Korean J Radiol.
2010 Jun;11(3):333-345. 10.3348/kjr.2010.11.3.333.
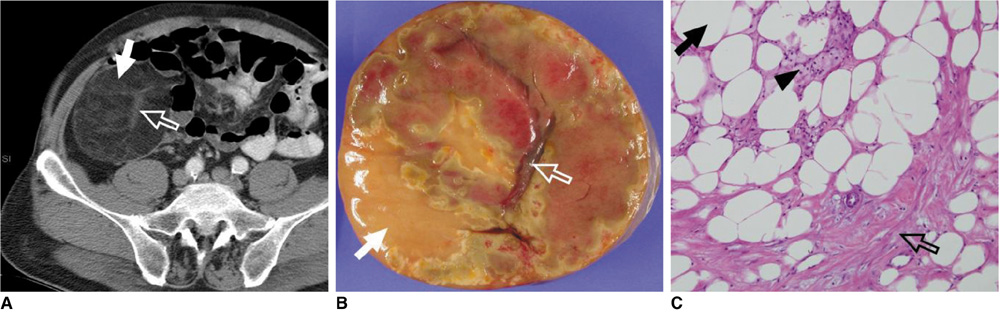
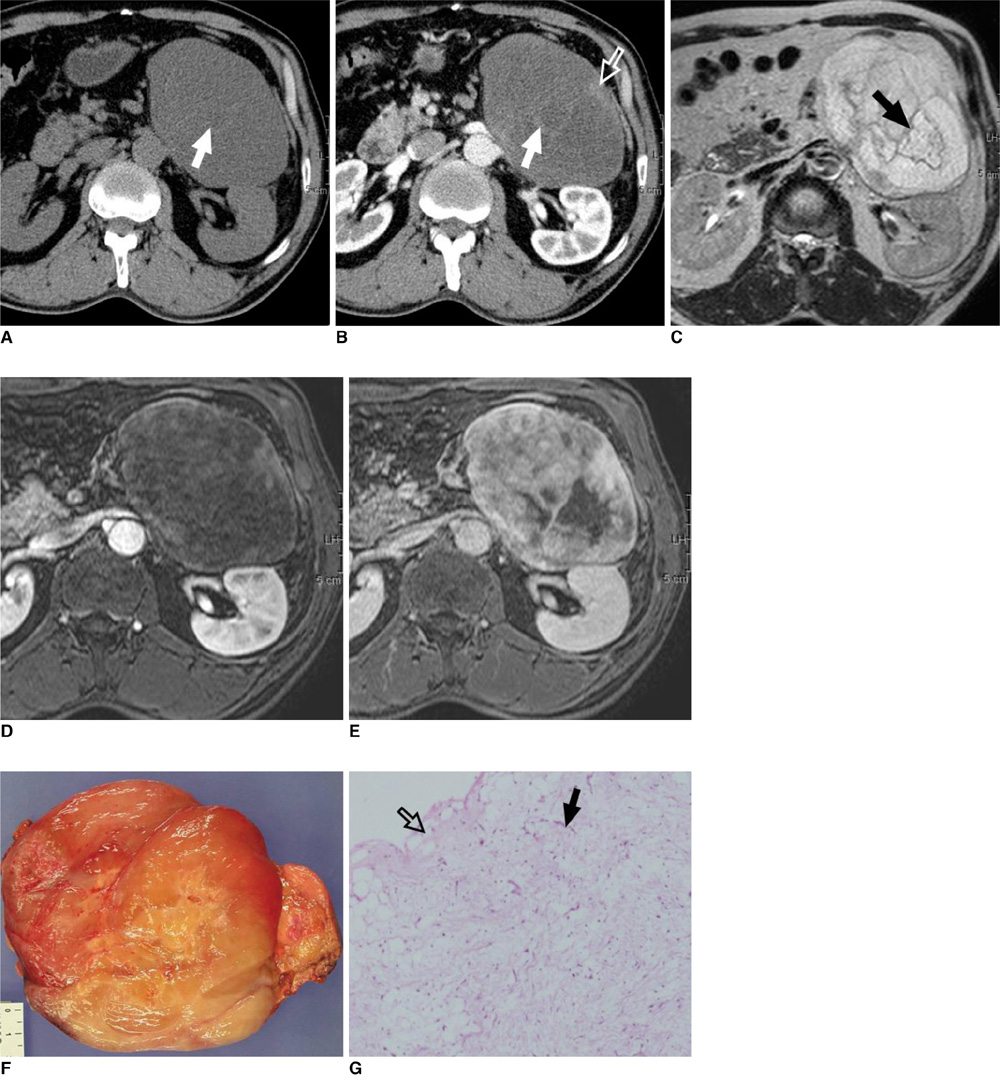
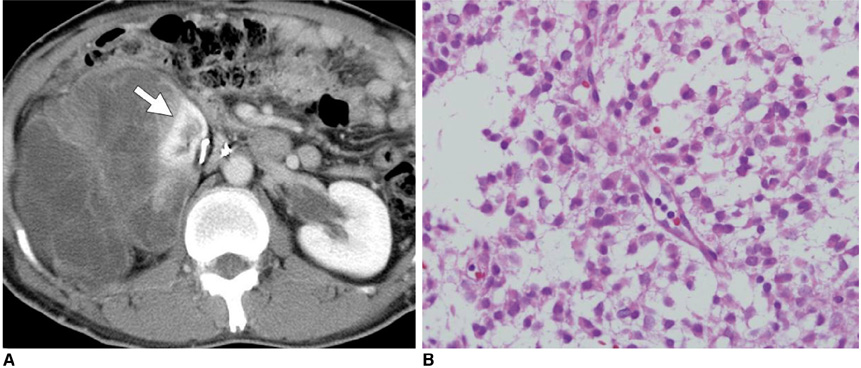
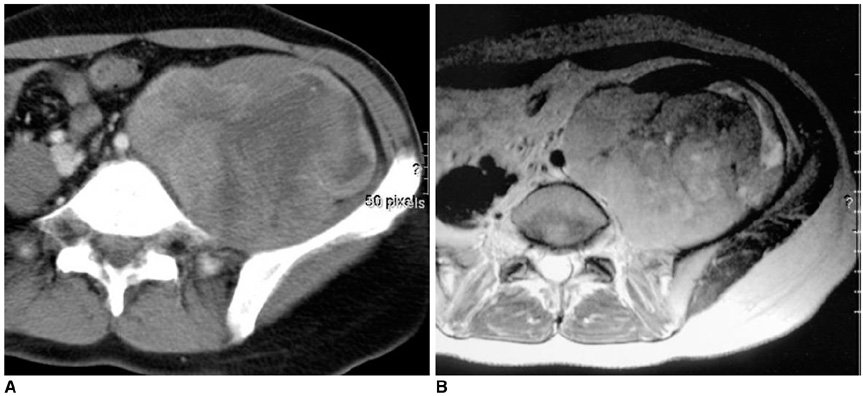
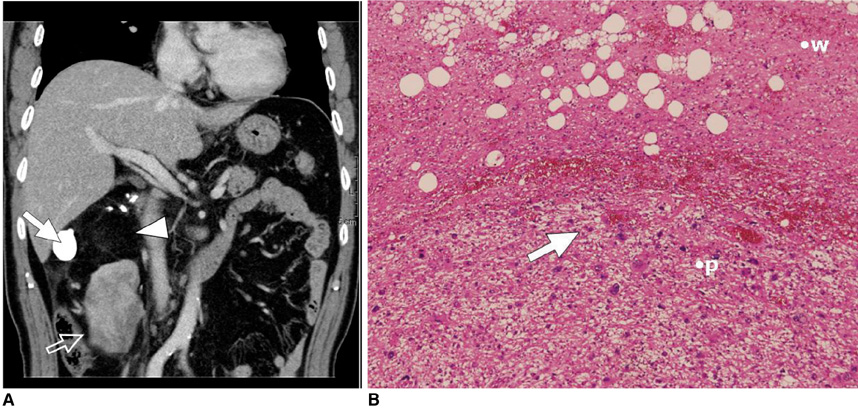
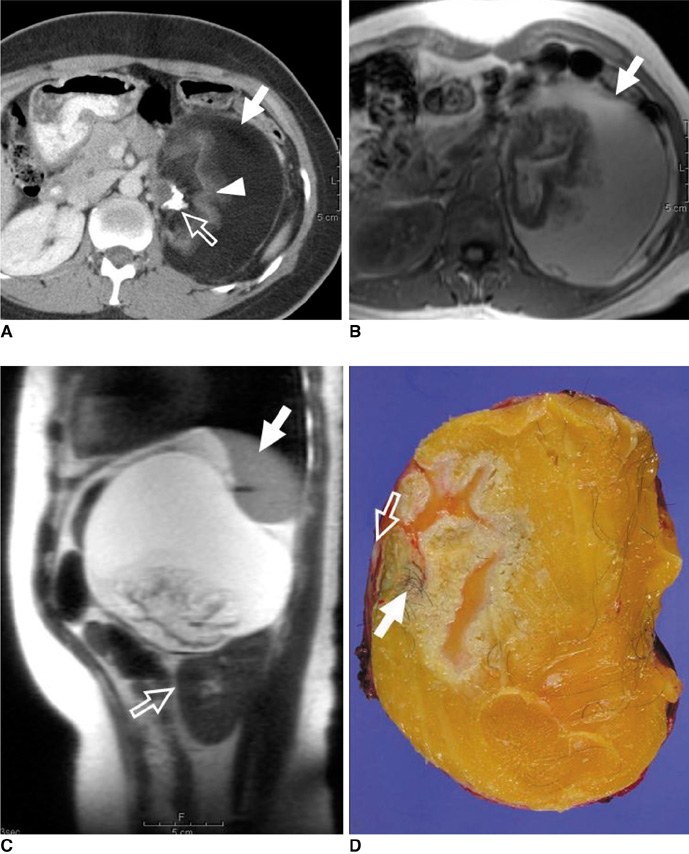
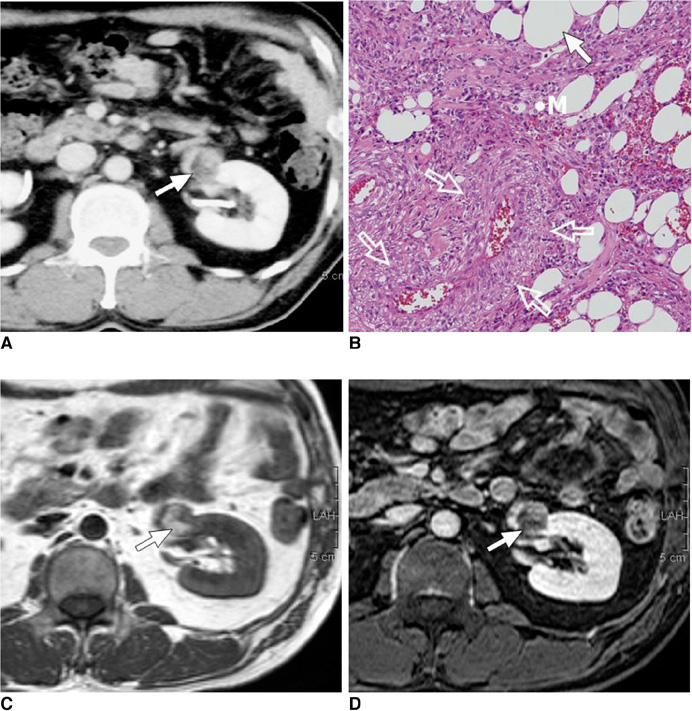
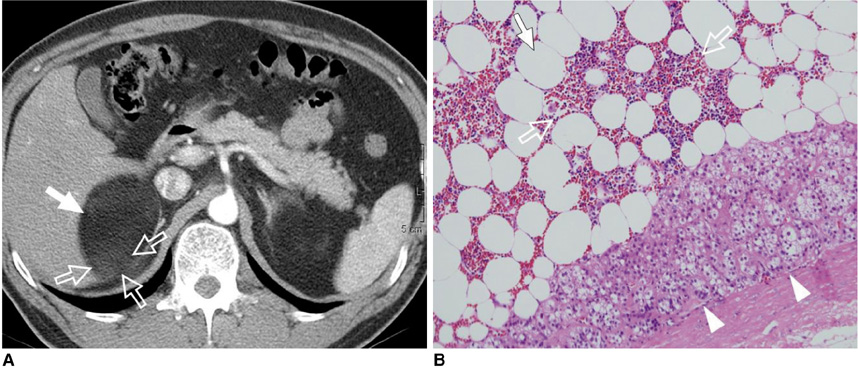
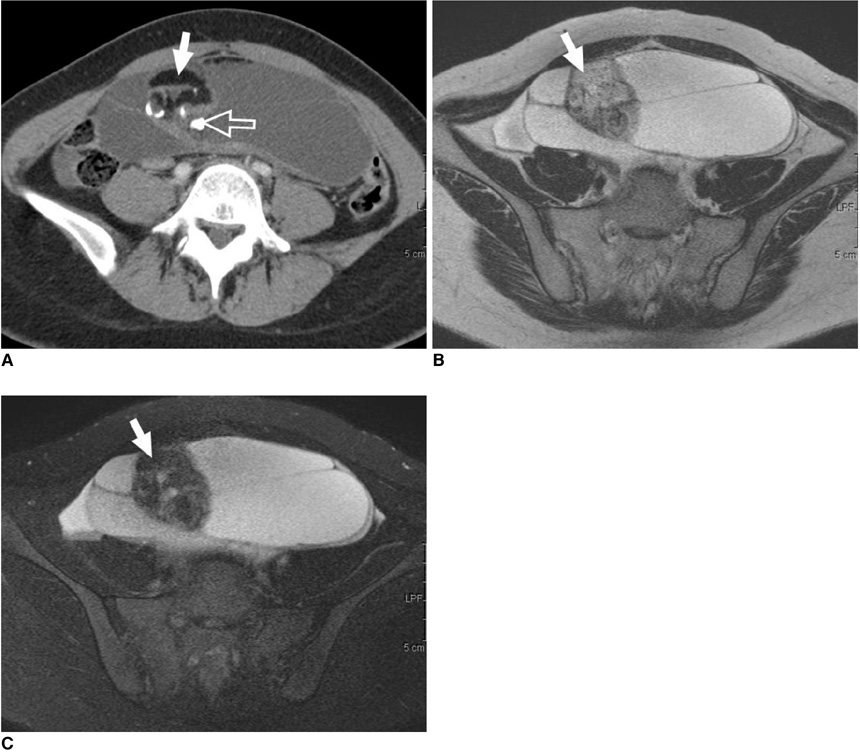
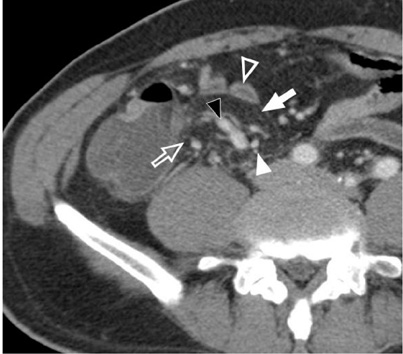
The Differential Imaging Features of Fat-Containing Tumors in the Peritoneal Cavity and Retroperitoneum: the Radiologic-Pathologic Correlation
