J Korean Med Sci.
2025 Apr;40(16):e44. 10.3346/jkms.2025.40.e44.
A Study on the Healthcare Workforce and Care for Acute Stroke: Results From the Survey of Hospitals Included in the National Acute Stroke Quality Assessment Program
- Affiliations
-
- 1Department of Neurosurgery, Hallym University Gangdong Sacred Heart Hospital, Seoul, Korea
- 2Department of Neurosurgery, Biomedical Research Institute, Pusan National University Hospital, School of Medicine, Pusan National University, Busan, Korea
- 3Department of Neurosurgery, Kyung Hee University Hospital at Gangdong, Kyung Hee University College of Medicine, Seoul, Korea
- 4Department of Neurosurgery, Inje University Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea
- 5Department of Neurosurgery, Chungnam National University Hospital, Chungnam National University School of Medicine, Daejeon, Korea
- 6Department of Neurosurgery, Institute of Wonkwang Medical Science, Wonkwang University School of Medicine, Iksan, Korea
- 7Department of Neurosurgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 8Department of Neurosurgery, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- 9Department of Neurosurgery, Bucheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 10Department of Neurosurgery, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 11Department of Neurosurgery, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea
- 12Department of Neurosurgery, Uijeongbu St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 13Department of Neurosurgery, Korea University Guro Hospital, Seoul, Korea
- 14Department of Neurosurgery, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 15Department of Neurosurgery, Soonchunhyang University Bucheon Hospital, Bucheon, Korea
- 16Department of Neurosurgery, Hallym University Sacred Heart Hospital, Anyang, Korea
- 17Department of Neurosurgery, Jeju National University Hospital, Jeju National University College of Medicine, Jeju, Korea
- 18Department of Neurosurgery, Incheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea
- 19Department of Neurosurgery, Yeungnam University Medical Center and Yeungnam University Medical School, Daegu, Korea
- 20Department of Neurosurgery, Chosun University Hospital, Gwangju, Korea
- 21Department of Neurosurgery, CHA Bundang Medical Center, CHA University College of Medicine, Seongnam, Korea
- KMID: 2568085
- DOI: http://doi.org/10.3346/jkms.2025.40.e44
Abstract
- Background
With growing elderly populations, management of patients with acute stroke is increasingly important. In South Korea, the Acute Stroke Quality Assessment Program (ASQAP) has contributed to improving the quality of stroke care and practice behavior in healthcare institutions. While the mortality of hemorrhagic stroke remains high, there are only a few assessment indices associated with hemorrhagic stroke. Considering the need to develop assessment indices to improve the actual quality of care in the field of acute stroke treatment, this study aims to investigate the current status of human resources and practices related to the treatment of patients with acute stroke through a nationwide survey.
Methods
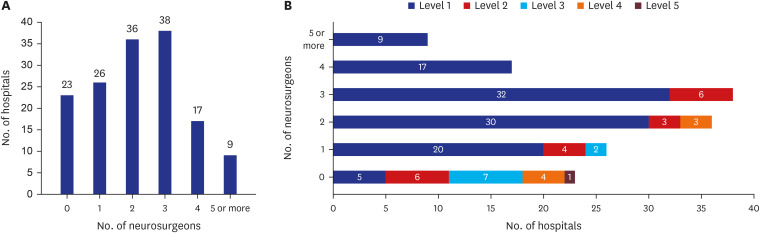
For the healthcare institutions included in the Ninth ASQAP of the Health Insurance Review and Assessment Service (HIRA), data from January 2022 to December 2022 were collected through a survey on the current status and practice of healthcare providers related to the treatment of patients with acute stroke. The questionnaire consisted of 19 items, including six items on healthcare providers involved in stroke care and 10 items on the care of patients with acute stroke.
Results
In the treatment of patients with hemorrhagic stroke among patients with acute stroke, neurosurgeons were the most common providers. The contribution of neurosurgeons in the treatment of ischemic stroke has also been found to be equivalent to that of neurologists. However, a number of institutions were found to be devoid of healthcare providers who perform definitive treatments, such as intra-arterial thrombectomy for patients with ischemic stroke or cerebral aneurysm clipping for subarachnoid hemorrhage. The intensity of the workload of healthcare providers involved in the care of patients with acute stroke, especially those involved in definitive treatment, was also found to be quite high.
