Ann Hepatobiliary Pancreat Surg.
2025 May;29(2):99-112. 10.14701/ahbps.24-236.
Feasibility and safety of robotic radical resection for hilar cholangiocarcinoma in highly selected patients: A systematic review and meta-analysis with meta-regression
- Affiliations
-
- 1Department of Hepatobiliary and Pancreatic Surgery, Morriston Hospital, Swansea, UK
- 2Department of Hepatobiliary and Pancreatic Surgery, Royal Stoke University Hospital, Stoke-on-Trent, UK
- 3Department of Hepatobiliary and Pancreatic Surgery, Manchester Royal Infirmary Hospital, Manchester, UK
- KMID: 2568251
- DOI: http://doi.org/10.14701/ahbps.24-236
Abstract
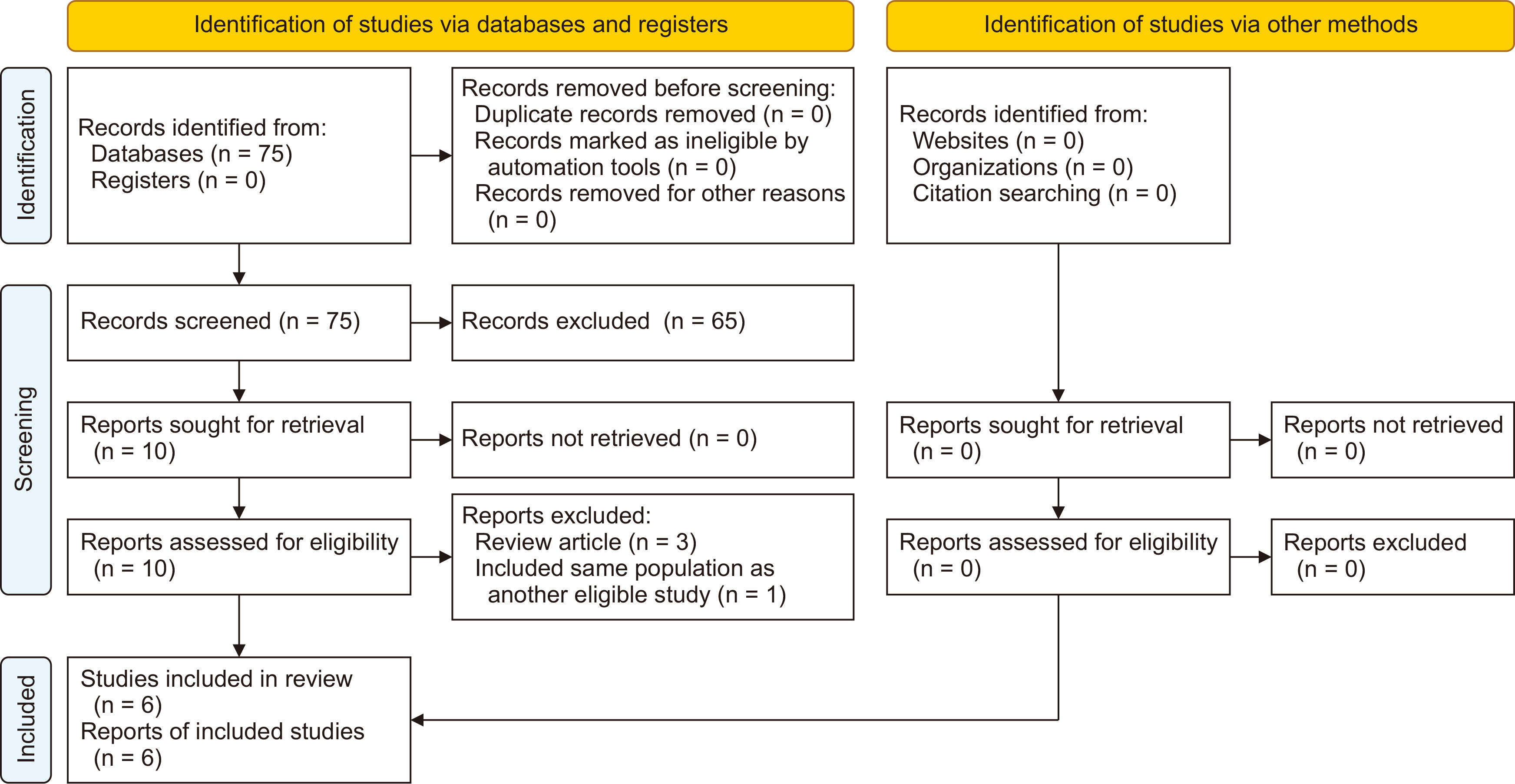
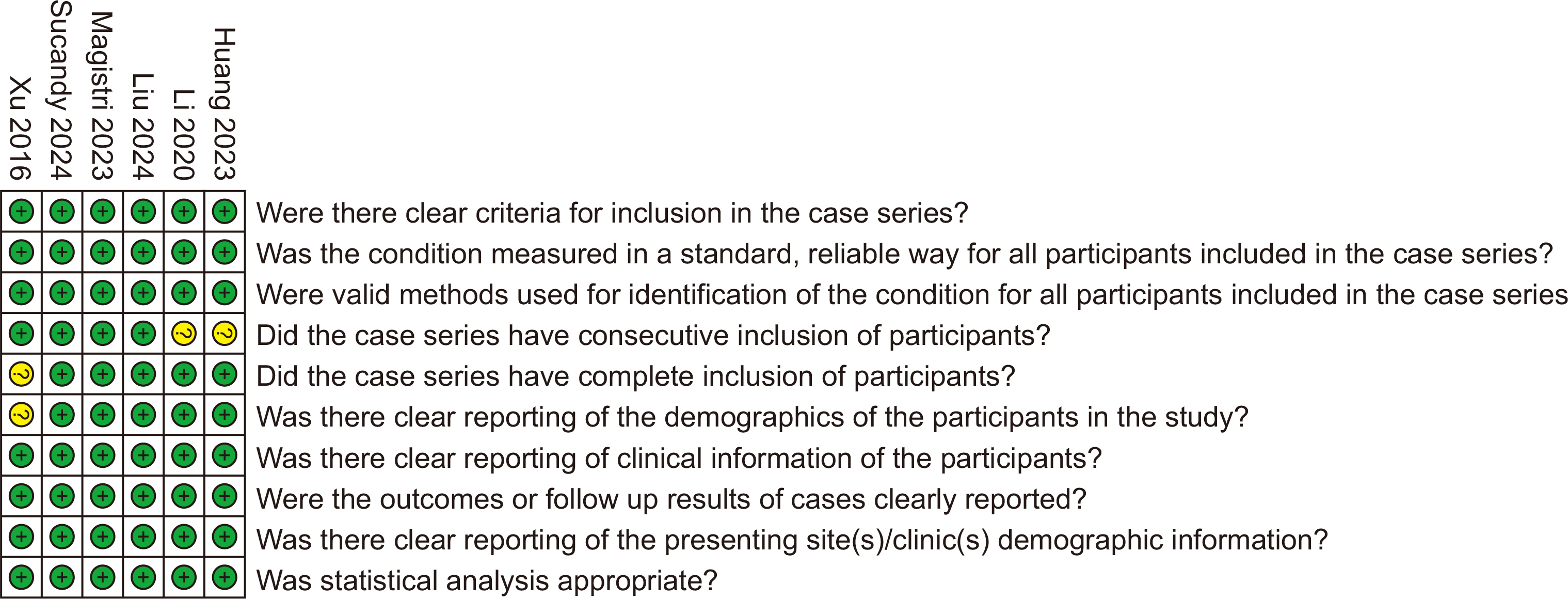
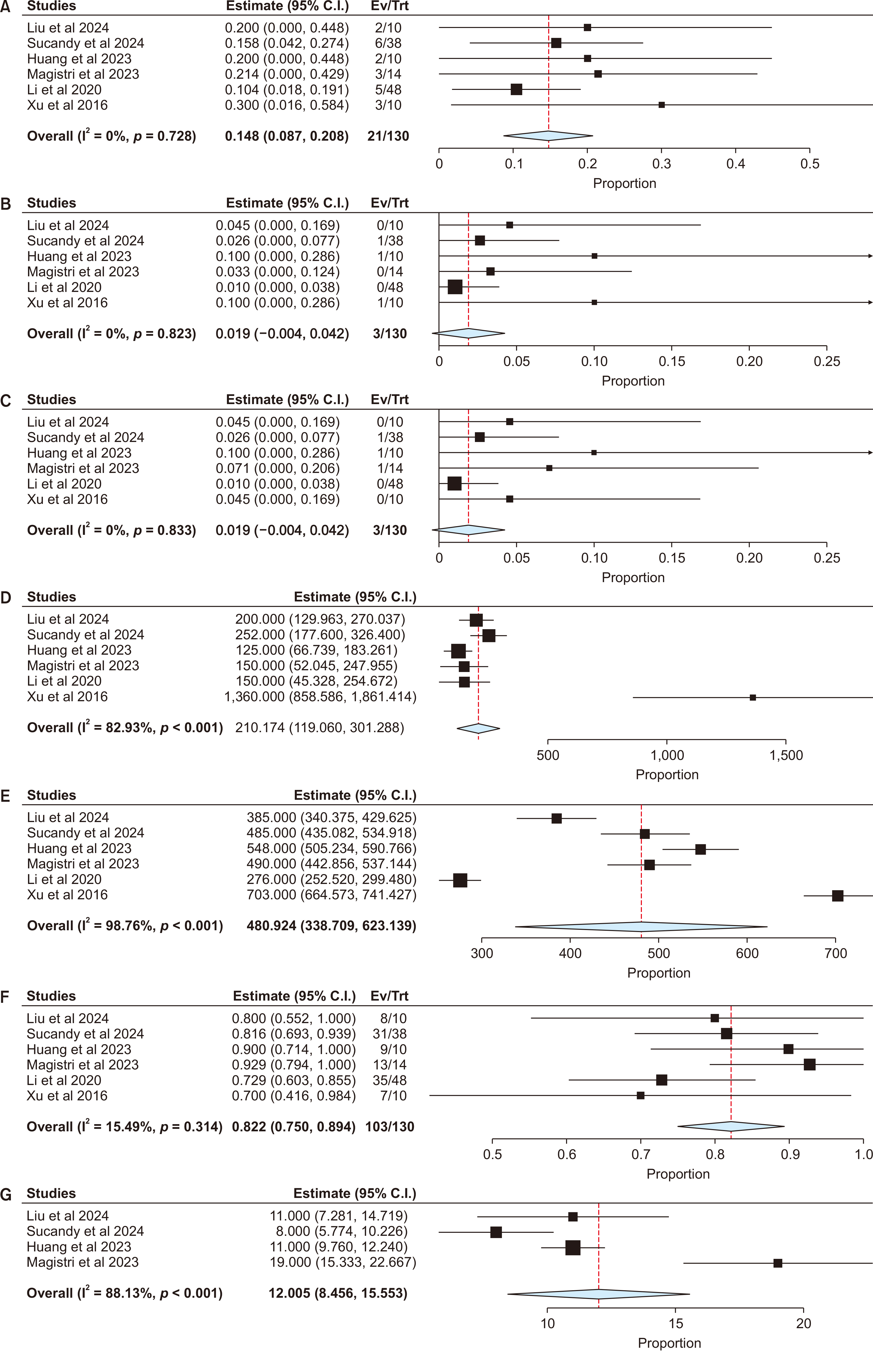
- To examine the feasibility and safety of robotic radical resection (RRR) for hilar cholangiocarcinoma (HCCA). A PRISMA-compliant meta-analysis with meta-regression was conducted, including studies reporting outcomes of RRR in patients with HCCA. Six studies comprising 295 patients were included. In highly selected patients (body mass index [BMI] < 25 kg/m” ; tumor