Korean J Ophthalmol.
2007 Sep;21(3):178-184. 10.3341/kjo.2007.21.3.178.
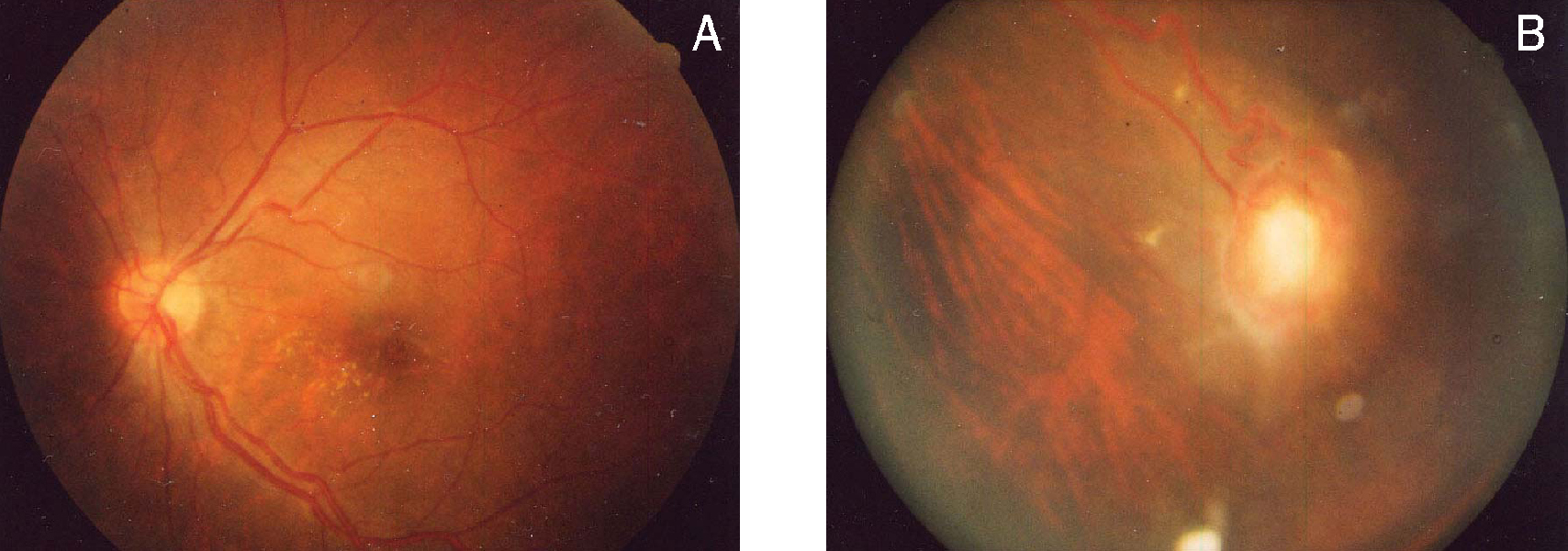
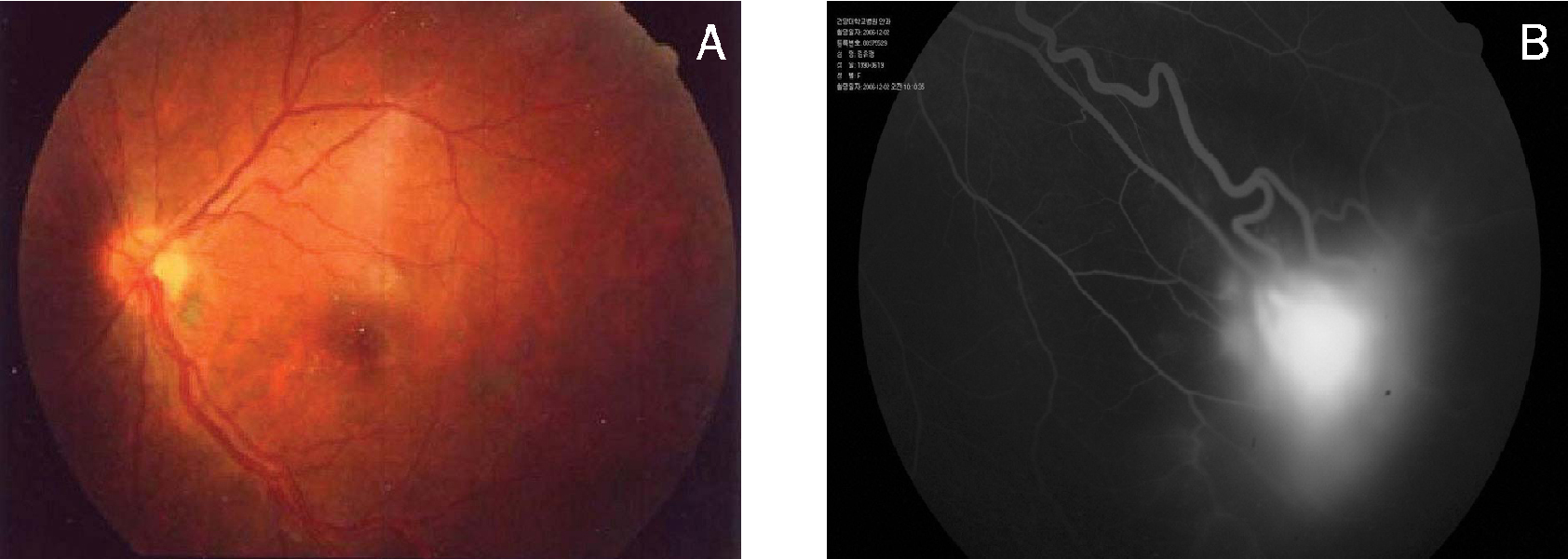
Retinal Capillary Hemangioma Treated with Verteporfin Photodynamic Therapy and Intravitreal Triamcinolone Acetonide
- Affiliations
-
- 1Department of Ophthalmology, College of Medicine, Konyang University, Myung Gok Eye Research Institute, Daejeon, Korea. ophthal73@hanmail.net
- KMID: 1099037
- DOI: http://doi.org/10.3341/kjo.2007.21.3.178
Abstract
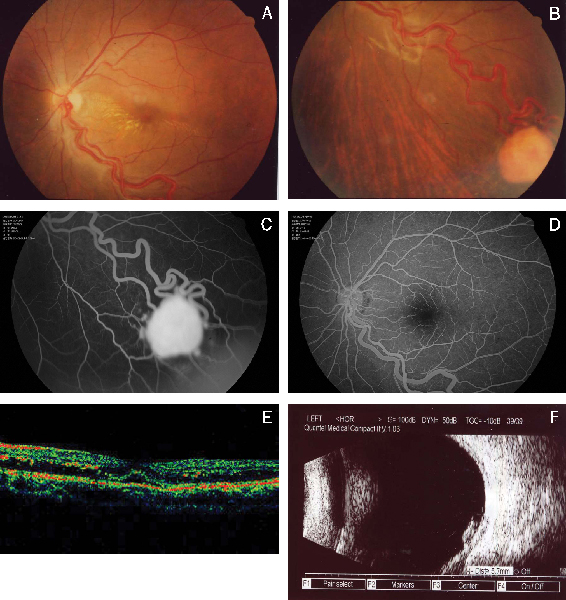
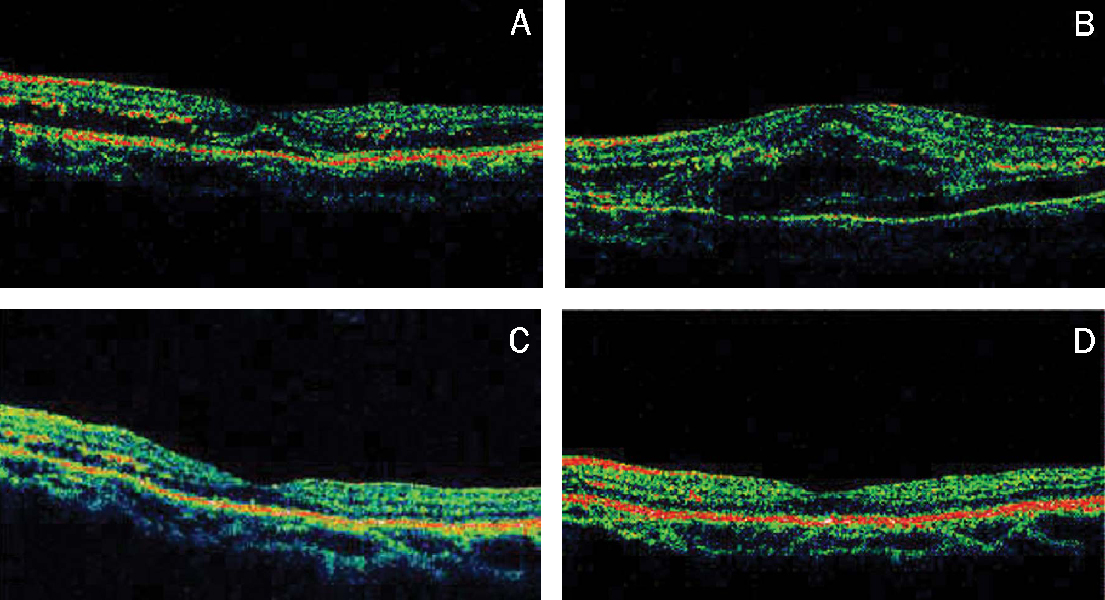
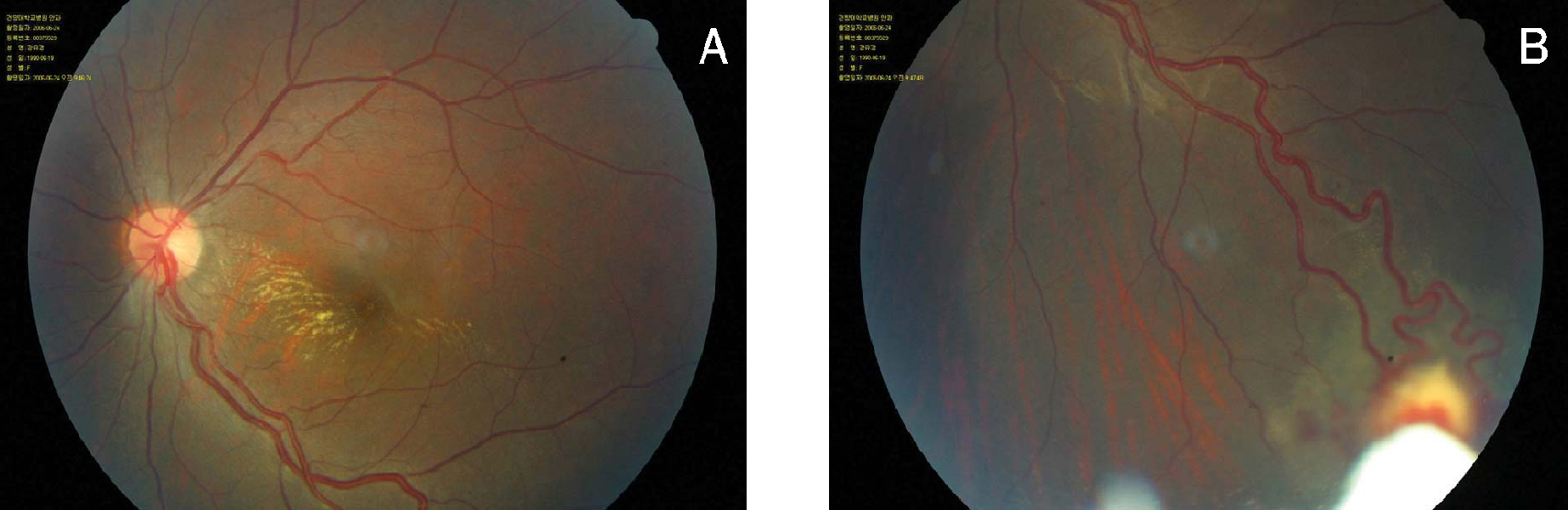
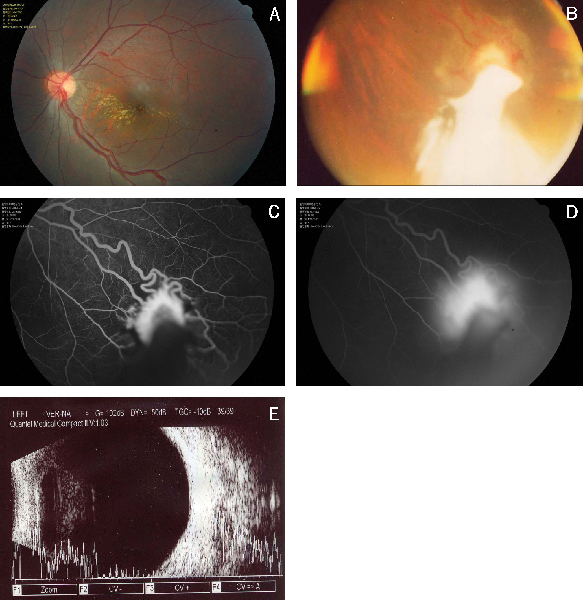
- PURPOSE: To report a case of retinal capillary hemangioma treated with verteporfin photodynamic therapy combined with intravitreal triamcinolone acetonide. METHODS: A 15-year-old female presented with metamorphopsia in the left eye for 7 days. Examination showed peripheral endophytic retinal capillary hemangioma, macular edema, and a best-corrected visual acuity of 20/50. The hemangioma and macular edema were treated with verteporfin photodynamic therapy and intravitreal triamcinolone acetonide. RESULTS: After 5 months of follow-up, involution of the hemangioma, reduction of macular edema, decrease of the feeder and draining vessel diameter, and improvement of best-corrected visual acuity to 20/25 was