Clin Orthop Surg.
2010 Mar;2(1):22-27. 10.4055/cios.2010.2.1.22.
Operations about Hip in Human Immunodeficiency Virus-Positive Patients
- Affiliations
-
- 1Department of Orthopedic Surgery, Seoul National University College of Medicine, Seoul, Korea. oskim@snu.ac.kr
- KMID: 1110345
- DOI: http://doi.org/10.4055/cios.2010.2.1.22
Abstract
-
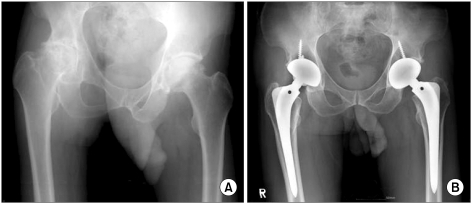
BACKGROUND: The number of human immunodeficiency virus (HIV)-infected patients is increasing constantly, and it is well known that there is a significantly high prevalence of osteonecrosis of the femoral head in HIV-infected patients. Therefore, it is important to develop methods that can ensure the safety of both the patients and medical personnel who participate in surgery on HIV-infected patients. Recently, the authors performed 8 procedures on 5 HIV-infected patients. This paper reports our experience.
METHODS
This study examined the medical records and radiological studies of 5 HIV-infected patients who had undergone surgery around the hip joint from January, 2005 to September, 2007. During the procedures, their mean age was 38.6 years (range, 23 to 53 years) and all were male. Four of them were under an anti-retroviral therapy program. The reasons for the operations were nonunion of the femoral shaft after trauma in two patients and osteonecrosis of both femoral heads in three. One autologous bone grafting, one screw fixation with autologous bone grafting, five total hip replacement arthroplasties, and one multiple drilling were performed. All procedures were carried out according to the guidelines of HIV infection control made by the Korea Centers for Disease Control and Prevention. The mean follow-up period was 16.6 months (range, 4 to 37 months).
RESULTS
The preoperative CD4 count was 130 in one patient, and 200 to 499 in the other 4. The viral loads were 15100 and 420 in two patients, and negative in the other 3. Bony union was achieved in those who had undergone autologous bone grafting. There were significant improvements in both the Harris Hip Score and functional state in those who had total hip replacement arthroplasty. There were no immediate postoperative complications, such as infection. During the follow-up period, one patient died from esophageal variceal bleeding. However, no surgery-related complications were observed in the other 4 patients.
CONCLUSIONS
There were no significant complications in HIV-infected patients after the operations around the hip joint when their preoperative immunity was optimal. In addition, the safety of medical personnel can be assured when the operation is performed in line with the guidelines of HIV infection control.
Keyword
MeSH Terms
-
Adult
*Arthroplasty, Replacement, Hip/adverse effects
Bone Transplantation
CD4 Lymphocyte Count
Femoral Fractures/complications/*surgery
Femur Head Necrosis/complications/*surgery
Fractures, Ununited/complications/*surgery
HIV Infections/*complications/immunology/transmission/virology
Humans
Infectious Disease Transmission, Patient-to-Professional/prevention & control
Male
Middle Aged
Postoperative Complications
Viral Load
Young Adult
Figure
Reference
-
1. Korea Centers for Disease Control and Prevention. Annual Report from the Division of HIV and TB control. 2008. Seoul: Korea Centers for Disease Control and Prevention.2. Miller KD, Masur H, Jones EC, et al. High prevalence of osteonecrosis of the femoral head in HIV-infected adults. Ann Intern Med. 2002; 137(1):17–25. PMID: 12093241.
Article3. Morse CG, Mican JM, Jones EC, et al. The incidence and natural history of osteonecrosis in HIV-infected adults. Clin Infect Dis. 2007; 44(5):739–748. PMID: 17278070.
Article4. Keruly JC, Chaisson RE, Moore RD. Increasing inicidence of avascular necrosis of the hip in HIV-infected patients. J Acquir Immune Defic Syndr. 2001; 28(1):101–102. PMID: 11579286.5. Scribner AN, Troia-Cancio PV, Cox BA, et al. Osteonecrosis in HIV: a case-control study. J Acquir Immune Defic Syndr. 2000; 25(1):19–25. PMID: 11064500.
Article6. Ries MD, Barcohana B, Davidson A, Jergesen HE, Paiement GD. Association between human immunodeficiency virus and osteonecrosis of the femoral head. J Arthroplasty. 2002; 17(2):135–139. PMID: 11847610.
Article7. Gutierrez F, Padilla S, Masia M, et al. Osteonecrosis in patients infected with HIV: clinical epidemiology and natural history in a large case series from Spain. J Acquir Immune Defic Syndr. 2006; 42(3):286–292. PMID: 16763523.8. Lehman CR, Ries MD, Paiement GD, Davidson AB. Infection after total joint arthroplasty in patients with human immunodeficiency virus or intravenous drug use. J Arthroplasty. 2001; 16(3):330–335. PMID: 11307131.
Article9. Parvizi J, Sullivan TA, Pagnano MW, Trousdale RT, Bolander ME. Total joint arthroplasty in human immunodeficiency virus-positive patients: an alarming rate of early failure. J Arthroplasty. 2003; 18(3):259–264. PMID: 12728415.
Article10. Hoekman P, van de Perre P, Nelissen J, Kwisanga B, Bogaerts J, Kanyangabo F. Increased frequency of infection after open reduction of fractures in patients who are seropositive for human immunodeficiency virus. J Bone Joint Surg Am. 1991; 73(5):675–679. PMID: 2045392.
Article11. Paiement GD, Hymes RA, LaDouceur MS, Gosselin RA, Green HD. Postoperative infections in asymptomatic HIV-seropositive orthopedic trauma patients. J Trauma. 1994; 37(4):545–550. PMID: 7932883.
Article12. Harrison WJ, Lewis CP, Lavy CB. Wound healing after implant surgery in HIV-positive patients. J Bone Joint Surg Br. 2002; 84(6):802–806. PMID: 12211668.
Article13. Mahoney CR, Glesby MJ, DiCarlo EF, Peterson MG, Bostrom MP. Total hip arthroplasty in patients with human immunodeficiency virus infection: pathologic findings and surgical outcomes. Acta Orthop. 2005; 76(2):198–203. PMID: 16097544.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Ankylosing Spondylitis in a Patient with Human Immunodeficiency Virus
- Avascular Necrosis of Femoral Head Treated by Total Hip Replacement in AIDS Patients: A Case Report
- Sequential Bilateral Rapid Destructive Inflammatory Coxarthrosis in a Patient with Human Immunodeficiency Virus
- A Case of Management of Benign Lymphoepithelial Cysts of the Parotid Gland in Patient Infected with Human Immunodeficiency Virus
- Molecular Epidemiology of Human Immunodeficiency Virus