size < 3 cm), RRR of HCCA proved safe and feasible (Clavien-Dindo ≥ III complications: 14.8% [95% confidence interval 8.7%–20.8%]; 30-day mortality: 1.9% [0%–4.2%]; conversion to open surgery: 1.9% [0%–4.2%]; intraoperative blood loss: 210 mL [119–301 mL]; operative time: 481 minutes [339–623 minutes]; R0 resection rate: 82.2% [75.0%–89.4%]; retrieved lymph nodes: 12 [9–16]). Younger age (p = 0.008), higher BMI (p = 0.009), larger tumors (p = 0.048), and performing liver resections (p = 0.017) increased blood loss. American Society of Anesthesiologists status ≥ III (p < 0.001) and Bismuth IV disease (p < 0.001) increased operative times. Preoperative biliary drainage (p = 0.027) enhanced R0 resection rates. RRR led to less bleeding (mean difference [MD]: –184 mL, p = 0.0005), longer operative times (MD: 162 minutes, p = 0.001), and improved R0 resection rates (odds ratio: 3.29, p = 0.006) compared with the open approach. Subject to selection bias and type 2 error, RRR for HCCA might be safe and feasible in highly selected patients (favorable BMI and tumor size). The findings should not be taken as definitive conclusions but may be used for hypothesis generation in subsequent trials.
