Ann Hepatobiliary Pancreat Surg.
2025 May;29(2):121-126. 10.14701/ahbps.24-151.
Parenchymal-sparing non-anatomic resection vs. classic anatomic resection in colorectal cancer liver metastases
- Affiliations
-
- 1Department of Surgery, Inje University Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea
- KMID: 2568260
- DOI: http://doi.org/10.14701/ahbps.24-151
Abstract
- Backgrounds/Aims
Although anatomical liver resection is considered more effective in preventing complications and recurrence in hepatocellular carcinoma, its efficacy has yet to be clearly defined in colorectal cancer liver metastasis (CLM).
Methods
From January 2000 to December 2023, 145 patients underwent liver resections for CLM, divided into anatomic and non-anatomic resection cohorts. The dataset included demographic details, tumor size, number and distribution of metastases, neoadjuvant chemotherapy, primary tumor location and stage, type of liver surgery, transfusion rates, duration of hospital stay, postoperative complications, and completeness of resection.
Results
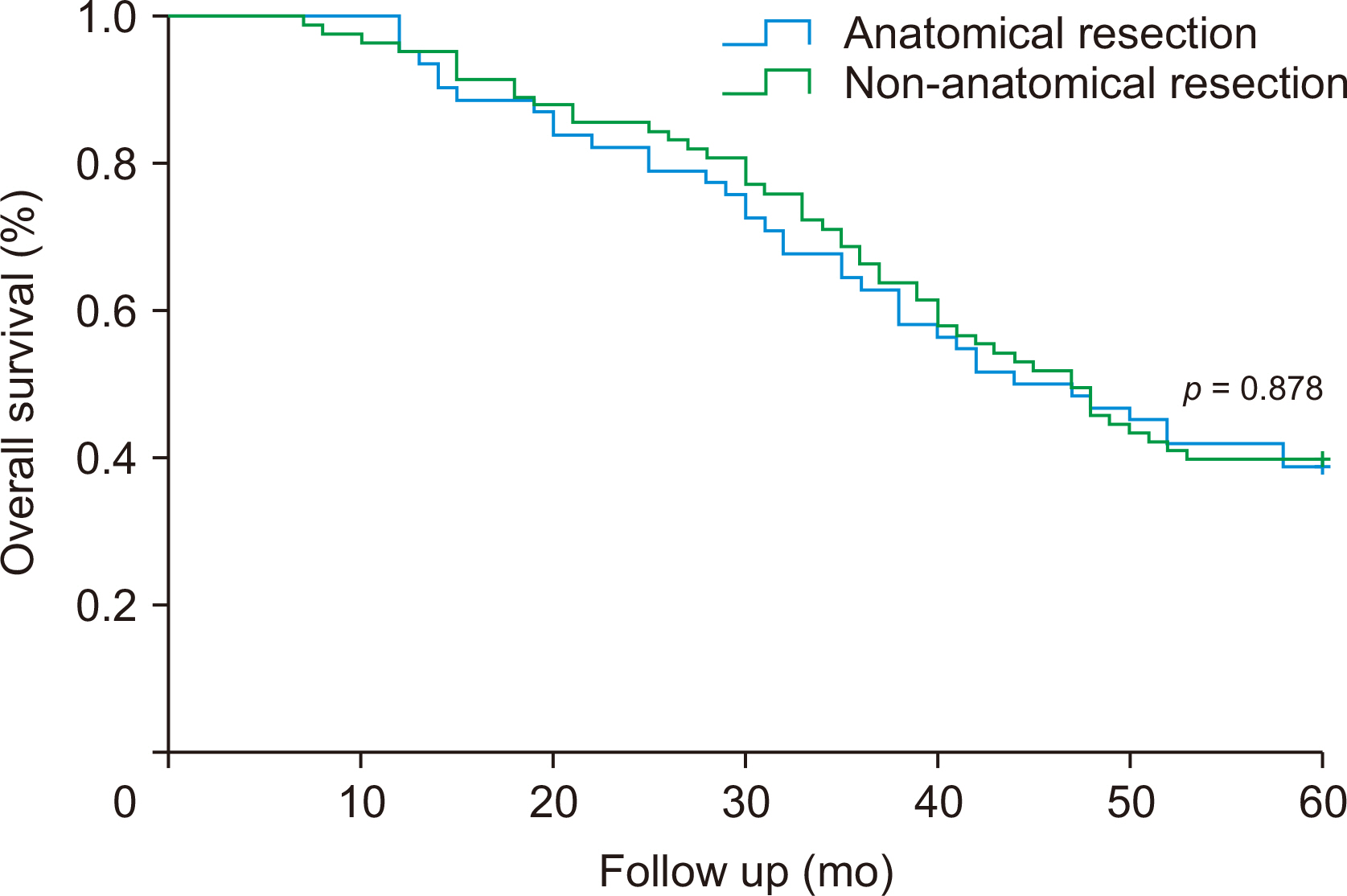
Of the 145 patients who underwent liver resections for metastases from colorectal cancer, 62 were in the anatomic group and 83 were in the non-anatomic group. The anatomic group had larger tumors (6.71 cm vs. 3.18 cm). Intraoperative transfusion rates were higher in the anatomic group (56.5% vs. 12.0%). Hospital stays, positive resection margin rates, and postoperative complication rates showed no significant differences. One surgery-related death occurred in the anatomic group. Disease-free and overall survival rates were comparable between groups.