seen. CONCLUSIONS: This verteporfin photodynamic therapy combined with intravitreal triamcinolone acetonide appeared to cause involution of the hemangioma with reduction in macular edema and improvement in visual acuity.
MeSH Terms
-
Adolescent
Female
Fundus Oculi
Glucocorticoids/*administration & dosage/therapeutic use
Hemangioma, Capillary/diagnosis/*drug therapy
Humans
Injections
*Photochemotherapy
Photosensitizing Agents/*therapeutic use
Porphyrins/*therapeutic use
Retinal Neoplasms/diagnosis/*drug therapy
Tomography, Optical Coherence
Triamcinolone Acetonide/*administration & dosage/therapeutic use
Ultrasonography
Vitreous Body
Figure
Cited by 1 articles
-
Clinical Results of Various Treatments for Retinal Capillary Hemangioma
Yeo-Kyoung Won, Min-Woo Lee, Yong-Il Shin, Jung-Yeul Kim, Young-Joon Jo
Korean J Ophthalmol. 2020;34(2):133-142. doi: 10.3341/kjo.2019.0075.
Reference
-
1. Singh AD, Nouri M, Shield CL, et al. Retinal capillary hemangioma: a comparison of sporadic cases and cases associated with von Hippel-Lindau disease. Ophthalmology. 2001. 108:1907–1911.2. Singh AD, Shields CL, Shields JA. von Hippel-Lindau disease. Surv Ophthalmol. 2001. 46:117–142.3. Moskowitz C, Edelstein C, Oh M, et al. Retinal capillary hemangioma in von Hippel-Lindau disease. Can J Ophthalmol. 2005. 40:192–194.4. Ryan SJ. Hinz BJ, Schachat AP, editors. Capillary hemangioma of the retina and von Hippel-Lindau diease. Retina. 