Korean J Radiol.
2011 Feb;12(1):113-121. 10.3348/kjr.2011.12.1.113.
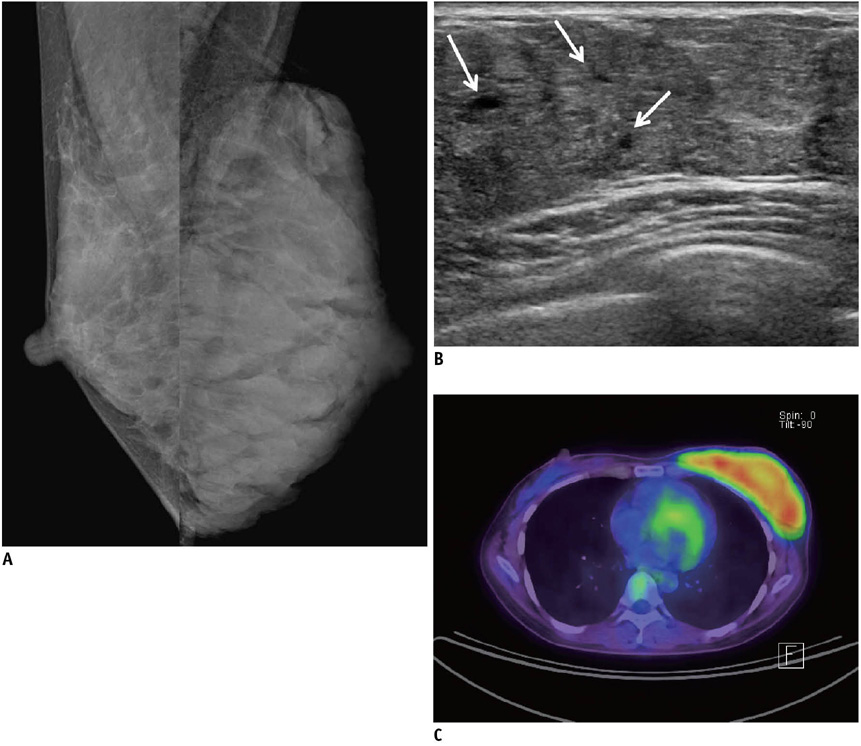
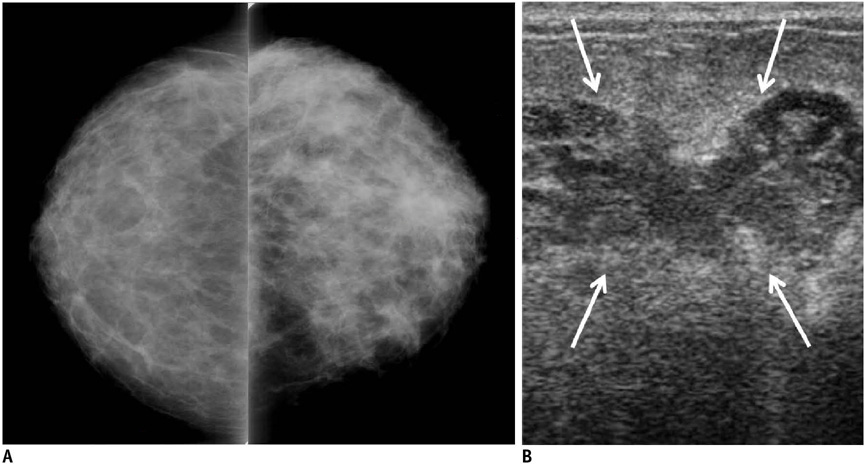
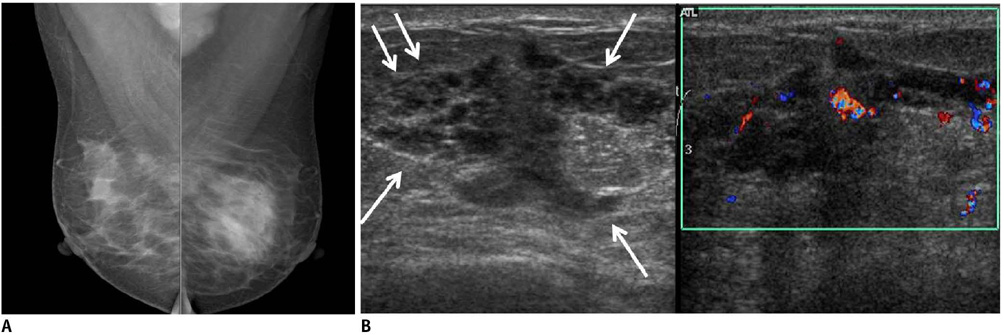
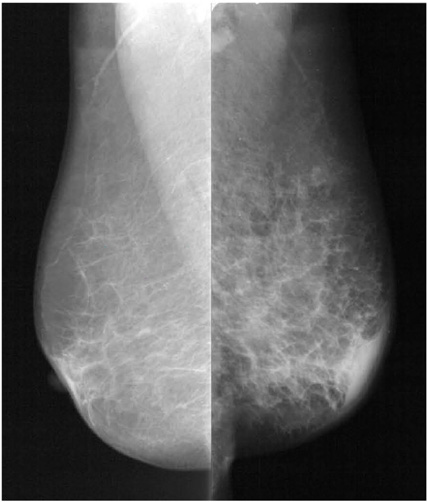
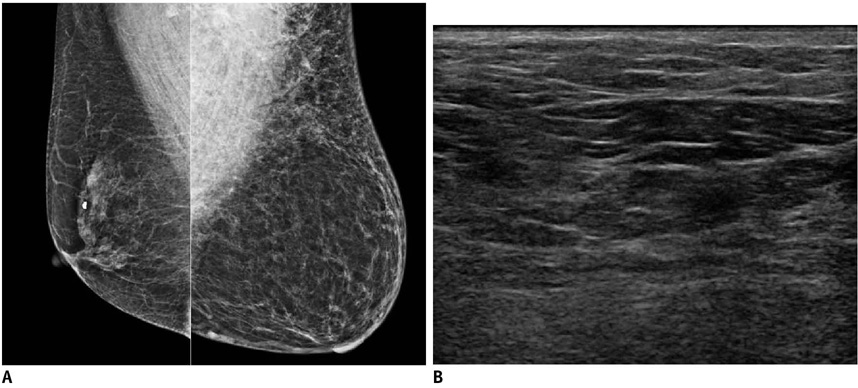
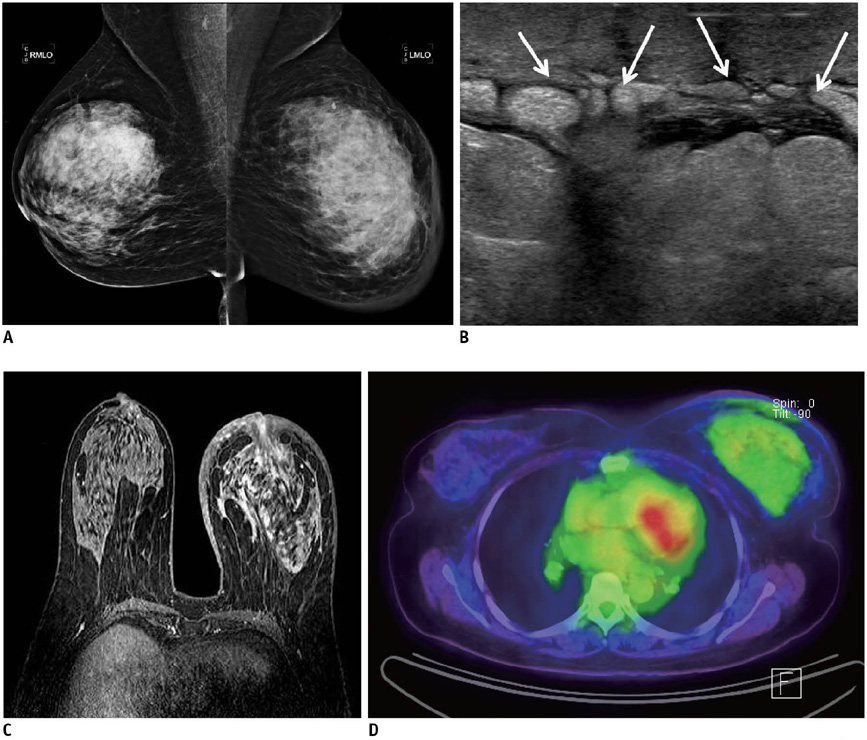
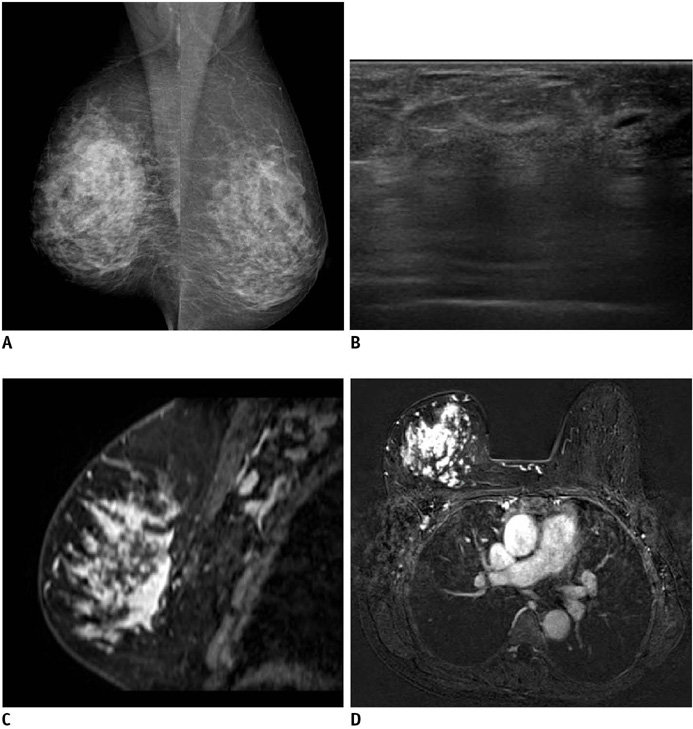
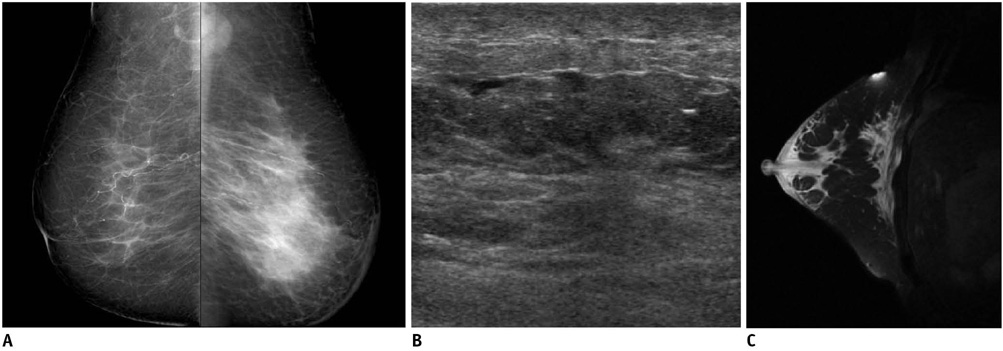
Diffuse Infiltrative Lesion of the Breast: Clinical and Radiologic Features
- Affiliations
-
- 1Department of Radiology, Seoul St. Mary's Hospital, Seoul 137-701, Korea. rad-ksh@catholic.ac.kr
- 2Department of Radiology, Ewha Womans University Mokdong Hospital, Seoul 158-701, Korea.
- 3Department of Radiology, St. Paul's Hospital, Seoul 130-709, Korea.
- 4Department of Radiology, Incheon St. Mary's Hospital, Incheon 403-720, Korea.
- 5Department of Radiology, Bucheon St. Mary's Hospital, Bucheon 420-717, Korea.
- 6Department of Radiology, Uijongbu St. Mary's Hospital, Uijongbu 480-130, Korea.
- KMID: 991689
- DOI: http://doi.org/10.3348/kjr.2011.12.1.113
Abstract
- The purpose of this paper is to show the clinical and radiologic features of a variety of diffuse, infiltrative breast lesions, as well to review the relevant literature. Radiologists must be familiar with the various conditions that can diffusely involve the breast, including normal physiologic changes, benign disease and malignant neoplasm.
MeSH Terms
Figure
Reference
-