Keyword
Figure
Reference
-
References
1. Jena SS, Mehta NN, Nundy S. 2023; Surgical management of hilar cholangiocarcinoma: Controversies and recommendations. Ann Hepatobiliary Pancreat Surg. 27:227–240. DOI: 10.14701/ahbps.23-028. PMID: 37408334. PMCID: PMC10472117.
Article2. Cipriani F, Ratti F, Fiorentini G, Reineke R, Aldrighetti L. 2021; Systematic review of perioperative and oncologic outcomes of minimally-invasive surgery for hilar cholangiocarcinoma. Updates Surg. 73:359–377. DOI: 10.1007/s13304-021-01006-6. PMID: 33615423.
Article3. Xiong Y, Jingdong L, Zhaohui T, Lau J. 2021; A consensus meeting on expert recommendations on operating specifications for laparoscopic radical resection of hilar cholangiocarcinoma. Front Surg. 8:731448. DOI: 10.3389/fsurg.2021.731448. PMID: 34888342. PMCID: PMC8651246.
Article4. Antoniou SA, Antoniou GA, Antoniou AI, Granderath FA. 2015; Past, present, and future of minimally invasive abdominal surgery. JSLS. 19:e2015.00052. DOI: 10.4293/JSLS.2015.00052. PMID: 26508823. PMCID: PMC4589904.
