J Liver Cancer.
2023 Mar;23(1):202-205. 10.17998/jlc.2023.01.27.
Parenchymal-sparing hepatectomy for multiple bilobar colorectal liver metastases in a Jehovah’s witness: a case report
- Affiliations
-
- 1University Surgical Unit, National Hospital of Sri Lanka, Colombo, Sri Lanka
- 2Department of Surgery, Faculty of Medicine, University of Colombo, Colombo, Sri Lanka
- 3Department of Anaesthesiology and Critical Care, Faculty of Medicine, University of Colombo, Colombo, Sri Lanka
- KMID: 2540832
- DOI: http://doi.org/10.17998/jlc.2023.01.27
Abstract
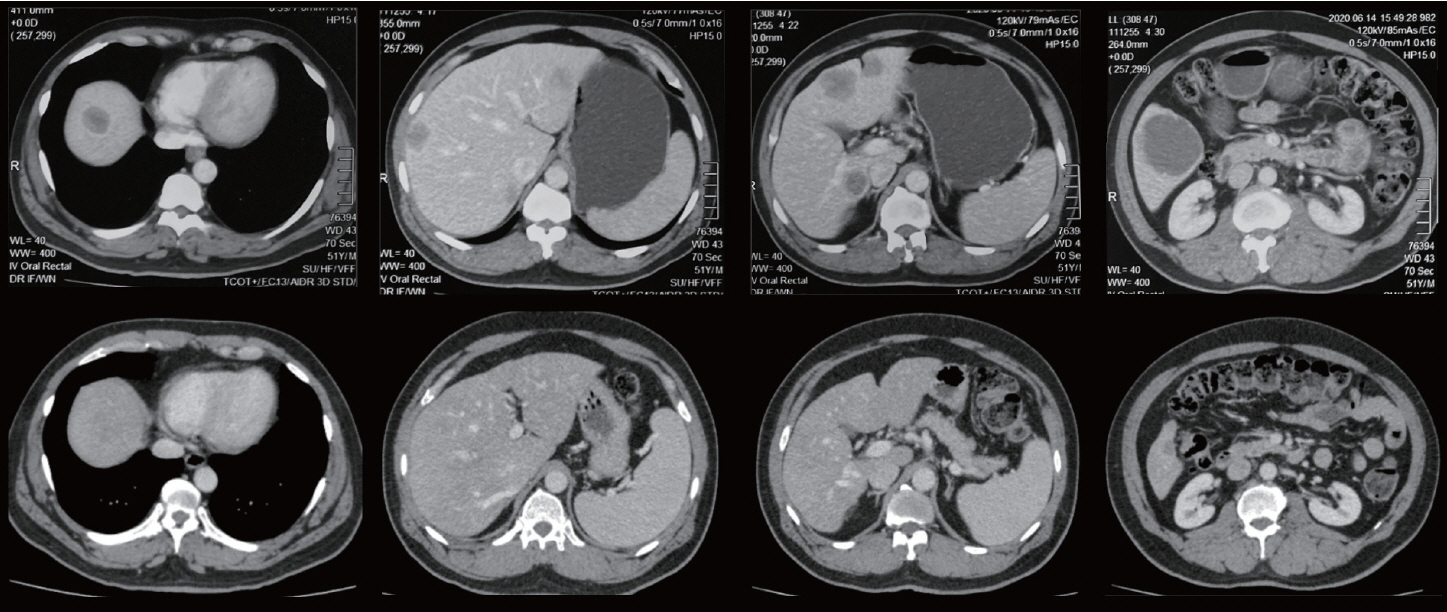
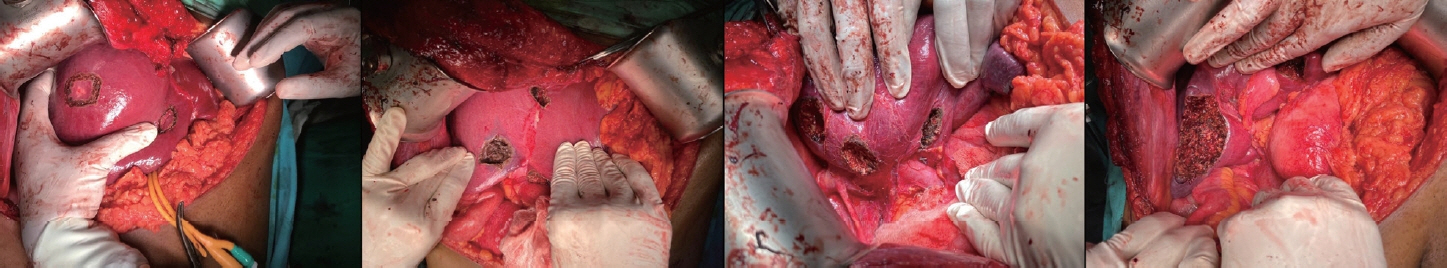
- Parenchymal-sparing hepatectomy (PSH), though technically challenging, is emerging as a choice of treatment for colorectal liver metastases (CRLM). PSH in Jehovah’s witness (JW) patients, for whom transfusion is not an option, involves complex surgical and medicolegal issues. A 52-year-old JW male with synchronous, multiple, bilobar liver metastases from a rectal adenocarcinoma was referred following neoadjuvant chemotherapy. At surgery, 10 metastatic deposits were observed and confirmed by intraoperative ultrasonography. Parenchymal-sparing non-anatomical resections were performed using a cavitron ultrasonic aspirator with the application of intermittent Pringle maneuvres. Histology confirmed multiple CRLMs with tumor-free resection margins. PSH is increasingly employed for CRLMs to preserve residual liver volume and minimize morbidity without compromising oncological outcomes. It is technically challenging, especially in the presence of bilobar, multi-segmental disease. This case illustrates the feasibility of performing complex hepatic surgery in special patient groups by meticulous planning and preparation involving multiple specialties and the patient.
Figure
Reference
-
References
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018; 68:394–424.
Article2. Moris D, Dimitroulis D, Vernadakis S, Papalampros A, Spartalis E, Petrou A, et al. Parenchymal-sparing hepatectomy as the new doctrine in the treatment of liver-metastatic colorectal disease: beyond oncological outcomes. Anticancer Res. 2017; 37:9–14.