1. Hogge JP, De Paredes ES, Magnant CM, Lage J. Imaging and management of breast masses during pregnancy and lactation. Breast J. 1999. 5:272–283.2. Hicks RJ, Binns D, Stabin MG. Pattern of uptake and excretion of (18) F-FDG in the lactating breast. J Nucl Med. 2001. 42:1238–1242.3. Yasuda S, Fujii H, Takahashi W, Takagi S, Ide M, Shohtsu A. Lactating breast exhibiting high F-18 FDG uptake. Clin Nucl Med. 1998. 23:767–768.4. Crowe DJ, Helvie MA, Wilson TE. Breast infection. Mammographic and sonographic findings with clinical correlation. Invest Radiol. 1995. 30:582–587.5. Ulitzsch D, Nyman MK, Carlson RA. Breast abscess in lactating women: US-guided treatment. Radiology. 2004. 232:904–909.6. Han BK, Choe YH, Park JM, Moon WK, Ko YH, Yang JH, et al. Granulomatous mastitis: mammographic and sonographic appearances. AJR Am J Roentgenol. 1999. 173:317–320.7. Fletcher A, Magrath IM, Riddell RH, Talbot IC. Granulomatous mastitis: a report of seven cases. J Clin Pathol. 1982. 35:941–945.8. Going JJ, Anderson TJ, Wilkinson S, Chetty U. Granulomatous lobular mastitis. J Clin Pathol. 1987. 40:535–540.9. Lee JH, Oh KK, Kim EK, Kwack KS, Jung WH, Lee HK. Radiologic and clinical features of idiopathic granulomatous lobular mastitis mimicking advanced breast cancer. Yonsei Med J. 2006. 47:78–84.10. Van Ongeval C, Schraepen T, Van Steen A, Baert AL, Moerman P. Idiopathic granulomatous mastitis. Eur Radiol. 1997. 7:1010–1012.11. Ibrahim RE, Sciotto CG, Weidner N. Pseudoangiomatous hyperplasia of mammary stroma. Some observations regarding its clinicopathologic spectrum. Cancer. 1989. 63:1154–1160.12. Ryu EM, Whang IY, Chang ED. Rapidly growing bilateral pseudoangiomatous stromal hyperplasia of the breast. Korean J Radiol. 