2006. v.1:4th ed. Mosby: Elsevier Inc.;chap. 24.5. Gass JDM. Stereoscopic atlas of macular disease. Diagnosis and treatment. 1997. 4th ed. St. Louis: Mosby;850–865.6. Ridley M, Green J, Johnson G. Retinal angiomatosis: the ocular manifestations of von Hippel-Lindau disease. Can J Ophthalmol. 1986. 21:276–283.7. Mcdonald HR, Schatz H, Johnson RN, et al. Vitrectomy in eyes with peripheral retinal angioma associated with traction macular detachment. Ophthalmology. 1996. 103:329–335.8. Rodriguez-Coleman H, Spaide RF, Yannuzzi LA. Treatment of angiomatous lesions of the retina with photodynamic therapy. Retina. 2002. 22:228–232.9. Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin. Arch Ophthalmol. 1999. 117:1329–1345.10. Verteporfin in Photodynamic Therapy Study Group. Verteporfin therapy of subfoveal choroidal neovascularization in age-related macular degeneration: two-year results of a randomized clinical trial including lesions with occult with no classic choroidal neovascularization-verteporfin in photodynamic therapy report 2. Am J Ophthalmol. 2001. 131:541–560.11. Singh AD, Shields JA, Shields CL. Solitary retinal capillary hemangioma: hereditary (von Hippel-Lindau disease) or non hereditary? Arch Ophthalmol. 2001. 119:232–234.12. Webster AR, Maher ER, Bird AC, Moore AT. Risk of multisystem disease in isolated ocular angioma (haemangioblastoma). J Med Genet. 