Korean J Radiol.
2011 Apr;12(2):176-186. 10.3348/kjr.2011.12.2.176.
Concurrent Chemotherapy and Pulsed High-Intensity Focused Ultrasound Therapy for the Treatment of Unresectable Pancreatic Cancer: Initial Experiences
- Affiliations
-
- 1Department of Radiology and the Institute of Radiation Medicine, Seoul National University Hospital, Seoul 110-744, Korea. bichoi@snu.ac.kr
- 2Department of Internal Medicine, Seoul National University Hospital, Seoul 110-744, Korea.
- 3Department of Medicine, University of Washington Medical Center, Seattle, USA.
- KMID: 1088562
- DOI: http://doi.org/10.3348/kjr.2011.12.2.176
Abstract
OBJECTIVE
This study was performed to evaluate the potential clinical value of concurrent chemotherapy and pulsed high intensity focused ultrasound (HIFU) therapy (CCHT), as well as the safety of pulsed HIFU, for the treatment of unresectable pancreatic cancer.
MATERIALS AND METHODS
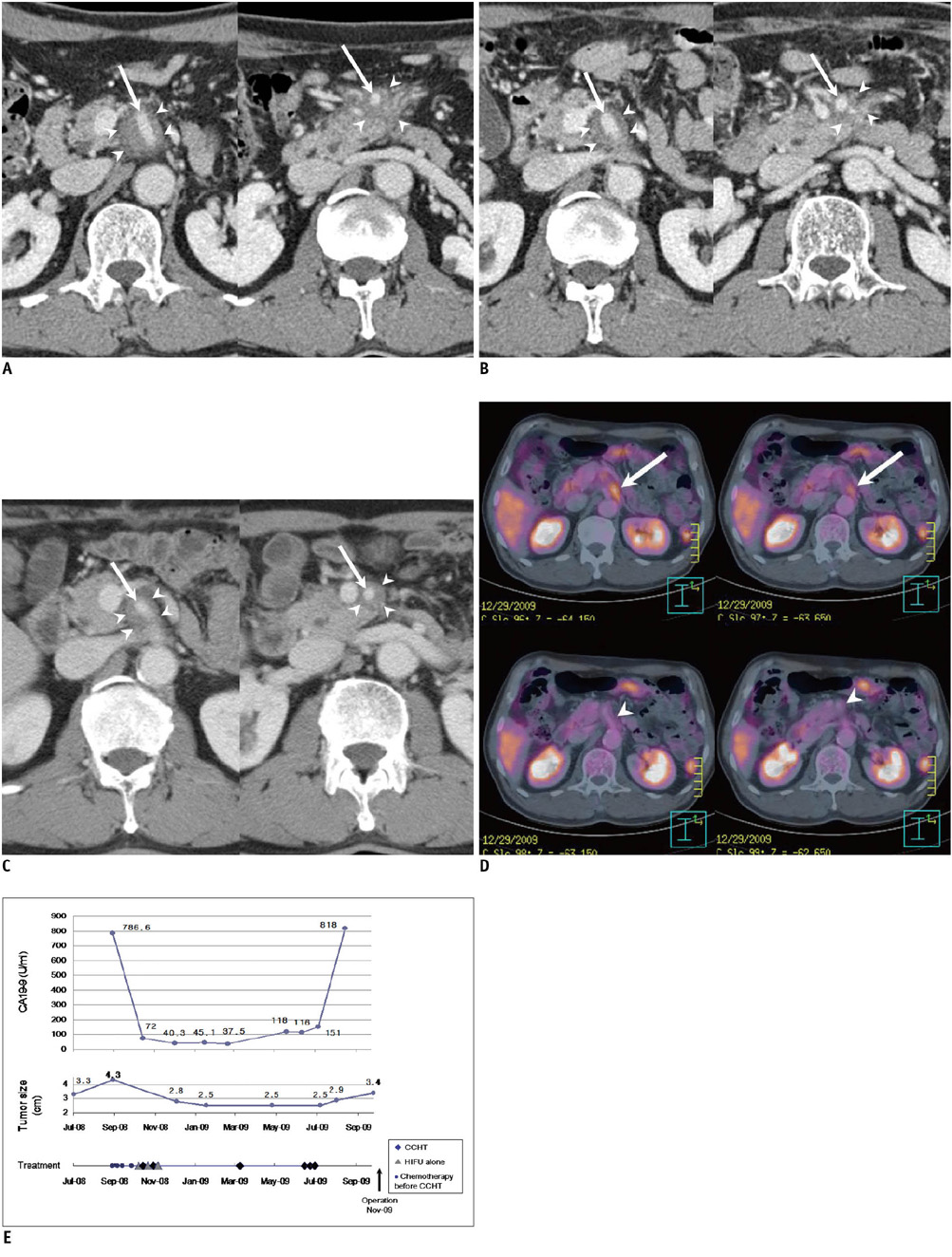
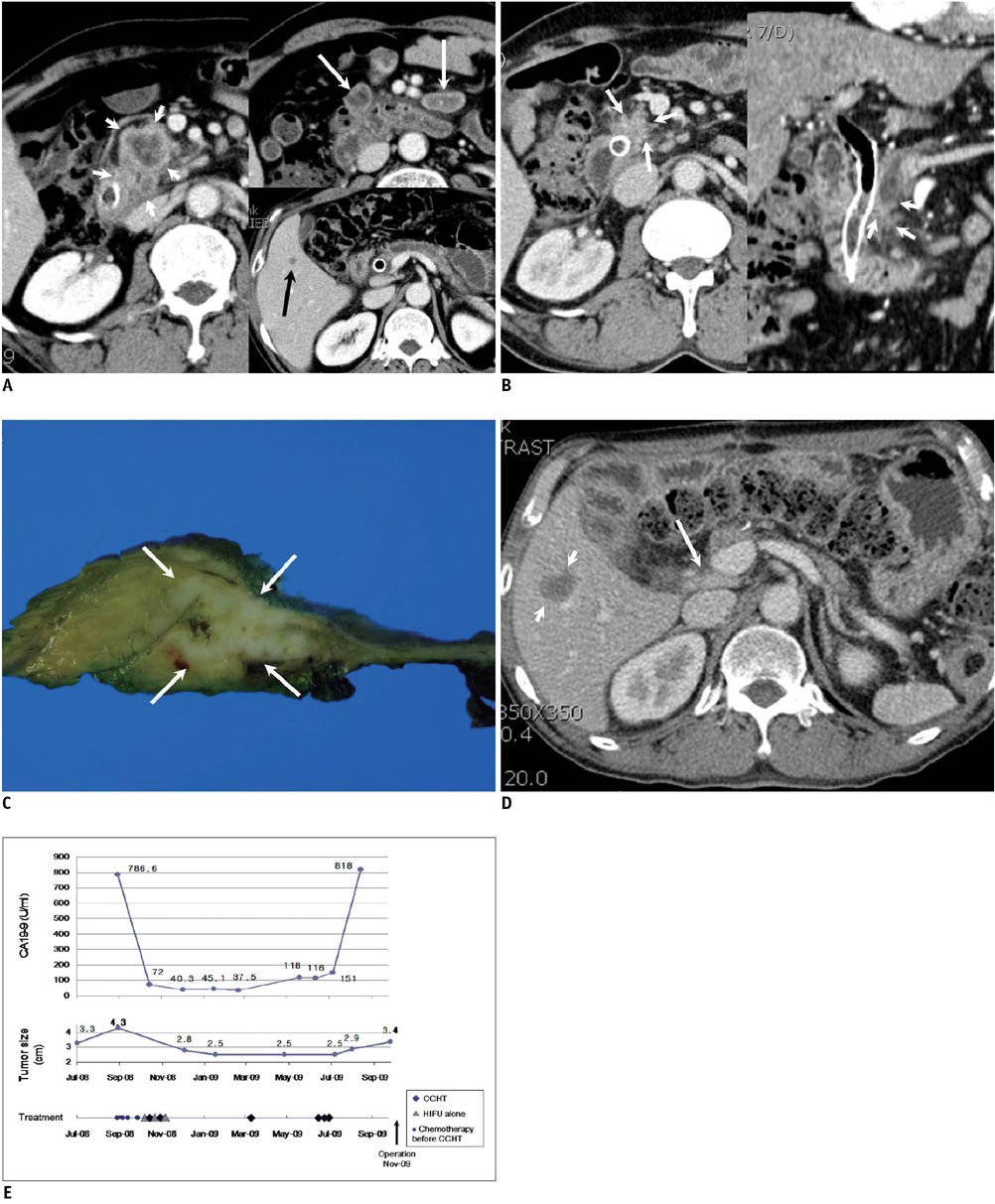
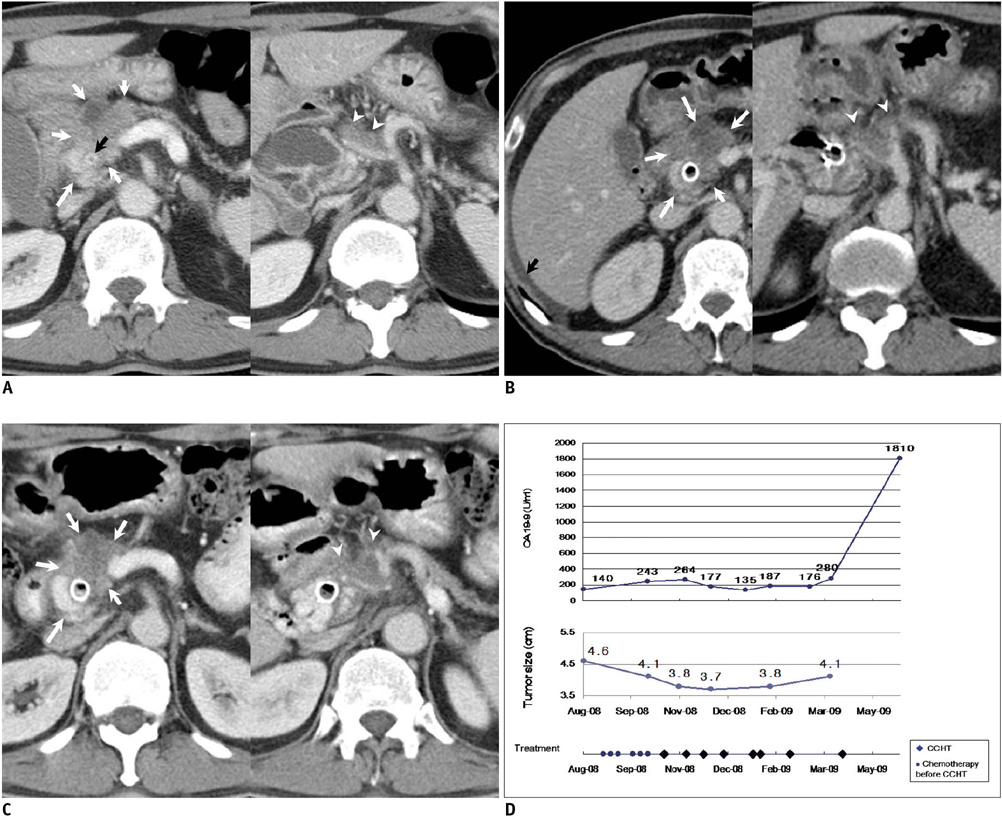
Twelve patients were treated with HIFU from October 2008 to May 2010, and three of them underwent CCHT as the main treatment (the CCHT group). The overall survival (OS), the time to tumor progression (TTP), the complications and the current performance status in the CCHT and non-CCHT groups were analyzed. Nine patients in the non-CCHT group were evaluated to determine why CCHT could not be performed more than twice.
RESULTS
The OS of the three patients in the CCHT group was 26.0, 21.6 and 10.8 months, respectively, from the time of diagnosis. Two of them were alive at the time of preparing this manuscript with an excellent performance status, and one of them underwent a surgical resection one year after the initiation of CCHT. The TTP of the three patients in the CCHT group was 13.4, 11.5 and 9.9 months, respectively. The median OS and TTP of the non-CCHT group were 10.3 months and 4.4 months, respectively. The main reasons why the nine patients of the non-CCHT group failed to undergo CCHT more than twice were as follows: pancreatitis (n = 1), intolerance of the pain during treatment (n = 4), palliative use of HIFU for pain relief (n = 1) and a poor physical condition due to disease progression (n = 3). No major complications were encountered except one case of pancreatitis.
CONCLUSION
This study shows that CCHT is a potentially effective and safe modality for the treatment of unresectable pancreatic cancer.