Article5. Berber E, Akyildiz HY, Aucejo F, Gunasekaran G, Chalikonda S, Fung J. 2010; Robotic versus laparoscopic resection of liver tumours. HPB (Oxford). 12:583–586. DOI: 10.1111/j.1477-2574.2010.00234.x. PMID: 20887327. PMCID: PMC2997665.
Article6. https://www.training.cochrane.org/handbook.7. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. 2021; The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 372:n71. DOI: 10.1136/bmj.n71. PMID: 33782057. PMCID: PMC8005924.8. Munn Z, Barker TH, Moola S, Tufanaru C, Stern C, McArthur A, et al. 2020; Methodological quality of case series studies: an introduction to the JBI critical appraisal tool. JBI Evid Synth. 18:2127–2133. DOI: 10.11124/JBISRIR-D-19-00099. PMID: 33038125.9. https://gdt.gradepro.org/app/handbook/handbook.html.10. Liu J, Dou C, Chen J, Lu Y, Liang L, Wei F, et al. 2024; Evaluation of the outcomes of biliary-enteric reconstruction in robotic radical resection of hilar cholangiocarcinoma: a single-center propensity score matching analysis. Sci Rep. 14:14836. DOI: 10.1038/s41598-024-65875-8. PMID: 38937559. PMCID: PMC11211424.
