Korean J Radiol.
2008 Aug;9(4):340-347. 10.3348/kjr.2008.9.4.340.
Radiofrequency Ablation Treatment for Renal Cell Carcinoma: Early Clinical Experience
- Affiliations
-
- 1Department of Radiology, Dong-A University College of Medicine, Busan, Korea. cerub@chollian.net
- 2Departments of Urology, Dong-A University College of Medicine, Busan, Korea.
- KMID: 1076460
- DOI: http://doi.org/10.3348/kjr.2008.9.4.340
Abstract
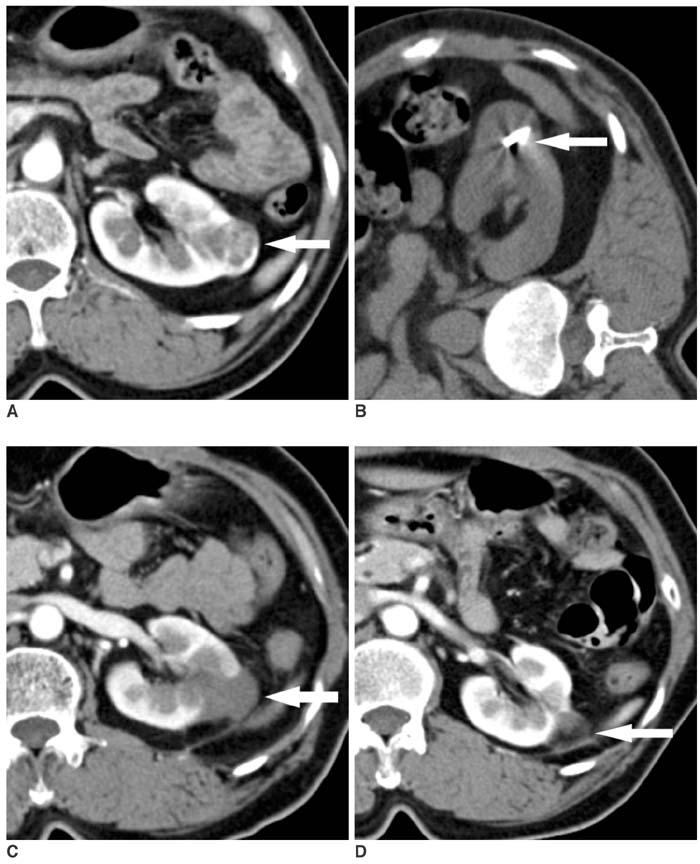
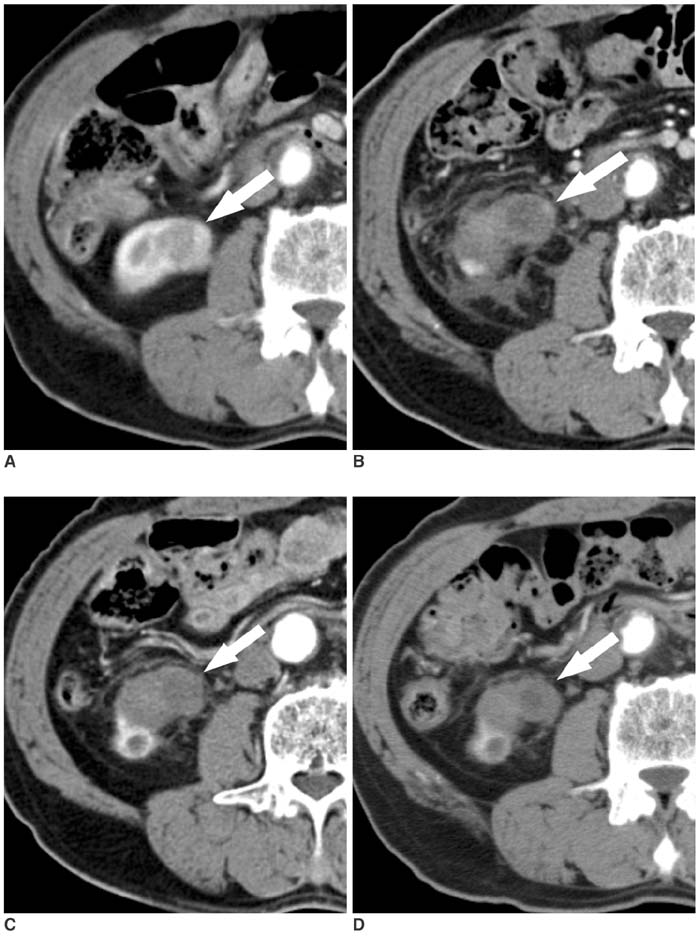
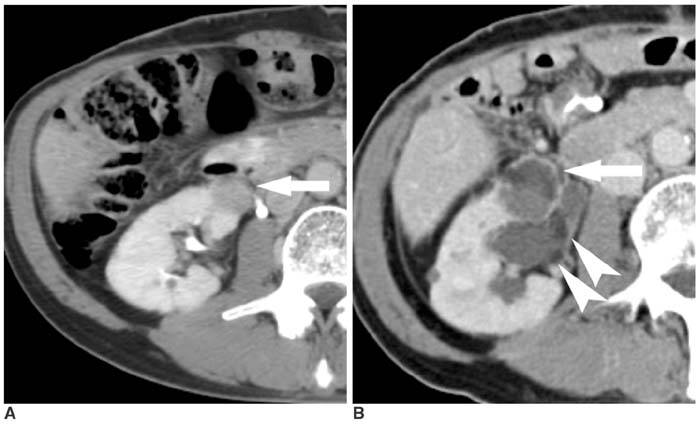
OBJECTIVE
To evaluate the early clinical experience associated with radiofrequency (RF) ablation in patients with renal cell carcinoma (RCC). MATERIALS AND METHODS: The RF ablation treatment was performed on 17 tumors from 16 patients (mean age, 60.5 years; range, 43-73 years) with RCC. The treatment indications were localized, solid renal mass, comorbidities, high operation risk, and refusal to perform surgery. All tumors were treated by a percutaneous CT (n = 10), followed by an US-guided (n = 2), laparoscopy-assisted US (n = 2), and an open (n = 2) RF ablation. Furthermore, patients underwent a follow-up CT at one day, one week, one month, three and six months, and then every six months from the onset of treatment. We evaluated the technical success, technical effectiveness, ablation zone, benign periablation enhancement, irregular peripheral enhancement, and complications. RESULTS: All 17 exophytic tumors (mean size, 2.2 cm; range, 1.1-5.0 cm) were completely ablated. Technical success and effectiveness was achieved in all cases and the mean follow-up period was 23.8 months (range, 17-33 months). A local recurrence was not detected in any of the cases; however, five patients developed complications as a result of treatment, including hematuria (n = 2), mild thermal injury of the psoas muscle (n = 1), mild hydronephrosis (n = 1), and fistula formation (n = 1). CONCLUSION: The RF ablation is an alternative treatment for exophytic RCCs and represents a promising treatment for some patients with small RCCs.