MeSH Terms
Figure
Reference
-
1. Kim YS, Rhim H, Choi MJ, Lim HK, Choi D. High-intensity focused ultrasound therapy: an overview for radiologists. Korean J Radiol. 2008. 9:291–302.2. Wu F, Wang ZB, Zhu H, Chen WZ, Zou JZ, Bai J, et al. Feasibility of US-guided high-intensity focused ultrasound treatment in patients with advanced pancreatic cancer: initial experience. Radiology. 2005. 236:1034–1040.3. Cunningham D, Chau I, Stocken DD, Valle JW, Smith D, Steward W, et al. Phase III randomized comparison of gemcitabine versus gemcitabine plus capecitabine in patients with advanced pancreatic cancer. J Clin Oncol. 2009. 27:5513–5518.4. Herrmann R, Bodoky G, Ruhstaller T, Glimelius B, Bajetta E, Schuller J, et al. Gemcitabine plus capecitabine compared with gemcitabine alone in advanced pancreatic cancer: a randomized, multicenter, phase III trial of the Swiss Group for Clinical Cancer Research and the Central European Cooperative Oncology Group. J Clin Oncol. 2007. 25:2212–2217.5. Park JK, Ryu JK, Lee JK, Yoon WJ, Lee SH, Kim YT, et al. Gemcitabine chemotherapy versus 5-fluorouracil-based concurrent chemoradiotherapy in locally advanced unresectable pancreatic cancer. Pancreas. 2006. 33:397–402.6. Park BB, Park JO, Lee HR, Lee J, Choi DW, Choi SH, et al. A phase II trial of gemcitabine plus capecitabine for patients with advanced pancreatic adenocarcinoma. Cancer Chemother Pharmacol. 2007. 60:489–494.7. Wu F, Chen WZ, Bai J, Zou JZ, Wang ZL, Zhu H, et al. Pathological changes in human malignant carcinoma treated with high-intensity focused ultrasound. Ultrasound Med Biol. 2001. 27:1099–1106.8. Li JJ, Gu MF, Luo GY, Liu LZ, Zhang R, Xu GL. Complications of high intensity focused ultrasound for patients with hepatocellular carcinoma. Technol Cancer Res Treat. 2009. 8:217–224.9. Li JJ, Xu GL, Gu MF, Luo GY, Rong Z, Wu PH, et al. Complications of high intensity focused ultrasound in patients with recurrent and metastatic abdominal tumors. World J Gastroenterol. 2007. 13:2747–2751.10. Dromi S, Frenkel V, Luk A, Traughber B, Angstadt M, Bur M, et al. Pulsed-high intensity focused ultrasound and low temperature-sensitive liposomes for enhanced targeted drug delivery and antitumor effect. Clin Cancer Res. 2007. 13:2722–2727.11. Poff JA, Allen CT, Traughber B, Colunga A, Xie J, Chen Z, et al. Pulsed high-intensity focused ultrasound enhances apoptosis and growth inhibition of squamous cell carcinoma xenografts with proteasome inhibitor bortezomib. Radiology. 2008. 248:485–491.12. Wang RS, Liu LX, Gu YH, Lin QF, Guo RH, Shu YQ. The effect of endostatin and gemcitabine combined with HIFU on the animal xenograft model of human pancreatic cancer. Biomed Pharmacother. 2010. 64:309–312.13. Zhao H, Yang G, Wang D, Yu X, Zhang Y, Zhu J, et al. Concurrent gemcitabine and high-intensity focused ultrasound therapy in patients with locally advanced pancreatic cancer. Anticancer Drugs. 2010. 21:447–452.14. Xiong LL, Hwang JH, Huang XB, Yao SS, He CJ, Ge XH, et al. Early clinical experience using high intensity focused ultrasound for palliation of inoperable pancreatic cancer. JOP. 2009. 10:123–129.15. Hwang JH, Wang YN, Warren C, Upton MP, Starr F, Zhou Y, et al. Preclinical in vivo evaluation of an extracorporeal HIFU device for ablation of pancreatic tumors. Ultrasound Med Biol. 2009. 35:967–975.16. White RR, Hurwitz HI, Morse MA, Lee C, Anscher MS, Paulson EK, et al. Neoadjuvant chemoradiation for localized adenocarcinoma of the pancreas. Ann Surg Oncol. 2001. 8:758–765.17. Wolff RA. Neoadjuvant chemoradiation for localized adenocarcinoma of the pancreas: great logic, grim reality. Ann Surg Oncol. 2001. 8:747–748.18. Paparel P, Chapelon JY, Bissery A, Chesnais S, Curiel L, Gelet A. Influence of the docetaxel administration period (neoadjuvant or concomitant) in relation to HIFU treatment on the growth of Dunning tumors: results of a preliminary study. Prostate Cancer Prostatic Dis. 2008. 11:181–186.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long Term Complete Response of Unresectable Locally Advanced Pancreatic Cancer after CCRT and Gemcitabine Chemotherapy
- Long-term Survivor of Unresectable Pancreatic Cancer Treated with Concurrent Chemoradiotherapy
- Neoadjuvant Therapy for Resectable or Borderline Resectable Pancreatic Cancer
- Current and Future Clinical Applications of High-Intensity Focused Ultrasound (HIFU) for Pancreatic Cancer
- Second Line Chemotherapy for Pancreatic Cancer