- Affiliations
-
- 1Department of Radiology, Severance Hospital, Yonsei University School of Medicine, Seoul 120-752, Korea. kimnex@yuhs.ac
- 2Department of Pathology, Severance Hospital, Yonsei University School of Medicine, Seoul 120-752, Korea.
- KMID: 946274
- DOI: http://doi.org/10.3348/kjr.2010.11.3.333
Abstract
- There are a variety of fat-containing lesions that can arise in the intraperitoneal cavity and retroperitoneal space. Some of these fat-containing lesions, such as liposarcoma and retroperitoneal teratoma, have to be resected, although resection can be deferred for others, such as adrenal adenoma, myelolipoma, angiomyolipoma, ovarian teratoma, and lipoma, until the lesions become large or symptomatic. The third group tumors (i.e., mesenteric panniculitis and pseudolipoma of Glisson's capsule) require medical treatment or no treatment at all. Identifying factors such as whether the fat is macroscopic or microscopic within the lesion, the origin of the lesions, and the presence of combined calcification is important for narrowing the differential diagnosis. The development and wide-spread use of modern imaging modalities make identification of these factors easier so narrowing the differential diagnosis is possible. At the same time, lesions that do not require immediate treatment are being incidentally found at an increasing rate with these same imaging techniques. Thus, the questions about the treatment methods have become increasingly important. Classifying lesions in terms of the necessity of performing surgical treatment can provide important information to clinicians, and this is the one of a radiologist's key responsibilities.