Conclusion
Currently, there are almost no assessment indices specific to hemorrhagic stroke in the ASQAP for acute stroke. Furthermore, it does not reflect the reality of the healthcare providers and practices that provide definitive treatment for acute stroke. The findings of this study suggest the need for the development of appropriate assessment indices that reflect the realities of acute stroke care.
Keyword
Figure
Reference
-
1. Thayabaranathan T, Kim J, Cadilhac DA, Thrift AG, Donnan GA, Howard G, et al. Global stroke statistics 2022. Int J Stroke. 2022; 17(9):946–956. PMID: 35975986.2. Moon J, Seo Y, Lee HH, Lee H, Kaneko F, Shin S, et al. Incidence and case fatality of stroke in Korea, 2011–2020. Epidemiol Health. 2024; 46:e2024003. PMID: 38186243.3. Cheon S, Li CY, Jeng JS, Wang JD, Ku LE. The lifetime burden following stroke: long term impact of stroke on survival and quality of life. Int J Stroke. 2023; 18(7):795–803. PMID: 36912208.4. Lee YS, Lee HY, Leigh JH, Choi Y, Kim HK, Oh BM. The socioeconomic burden of acquired brain injury among the Korean patients over 20 years of age in 2015–2017: a prevalence-based approach. Brain Neurorehabil. 2021; 14(3):e24. PMID: 36741222.5. Zahuranec DB, Lisabeth LD, Sánchez BN, Smith MA, Brown DL, Garcia NM, et al. Intracerebral hemorrhage mortality is not changing despite declining incidence. Neurology. 2014; 82(24):2180–2186. PMID: 24838789.6. Nakaoku Y, Ogata S, Ren N, Tanaka T, Kurogi R, Nishimura K, et al. Ten-year national trends in in-hospital mortality and functional outcomes after intracerebral hemorrhage by age in Japan: J-ASPECT study. Eur Stroke J. 2024; 9(2):398–408. PMID: 38288694.7. Jolink WM, Klijn CJ, Brouwers PJ, Kappelle LJ, Vaartjes I. Time trends in incidence, case fatality, and mortality of intracerebral hemorrhage. Neurology. 2015; 85(15):1318–1324. PMID: 26377254.8. Lee KB, Lee JS, Lee JY, Kim JY, Jeong HY, Kim SE, et al. Quality of acute stroke care within emergency medical service system in Korea: proposal for severe emergency medical center. J Korean Neurol Assoc. 2023; 41(1):18–30.9. McKinney JS, Cheng JQ, Rybinnik I, Kostis JB. Myocardial Infarction Data Acquisition System (MIDAS 22) Study Group. Comprehensive stroke centers may be associated with improved survival in hemorrhagic stroke. J Am Heart Assoc. 2015; 4(5):e001448. PMID: 25950185.10. Kurogi R, Kada A, Ogasawara K, Kitazono T, Sakai N, Hashimoto Y, et al. Effects of case volume and comprehensive stroke center capabilities on patient outcomes of clipping and coiling for subarachnoid hemorrhage. J Neurosurg. 2020; 134(3):929–939. PMID: 32168489.11. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; 372(1):11–20. PMID: 25517348.12. Kim TG, Kwon O, Shin YS, Sung JH, Koh JS, Kim BT. Endovascular treatments performed collaboratively by the Society of Korean Endovascular Neurosurgeons Members: a nationwide multicenter survey. J Korean Neurosurg Soc. 2019; 62(5):502–518. PMID: 31288507.13. Jo KW, Kim H, Yoo DS, Hyun DK, Cheong JH, Park HK, et al. Current status of neurosurgical and neurointensive care units in Korea: a brief report on nationwide survey results. J Korean Neurosurg Soc. 2020; 63(4):519–531. PMID: 32664714.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Epidemiology and Functional Outcome of Acute Stroke Patients in Korea Using Nationwide data
- Organization of Stroke Care System: Stroke Unit and Stroke Center
- Problems and future directions for quality evaluation of the Health Insurance Review and Assessment Service
- Pneumococcal meningitis complicated by otomastoiditis and pneumocephalus confounding an acute ischemic stroke diagnosis
- Primary and Comprehensive Stroke Centers: History, Value and Certification Criteria