2010. 11:355–358.13. Teh HS, Chiang SH, Leung JW, Tan SM, Mancer JF. Rapidly enlarging tumoral pseudoangiomatous stromal hyperplasia in a 15-year-old patient: distinguishing sonographic and magnetic resonance imaging findings and correlation with histologic findings. J Ultrasound Med. 2007. 26:1101–1106.14. Kwak JY, Kim EK, Chung SY, You JK, Oh KK, Lee YH, et al. Unilateral breast edema: spectrum of etiologies and imaging appearances. Yonsei Med J. 2005. 46:1–7.15. Toh CK, Leong SS, Thng CH, Tan EH. Unilateral breast edema in two patients with malignant pleural effusion. Tumori. 2004. 90:501–503.16. Rosen PP. Vascular tumors of the breast. V. Nonparenchymal hemangiomas of mammary subcutaneous tissues. Am J Surg Pathol. 1985. 9:723–729.17. Rosen PP. Vascular tumors of the breast. III. Angiomatosis. Am J Surg Pathol. 1985. 9:652–658.18. Siewert B, Jacobs T, Baum JK. Sonographic evaluation of subcutaneous hemangioma of the breast. AJR Am J Roentgenol. 2002. 178:1025–1027.19. Mesurolle B, Sygal V, Lalonde L, Lisbona A, Dufresne MP, Gagnon JH, et al. Sonographic and mammographic appearances of breast hemangioma. AJR Am J Roentgenol. 2008. 191:W17–W22.20. Dershaw DD, Moore MP, Liberman L, Deutch BM. Inflammatory breast carcinoma: mammographic findings. Radiology. 1994. 190:831–834.21. Ellis DL, Teitelbaum SL. Inflammatory carcinoma of the breast. A pathologic definition. Cancer. 1974. 33:1045–1047.22. Baslaim MM, Bakheet SM, Bakheet R, Ezzat A, El-Foudeh M, Tulbah A. 18-Fluorodeoxyglucose-positron emission tomography in inflammatory breast cancer. World J Surg. 2003. 