Article11. Sucandy I, Marques HP, Lippert T, Magistri P, Coelho JS, Ross SB, et al. 2024; Clinical outcomes of robotic resection for perihilar cholangiocarcinoma: a first, multicenter, trans-atlantic, expert-center, collaborative study. Ann Surg Oncol. 31:81–89. DOI: 10.1245/s10434-023-14307-4. PMID: 37718337.
Article12. Huang XT, Xie JZ, Cai JP, Chen W, Chen LH, Liang LJ, et al. 2023; Evaluation of the short-term outcomes of robotic-assisted radical resection for perihilar cholangiocarcinoma: a propensity-scored matching analysis. Gastroenterol Rep (Oxf). 11:goad018. DOI: 10.1093/gastro/goad018. PMID: 37051578. PMCID: PMC10085544.
Article13. Magistri P, Pang NQ, Guidetti C, Caracciolo D, Odorizzi R, Catellani B, et al. 2023; Robotic approach for perihilar cholangiocarcinoma: from Bismuth 1 to vascular resection. Eur J Surg Oncol. 49:107002. DOI: 10.1016/j.ejso.2023.107002. PMID: 37599146.
Article14. Li J, Tan X, Zhang X, Zhao G, Hu M, Zhao Z, et al. 2020; Robotic radical surgery for hilar cholangiocarcinoma: a single-centre case series. Int J Med Robot. 16:e2076. DOI: 10.1002/rcs.2076. PMID: 31925864.
Article15. Xu Y, Wang H, Ji W, Tang M, Li H, Leng J, et al. 2016; Robotic radical resection for hilar cholangiocarcinoma: perioperative and long-term outcomes of an initial series. Surg Endosc. 30:3060–3070. DOI: 10.1007/s00464-016-4925-7. PMID: 27194255.
Article16. Hu M, Xu D, Zhang Y, Li A, Li X, Huang J. 2024; Efficacy and safety of robotic surgery versus open surgery for hilar cholangiocarcinoma: a systematic review and meta-analysis. Int J Surg. 111:1301–1310. DOI: 10.1097/JS9.0000000000001952. PMID: 39037741. PMCID: PMC11745663.
Article17. Brolese A, Rigoni M, Pasquale A, Viel G, Brolese M, Ciarleglio FA. 2022; The role of robotic surgery for the treatment of hilar cholangiocarcinoma: a systematic review. Front Oncol. 12:1001838. DOI: 10.3389/fonc.2022.1001838. PMID: 36237328. PMCID: PMC9552766.
Article18. De Bellis M, Mastrosimini MG, Conci S, Pecori S, Campagnaro T, Castelli C, et al. 2022; The prognostic role of true radical resection in perihilar cholangiocarcinoma after improved evaluation of radial margin status. Cancers (Basel). 14:6126. DOI: 10.3390/cancers14246126. PMID: 36551610. PMCID: PMC9776927.
Article19. Hajibandeh S, Kotb A, Evans L, Sams E, Naguib A, Hajibandeh S, et al. 2023; Procedural outcomes of laparoscopic caudate lobe resection: a systematic review and meta-analysis. Ann Hepatobiliary Pancreat Surg. 27:6–19. DOI: 10.14701/ahbps.22-045. PMID: 36245071. PMCID: PMC9947369.
Article20. Jones T, Christodoulou M, Ross S, Pattilachan TM, Rosemurgy A, Sucandy I. 2025; Caudate lobe and posterosuperior segment hepatectomy using the robotic approach. Outcome analysis of liver resection in difficult locations. Am J Surg. 239:115996. DOI: 10.1016/j.amjsurg.2024.115996. PMID: 39393300.
Article