Keyword
MeSH Terms
-
Abdominal Fat/pathology/radiography
Adult
Aged
Diagnosis, Differential
Female
Humans
Magnetic Resonance Imaging/methods
Male
Middle Aged
Neoplasms, Adipose Tissue/*pathology/*radiography
Peritoneal Cavity/pathology/radiography
Peritoneal Diseases/pathology/radiography
Peritoneal Neoplasms/*pathology/*radiography
Retroperitoneal Neoplasms/*pathology/*radiography
Retroperitoneal Space/pathology/radiography
Tomography, Spiral Computed/methods
Young Adult
Figure
Cited by 1 articles
-
The Magnetic Resonance (MR) Imaging Features of Myxoid Liposarcoma Arising from the Mesentery: a Case Report
Taehoon Ahn, Young Hwan Lee, Guy Mok Lee, Youe Ree Kim, Kwon-Ha Yoon
Investig Magn Reson Imaging. 2017;21(4):252-258. doi: 10.13104/imri.2017.21.4.252.
Reference
-
1. Prasad SR, Wang H, Rosas H, Menias CO, Narra VR, Middleton WD, et al. Fat-containing lesions of the liver: radiologic-pathologic correlation. Radiographics. 2005. 25:321–331.2. Pereira JM, Sirlin CB, Pinto PS, Casola G. CT and MR imaging of extrahepatic fatty masses of the abdomen and pelvis: techniques, diagnosis, differential diagnosis, and pitfalls. Radiographics. 2005. 25:69–85.3. Israel GM, Bosniak MA, Slywotzky CM, Rosen RJ. CT differentiation of large exophytic renal angiomyolipomas and perirenal liposarcomas. AJR Am J Roentgenol. 2002. 179:769–773.4. Singer S, Antonescu CR, Riedel E, Brennan MF. Histologic subtype and margin of resection predict pattern of recurrence and survival for retroperitoneal liposarcoma. Ann Surg. 2003. 238:358–370.5. Weiss SW. Weiss SW, Brooks JSJ, editors. Lipomatous tumors. Soft tissue tumors. 1996. Baltimore: Williams & Wilkins;207–251.6. Kim T, Murakami T, Oi H, Tsuda K, Matsushita M, Tomoda K, et al. CT and MR imaging of abdominal liposarcoma. AJR Am J Roentgenol. 1996. 166:829–833.7. Kawano R, Nishie A, Yoshimitsu K, Irie H, Tajima T, Hirakawa M, et al. Retroperitoneal well-differentiated inflammatory liposarcoma: a diagnostic dilemma. Radiat Med. 2008. 26:450–453.8. Dei Tos AP. Liposarcoma: new entities and evolving concepts. Ann Diagn Pathol. 2000. 4:252–266.9. Song T, Shen J, Liang BL, Mai WW, Li Y, Guo HC. Retroperitoneal liposarcoma: MR characteristics and pathological correlative analysis. Abdom Imaging. 2007. 32:668–674.10. Tateishi U, Hasegawa T, Beppu Y, Satake M, Moriyama N. Primary dedifferentiated liposarcoma of the retroperitoneum. Prognostic significance of computed tomography and magnetic resonance imaging features. J Comput Assist Tomogr. 2003. 27:799–804.11. Gatcombe HG, Assikis V, Kooby D, Johnstone PA. Primary retroperitoneal teratomas: a review of the literature. J Surg Oncol. 2004. 86:107–113.12. Taori K, Rathod J, Deshmukh A, Sheorain VS, Jawale R, Sanyal R, et al. Primary extragonadal retroperitoneal teratoma in an adult. Br J Radiol. 2006. 79:E120–E122.13. Davidson AJ, Hartman DS, Goldman SM. Mature teratoma of the retroperitoneum: radiologic, pathologic, and clinical correlation. Radiology. 1989. 172:421–425.14. Kurosaki Y, Tanaka YO, Itai Y. Well-differentiated liposarcoma of the retroperitoneum with a fat-fluid level: US, CT, and MR appearance. Eur Radiol. 1998. 8:474–475.15. Commons RR, Callaway CP. Adenomas of the adrenal cortex. Arch Med Interna. 1948. 81:37–41.16. Korobkin M, Giordano TJ, Brodeur FJ, Francis IR, Siegelman ES, Quint LE, et al. Adrenal adenomas: relationship between histologic lipid and CT and MR findings. Radiology. 1996. 