Keyword
MeSH Terms
Figure
Reference
-
1. Greenlee RT, Murray T, Bolden S, Wingo PA. Cancer statistics, 2000. CA Cancer J Clin. 2000. 50:7–33.2. Rendon RA, Stanietzky N, Panzarella T, Robinette M, Klotz LH, Thurston W, et al. The natural history of small renal masses. J Urol. 2000. 164:1143–1147.3. Duque JL, Loughlin KR, O'Leary MP, Kumar S, Richie JP. Partial nephrectomy: alternative treatment for selected patients with renal cell carcinoma. Urology. 1998. 52:584–590.4. Nakada SY, McDougall EM, Clayman RV. Laparoscopic extirpation of renal cell cancer: feasibility, questions, and concerns. Semin Surg Oncol. 1996. 12:100–112.5. Zagoria RJ. Imaging-guided radiofrequency ablation of renal masses. Radiographics. 2004. 24:S59–S71.6. Goldberg SN, Grassi CJ, Cardella JF, Charboneau JW, Dodd GD 3rd, Dupuy DE, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria. Radiology. 2005. 235:728–739.7. Rossi S, Buscarini E, Garbagnati F, Di Stasi M, Quaretti P, Rago M, et al. Percutaneous treatment of small hepatic tumors by an expandable RF needle electrode. AJR Am J Roentgenol. 1998. 170:1015–1022.8. Solbiati L, Goldberg SN, Ierace T, Livraghi T, Meloni F, Dellanoce M, et al. Hepatic metastases: percutaneous radiofrequency ablation with cooled-tip electrodes. Radiology. 1997. 205:367–373.9. Anzai Y, Lufkin R, DeSalles A, Hamilton DR, Farahani K, Black KL. Preliminary experience with MR-guided thermal ablation of brain tumors. AJNR Am J Neuroradiol. 1995. 16:39–48.10. Woertler K, Vestring T, Boettner F, Winkelmann W, Heindel W, Lindner N. Osteoid osteoma: CT-guided percutaneous radiofrequency ablation and follow-up in 47 patients. J Vasc Interv Radiol. 2001. 12:717–722.11. McGovern FJ, Wood BJ, Goldberg SN, Mueller PR. Radiofrequency ablation of renal cell carcinoma via image guided needle electrodes. J Urol. 1999. 161:599–600.12. Gervais DA, McGovern FJ, Arellano RS, McDougal WS, Mueller PR. Renal cell carcinoma: clinical experience and technical success with radio-frequency ablation of 42 tumors. Radiology. 2003. 226:417–424.13. Gervais DA, McGovern FJ, Wood BJ, Goldberg SN, McDougal WS, Mueller PR. Radio-frequency ablation of renal cell carcinoma: early clinical experience. Radiology. 2000. 217:665–672.14. Goldberg SN, Gazelle GS, Solbiati L, Rittman WJ, Mueller PR. Radiofrequency tissue ablation: increased lesion diameter with a perfusion electrode. Acad Radiol. 1996. 3:636–644.15. Goldberg SN, Hahn PF, Tanabe KK, Mueller PR, Schima W, Athanasoulis CA, et al. Percutaneous radiofrequency tissue ablation: does perfusion-mediated tissue cooling limit coagulation necrosis? J Vasc Interv Radiol. 1998. 9:101–111.16. Livraghi T, Goldberg SN, Lazzaroni S, Meloni F, Solbiati L, Gazelle GS. Small hepatocellular carcinoma: treatment with radio-frequency ablation versus ethanol injection. Radiology. 1999. 210:655–661.17. Farrell MA, Charboneau WJ, DiMarco DS, Chow GK, Zincke H, Callstrom MR, et al. Imaging-guided radiofrequency ablation of solid renal tumors. AJR Am J Roentgenol. 2003. 180:1509–1513.18. Schiller JD, Gervais DA, Mueller PR. Radiofrequency ablation of renal cell carcinoma. Abdom Imaging. 2005. 30:442–450.19. Park S, Anderson JK, Matsumoto ED, Lotan Y, Josephs S, Cadeddu JA. Radiofrequency ablation of renal tumors: intermediate-term results. J Endourol. 2006. 20:569–573.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spontaneous Regression of Pulmonary and Adrenal Metastases Following Percutaneous Radiofrequency Ablation of a Recurrent Renal Cell Carcinoma
- Chemoembolization combined with radiofrequency ablation is the best option for the local treatment of early hepatocellular carcinoma?
- Radiofrequency Thermal Ablation of Hepatocellular Carcinomas
- Microwave thermosphere versus radiofrequency ablation for hepatocellular carcinoma: Are we approaching the time to end the debate?
- Radiofrequency Ablation for Hepatocellular Carcinoma