27:1099–1104.23. Dixon JM, Anderson TJ, Page DL, Lee D, Duffy SW. Infiltrating lobular carcinoma of the breast. Histopathology. 1982. 6:149–161.24. Krecke KN, Gisvold JJ. Invasive lobular carcinoma of the breast: mammographic findings and extent of disease at diagnosis in 184 patients. AJR Am J Roentgenol. 1993. 161:957–960.25. Butler RS, Venta LA, Wiley EL, Ellis RL, Dempsey PJ, Rubin E. Sonographic evaluation of infiltrating lobular carcinoma. AJR Am J Roentgenol. 1999. 172:325–330.26. Vizcaíno I, Torregrosa A, Higueras V, Morote V, Cremades A, Torres V, et al. Metastasis to the breast from extramammary malignancies: a report of four cases and a review of literature. Eur Radiol. 2001. 11:1659–1665.27. Chung SY, Oh KK. Imaging findings of metastatic disease to the breast. Yonsei Med J. 2001. 42:497–502.28. Lee SH, Park JM, Kook SH, Han BK, Moon WK. Metastatic tumors to the breast: mammographic and ultrasonographic findings. J Ultrasound Med. 2000. 19:257–262.29. Arora R, Robinson WA. Breast metastases from malignant melanoma. J Surg Oncol. 1992. 50:27–29.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary Systemic Amyloidosis Presenting as Swollen Dense Breast: A Case Report
- Infiltrative invasion of the diaphragm: an uncommon manifestation of recurrent hepatocellular carcinoma
- DILD (diffuse infiltrative lung disease); Radiologic Diagnostic Approach According to High-Resolution CT Pattern
- Ultrasonographic Findings of Apocrine Lesions Arising from the Breast
- Ultrasonographic and Mammographic Findings of Gynecomastia