2000. 37:62–63.13. Annesley WH Jr, Leonard BC, Shield JA, et al. Fifteen year review of treated cases of retinal angiomatosis. Trans Am Acad Ophthalmol Otolaryngol. 1977. 83:446–453.14. Ridley M, Green J, Johnson G. Retinal angiomatosis: the ocular manifestations of von Hippel-Lindau disease. Can J Ophthalmol. 1986. 21:276–283.15. Shields JA, Shields CL. Intraocular tumors, A text and atlas. 1992. Philadelphia: WB Saunders;393–419.16. Husain D, Gragoudas ES, Miller JW. Principles and practice of ophthalmology. 2000. 2nd ed. Philadelphia: WB Saunders;577–587.17. Gass JDM. Treatment of retinal vascular anomalies. Trans Am Acad Ophthalmol Otolaryngol. 1977. 83:432–442.18. Welch RB. von Hippel-Lindau disease: the recognition and treatment of early angiomatosis retinae and the use of cryosurgery as an adjunct to therapy. Trans Am Ophthalmol Soc. 1970. 68:367–424.19. Atebara NH. Retinal capillary haemangioma treated with verteporfin photodynamic therapy. Am J Ophthalmol. 2002. 134:788–790.20. Ryan SJ. Hinz BJ, Schachat AP, editors. Capillary hemangioma of the retina and von Hippel-Lindau diease. Retina. 2006. v. 1:4th ed. Mosby: Elsevier Inc.;chap. 65.21. Spaide RF, Sorenson J, Maranan L. Combined photodynamic therapy with verteporfin and intravitreal triamcinolone acetonide for choroidal neovascularization. Ophthalmology. 