepski B, Andrulonis PA. Abdominal pain and irritable bowel syndrome in adolescents: a community-based study. J Pediatr. 1996. 129:220–226.
Article3. Starfield B, Gross E, Wood M, Pantell R, Allen C, Gordon IB, et al. Psychosocial and psychosomatic diagnoses in primary care of children. Pediatrics. 1980. 66:159–167.4. Apley J, Naish N. Recurrent abdominal pains: a field survey of 1,000 school children. Arch Dis Child. 1958. 33:165–170.
Article5. Oster J. Recurrent abdominal pain, headache and limb pains in children and adolescents. Pediatrics. 1972. 50:429–436.
Article6. Kohli R, Li BU. Differential diagnosis of recurrent abdominal pain: new considerations. Pediatr Ann. 2004. 33:113–122.
Article7. Hyams JS, Hyman PE. Recurrent abdominal pain and the biopsychosocial model of medical practice. J Pediatr. 1998. 133:473–478.
Article8. Apley J. The child with recurrent abdominal pain. Pediatr Clin North Am. 1967. 14:63–72.
Article9. Hwang JB, Jeong SH. Practical Diagnostic Approaches to Chronic Abdominal Pain in Children and Adolescents. J Korean Med Assoc. 2009. 52:271–284.
Article10. Yang HR. New approach to chronic recurrent abdominal pain in children. Korean J Pediatr. 2006. 49:129–135.
Article11. Rasquin A, Di Lorenzo C, Forbes D, Guiraldes E, Hyams JS, Staiano A, et al. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology. 2006. 130:1527–1537.
Article12. Bufler P, Gross M, Uhlig HH. Recurrent abdominal pain in childhood. Dtsch Arztebl Int. 2011. 108:295–304.
Article13. Alfven G. One hundred cases of recurrent abdominal pain in children: diagnostic procedures and criteria for a psychosomatic diagnosis. Acta Paediatr. 2003. 92:43–49.
Article14. Campo JV, Jansen-McWilliams L, Comer DM, Kelleher KJ. Somatization in pediatric primary care: association with psychopathology, functional impairment, and use of services. J Am Acad Child Adolesc Psychiatry. 1999. 38:1093–1101.
Article15. Helgeland H, Sandvik L, Mathiesen KS, Kristensen H. Childhood predictors of recurrent abdominal pain in adolescence: A 13-year population-based prospective study. J Psychosom Res. 2010. 68:359–367.
Article16. Eminson DM. Medically unexplained symptoms in children and adolescents. Clin Psychol Rev. 2007. 27:855–871.
Article17. Campo JV, Fritsch SL. Somatization in children and adolescents. J Am Acad Child Adolesc Psychiatry. 1994. 33:1223–1235.
Article18. Schulte IE, Petermann F, Noeker M. Functional abdominal pain in childhood: from etiology to maladaptation. Psychother Psychosom. 2010. 79:73–86.
Article19. Sprenger L, Gerhards F, Goldbeck L. Effects of psychological treatment on recurrent abdominal pain in children - A meta-analysis. Clin Psychol Rev. 2011. 31:1192–1197.
Article20. Robinson JO, Alverez JH, Dodge JA. Life events and family history in children with recurrent abdominal pain. J Psychosom Res. 1990. 34:171–181.
Article21. Walker LS, Garber J, Smith CA, Van Slyke DA, Claar RL. The relation of daily stressors to somatic and emotional symptoms in children with and without recurrent abdominal pain. J Consult Clin Psychol. 2001. 69:85–91.
Article22. Elena Garralda M, Chalder T. Practitioner review: chronic fatigue syndrome in childhood. J Child Psychol Psychiatry. 2005. 46:1143–1151.
Article23. Campo JV, Bridge J, Ehmann M, Altman S, Lucas A, Birmaher B, et al. Recurrent abdominal pain, anxiety, and depression in primary care. Pediatrics. 2004. 113:817–824.
Article24. Campo JV, Di Lorenzo C, Chiappetta L, Bridge J, Colborn DK, Gartner JC Jr, et al. Adult outcomes of pediatric recurrent abdominal pain: do they just grow out of it? Pediatrics. 2001. 108:E1.25. Egger HL, Costello EJ, Erkanli A, Angold A. Somatic complaints and psychopathology in children and adolescents: stomach aches, musculoskeletal pains, and headaches. J Am Acad Child Adolesc Psychiatry. 1999. 38:852–860.
Article26. Campo JV, Fritz G. A management model for pediatric somatization. Psychosomatics. 2001. 42:467–476.
Article27. Anbar RD. Self-hypnosis for the treatment of functional abdominal pain in childhood. Clin Pediatr (Phila). 2001. 40:447–451.
Article28. Walker LS, Williams SE, Smith CA, Garber J, Van Slyke DA, Lipani TA. Parent attention versus distraction: impact on symptom complaints by children with and without chronic functional abdominal pain. Pain. 2006. 122:43–52.
Article29. Levy RL, Langer SL, Walker LS, Romano JM, Christie DL, Youssef N, et al. Cognitive-behavioral therapy for children with functional abdominal pain and their parents decreases pain and other symptoms. Am J Gastroenterol. 2010. 105:946–956.
Article30. Vlieger AM, Menko-Frankenhuis C, Wolfkamp SC, Tromp E, Benninga MA. Hypnotherapy for children with functional abdominal pain or irritable bowel syndrome: a randomized controlled trial. Gastroenterology. 2007. 133:1430–1436.
Article31. Campo JV, Perel J, Lucas A, Bridge J, Ehmann M, Kalas C, et al. Citalopram treatment of pediatric recurrent abdominal pain and comorbid internalizing disorders: an exploratory study. J Am Acad Child Adolesc Psychiatry. 2004. 43:1234–1242.
Article32. Hotopf M, Carr S, Mayou R, Wadsworth M, Wessely S. Why do children have chronic abdominal pain, and what happens to them when they grow up? Population based cohort study. BMJ. 1998. 316:1196–1200.
Article33. Hotopf M, Wilson-Jones C, Mayou R, Wadsworth M, Wessely S. Childhood predictors of adult medically unexplained hospitalisations. Results from a national birth cohort study. Br J Psychiatry. 2000. 176:273–280.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Psychosocial Factors in Patients with Chronic Kidney Disease
- Psychosocial treatment of psychiatric disorders of the elderly
- Practical Diagnostic Approaches to Chronic Abdominal Pain in Children and Adolescents
- Chronic Abdominal Pain-related Childhood Functional Gastrointestinal Disorders Based on the Rome III Criteria in Korea
- Psychosocial Stressors and Ratings in Child and Adolescent Psychiatric Disorders