200:743–747.17. L'Hostis H, Deminiere C, Ferriere JM, Coindre JM. Renal angiomyolipoma: a clinicopathologic, immunohistochemical, and follow-up study of 46 cases. Am J Surg Pathol. 1999. 23:1011–1020.18. Hajdu SI, Foote FW Jr. Angiomyolipoma of the kidney: report of 27 cases and review of the literature. J Urol. 1969. 102:396–401.19. Israel GM, Hindman N, Hecht E, Krinsky G. The use of opposed-phase chemical shift MRI in the diagnosis of renal angiomyolipomas. AJR Am J Roentgenol. 2005. 184:1868–1872.20. Wagner BJ, Wong-You-Cheong JJ, Davis CJ Jr. Adult renal hamartomas. Radiographics. 1997. 17:155–169.21. Schuster TG, Ferguson MR, Baker DE, Schaldenbrand JD, Solomon MH. Papillary renal cell carcinoma containing fat without calcification mimicking angiomyolipoma on CT. AJR Am J Roentgenol. 2004. 183:1402–1404.22. Kim JK, Park SY, Shon JH, Cho KS. Angiomyolipoma with minimal fat: differentiation from renal cell carcinoma at biphasic helical CT. Radiology. 2004. 230:677–684.23. Plaut A. Myelolipoma in the adrenal cortex; myeloadipose structures. Am J Pathol. 1958. 34:487–515.24. Kenney PJ, Wagner BJ, Rao P, Heffess CS. Myelolipoma: CT and pathologic features. Radiology. 1998. 208:87–95.25. Musante F, Derchi LE, Zappasodi F, Bazzocchi M, Riviezzo GC, Banderali A, et al. Myelolipoma of the adrenal gland: sonographic and CT features. AJR Am J Roentgenol. 1988. 151:961–964.26. Meyer A, Behrend M. Presentation and therapy of myelolipoma. Int J Urol. 2005. 12:239–243.27. Kumar M, Duerinckx AJ. Bilateral extraadrenal perirenal myelolipomas: an imaging challenge. AJR Am J Roentgenol. 2004. 183:833–836.28. Outwater EK, Siegelman ES, Hunt JL. Ovarian teratomas: tumor types and imaging characteristics. Radiographics. 2001. 21:475–490.29. Marina NM, Cushing B, Giller R, Cohen L, Lauer SJ, Ablin A, et al. Complete surgical excision is effective treatment for children with immature teratomas with or without malignant elements: A Pediatric Oncology Group/Children's Cancer Group Intergroup Study. J Clin Oncol. 1999. 17:2137–2143.30. Caspi B, Appelman Z, Rabinerson D, Zalel Y, Tulandi T, Shoham Z. The growth pattern of ovarian dermoid cysts: a prospective study in premenopausal and postmenopausal women. Fertil Steril. 1997. 68:501–505.31. Ayhan A, Bukulmez O, Genc C, Karamursel BS, Ayhan A. Mature cystic teratomas of the ovary: case series from one institution over 34 years. Eur J Obstet Gynecol Reprod Biol. 2000. 88:153–157.32. Daskalogiannaki M, Voloudaki A, Prassopoulos P, Magkanas E, Stefanaki K, Apostolaki E, et al. CT evaluation of mesenteric panniculitis: prevalence and associated diseases. AJR Am J Roentgenol. 2000. 174:427–431.33. Kikiros CS, Edis AJ. Mesenteric panniculitis resulting in bowel obstruction: response to steroids. Aust N Z J Surg. 1989. 59:287–290.34. Popkharitov AI, Chomov GN. Mesenteric panniculitis of the sigmoid colon: a case report and review of the literature. J Med Case Reports. 2007. 1:108.35. Quinn AM, Guzman-Hartman G. Pseudolipoma of Glisson capsule. Arch Pathol Lab Med. 2003. 127:503–504.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mesenchymal Tumors of the Breast: Imaging and the Histopathologic Correlation
- Radiologic-Pathologic Correlation of Unusual Lingual Masses:Part II: Benign and Malignant Tumors
- The peritoneal mesothelioma: 4 cases report
- Myxoid Solitary Fibrous Tumor of the Retroperitoneum: MRI Findings with the Pathologic Correlation
- Magnetic Resonance Imaging Features That Permit Differential Diagnosis of Chest Wall Liposarcoma Mimicking Lipoma in Men