2003. 110:1517–1525.22. Ryan SJ. Hinz BJ, Schachat AP, editors. Capillary hemangioma of the retina and von Hippel-Lindau diease. Retina. 2006. v. 1:4th ed. Mosby: Elsevier Inc.;chap. 55.23. Penfold PL, Wen L, Madigan MC, et al. Modulation of permeability and adhesion molecules expression by human choroidal endothelial cells. Invest Ophthalmol Vis Sci. 2002. 3125–3130.24. Wang YS, Friedrichs U, Eichler W, et al. Inhibitory effects of triamcinolone acetonide on bFGF-induced migration and tube formation in choroidal microvascular endothelial cells. Graefes Arch Clin Exp Ophthalmol. 2002. 240:42–48.25. Ciulla TA, Criswell MH, Danis RP, Hill TE. Intravitreal triamcinolone acetonide inhibits choroidal neovascularization in a laser-treated rat model. Arch Ophthalmol. 2001. 119:399–404.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Photodynamic Therapy and Intravitreal Triamcinolone Acetonide on Choroidal Neovascularization in Age-related Macular Degeneration
- A Case of Intralenticular Triamcinolone Complicated by Intravitreal Triamcinolone Acetonide Injection
- Different Effect of IVTA in the Management of Macular Edema Secondary to Perfusion and Ischemic Type BRVO
- Intravitreal Triamcinolone Versus Bevacizumab for Treatment of Macular Edema Secondary to Branch Retinal Vein Occlusion
- The Effect of Intravitreal Triamcinolone Acetonide on Cystoid Macular Edema