Article3. Schadde E, Grunhagen DJ, Verhoef C, Krzywon L, Metrakos P. Limitations in resectability of colorectal liver metastases 2020 - a systematic approach for clinicians and patients. Semin Cancer Biol. 2021; 71:10–20.
Article4. Moris D, Ronnekleiv-Kelly S, Rahnemai-Azar AA, Felekouras E, Dillhoff M, Schmidt C, et al. Parenchymal-sparing versus anatomic liver resection for colorectal liver metastases: a systematic review. J Gastrointest Surg. 2017; 21:1076–1085.
Article5. Deng G, Li H, Jia GQ, Fang D, Tang YY, Xie J, et al. Parenchymalsparing versus extended hepatectomy for colorectal liver metastases: a systematic review and meta-analysis. Cancer Med. 2019; 8:6165–6175.
Article6. Lim C, Salloum C, Esposito F, Giakoustidis A, Moussallem T, Osseis M, et al. Safety and feasibility of elective liver resection in adult Jehovah’s witnesses: the Henri Mondor Hospital experience. HPB (Oxford). 2018; 20:823–828.
Article7. Margonis GA, Sasaki K, Andreatos N, Kim Y, Merath K, Wagner D, et al. KRAS mutation status dictates optimal surgical margin width in patients undergoing resection of colorectal liver Metastases. Ann Surg Oncol. 2017; 24:264–271.
Article8. Konstantinidis IT, Allen PJ, D’Angelica MI, Dematteo RP, Fischer ME, Grant F, et al. Pancreas and liver resection in jehovah’s witness patients: feasible and safe. J Am Coll Surg. 2013; 217:1101–1107.
Article9. Jarnagin WR, Gonen M, Maithel SK, Fong Y, D'Angelica MI, Dematteo RP, et al. A prospective randomized trial of acute normovolemic hemodilution compared to standard intraoperative management in patients undergoing major hepatic resection. Ann Surg. 2008; 248:360–369.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- More than 7-year survival of a patient following repeat hepatectomy for total 20 colon cancer liver metastases
- Anesthetic Experience during Liver Transplantation in a Pediatric Jehovah's Witness: A case report
- Anesthesia for a Jehovah's Witness Patient Experiencing Unexpected Perioperative Hemorrhage: A Case Report
- Anesthetic management of Jehovah's Witness patients
- Factors Affecting Survival Rate Following Hepatic Resection for Metastatic Colorectal Cancer