Conclusions
Anatomic liver resection did not demonstrate a reduction in recurrence or an improvement in survival rates compared to non-anatomic resection. As such, anatomical resection does not offer a survival advantage over non-anatomical resection. Consequently, surgical method selection should prioritize patient safety, preservation of residual liver parenchyma, and tumor-specific factors.
Keyword
Figure
Reference
-
References
1. DeMatteo RP, Palese C, Jarnagin WR, Sun RL, Blumgart LH, Fong Y. 2000; Anatomic segmental hepatic resection is superior to wedge resection as an oncologic operation for colorectal liver metastases. J Gastrointest Surg. 4:178–184. DOI: 10.1016/S1091-255X(00)80054-2. PMID: 10675241.
Article2. Adam R, Delvart V, Pascal G, Valeanu A, Castaing D, Azoulay D, et al. 2004; Rescue surgery for unresectable colorectal liver metastases downstaged by chemotherapy: a model to predict long-term survival. Ann Surg. 240:644–657. discussion 657–658. DOI: 10.1097/01.sla.0000141198.92114.f6. PMID: 15383792. PMCID: PMC1356466.3. Tanaka K, Adam R, Shimada H, Azoulay D, Lévi F, Bismuth H. 2003; Role of neoadjuvant chemotherapy in the treatment of multiple colorectal metastases to the liver. Br J Surg. 90:963–969. DOI: 10.1002/bjs.4160. PMID: 12905549.
Article4. Bismuth H, Adam R, Lévi F, Farabos C, Waechter F, Castaing D, et al. 1996; Resection of nonresectable liver metastases from colorectal cancer after neoadjuvant chemotherapy. Ann Surg. 224:509–520. discussion 520–552. DOI: 10.1097/00000658-199610000-00009. PMID: 8857855. PMCID: PMC1235414.
Article5. Vauthey JN, Pawlik TM, Ribero D, Wu TT, Zorzi D, Hoff PM, et al. 2006; Chemotherapy regimen predicts steatohepatitis and an increase in 90-day mortality after surgery for hepatic colorectal metastases. J Clin Oncol. 24:2065–2072. DOI: 10.1200/JCO.2005.05.3074. PMID: 16648507.
Article6. Gold JS, Are C, Kornprat P, Jarnagin WR, Gönen M, Fong Y, et al. 2008; Increased use of parenchymal-sparing surgery for bilateral liver metastases from colorectal cancer is associated with improved mortality without change in oncologic outcome: trends in treatment over time in 440 patients. Ann Surg. 247:109–117. DOI: 10.1097/SLA.0b013e3181557e47. PMID: 18156930.
Article7. Kokudo N, Tada K, Seki M, Ohta H, Azekura K, Ueno M, et al. 2001; Anatomical major resection versus nonanatomical limited resection for liver metastases from colorectal carcinoma. Am J Surg. 181:153–159. DOI: 10.1016/S0002-9610(00)00560-2. PMID: 11425058.
Article8. Sarpel U, Bonavia AS, Grucela A, Roayaie S, Schwartz ME, Labow DM. 2009; Does anatomic versus nonanatomic resection affect recurrence and survival in patients undergoing surgery for colorectal liver metastasis? Ann Surg Oncol. 16:379–384. DOI: 10.1245/s10434-008-0218-2. PMID: 19020941.
Article9. Lalmahomed ZS, Ayez N, van der Pool AE, Verheij J, IJzermans JN, Verhoef C. 2011; Anatomical versus nonanatomical resection of colorectal liver metastases: is there a difference in surgical and oncological outcome? World J Surg. 35:656–661. DOI: 10.1007/s00268-010-0890-9. PMID: 21161655. PMCID: PMC3032901.
Article10. Seow-En I, Koh YX, Zhao Y, Ang BH, Tan IE, Chok AY, et al. 2024; Predictive modeling algorithms for liver metastasis in colorectal cancer: a systematic review of the current literature. Ann Hepatobiliary Pancreat Surg. 28:14–24. DOI: 10.14701/ahbps.23-078. PMID: 38129965. PMCID: PMC10896689.
Article