J Rhinol.
2025 Mar;32(1):48-54. 10.18787/jr.2025.00012.
Risk of Biliary Tract and Pancreatic Cancer Following Obstructive Sleep Apnea Diagnosis: Analysis of a National Health Insurance Database
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Inha University Hospital, Inha University School of Medicine, Incheon, Republic of Korea
- 2Department of Statistics and Actuarial Science, Soongsil University, Seoul, Republic of Korea
- 3Department of Otorhinolaryngology-Head and Neck Surgery, Konkuk University School of Medicine, Seoul, Republic of Korea
- 4Department of Otorhinolaryngology-Head and Neck Surgery, Soonchunhyang University College of Medicine, Bucheon Hospital, Bucheon, Republic of Korea
- KMID: 2565847
- DOI: http://doi.org/10.18787/jr.2025.00012
Abstract
- Background and Objectives
Obstructive sleep apnea (OSA) has been associated with an increased risk of cancer in various organs. OSA is also linked to chronic inflammation in the biliary tract and pancreas, a well-established risk factor for carcinogenesis in these organs. However, its relationship with biliary tract and pancreatic cancers remains unclear and has been rarely investigated. Therefore, we aimed to evaluate whether OSA serves as an independent risk factor for these malignancies by analyzing a nationwide healthcare claims database in South Korea.
Methods
A retrospective cohort study was conducted using the Korean National Health Insurance Service (KNHIS) database. Adults aged ≥20 years who were newly diagnosed with OSA (ICD-10: G47.30) between 2007 and 2014 were identified and propensity score-matched (1:5) with controls based on age, sex, and comorbidities. Individuals with pre-existing cancer diagnoses were excluded. The primary endpoints were the incidence of overall cancer, biliary tract cancer (C23–C24), and pancreatic cancer (C25). Cox proportional hazards regression models were used to calculate hazard ratios (HRs), adjusting for demographic and clinical factors.
Results
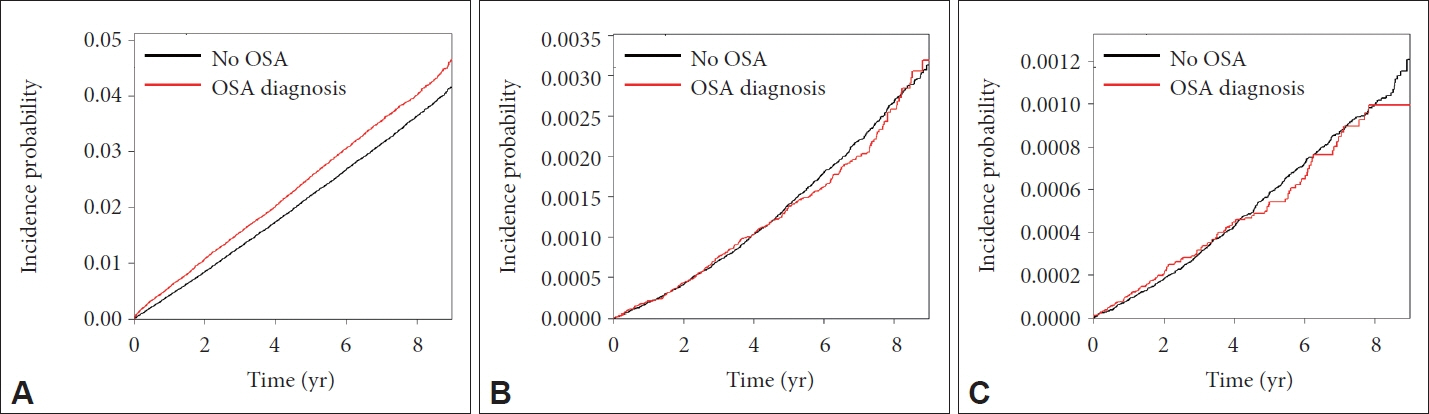
A total of 1,191,444 individuals were included, comprising 198,574 patients diagnosed with OSA and 992,870 matched controls. OSA was associated with an increased overall cancer incidence (HR, 1.132; 95% confidence interval [CI], 1.097–1.169); however, it was not significantly associated with pancreatic cancer (HR, 0.941; 95% CI, 0.823–1.072) or biliary tract cancer (HR, 0.931; 95% CI, 0.751–1.142). Subgroup analyses stratified by sex and age revealed no statistically significant associations across these groups.
Conclusion
Our findings do not support OSA as an independent risk factor for biliary tract or pancreatic cancers.
Figure
Reference
-
References
1. McNicholas WT, Pevernagie D. Obstructive sleep apnea: transition from pathophysiology to an integrative disease model. J Sleep Res. 2022; 31(4):e13616.
Article2. Mao Z, Zheng P, Zhu X, Wang L, Zhang F, Liu H, et al. Obstructive sleep apnea hypopnea syndrome and vascular lesions: an update on what we currently know. Sleep Med. 2024; 119:296–311.
Article3. Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MSM, Morrell MJ, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019; 7(8):687–98.
Article4. Slowik JM, Sankari A, Collen JF. Obstructive Sleep Apnea [Updated 2024 Mar 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 [cited 2025 Jan 21]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459252/.5. Kim J, In K, Kim J, You S, Kang K, Shim J, et al. Prevalence of sleep-disordered breathing in middle-aged Korean men and women. Am J Respir Crit Care Med. 2004; 170(10):1108–13.
Article6. Bonsignore MR, Baiamonte P, Mazzuca E, Castrogiovanni A, Marrone O. Obstructive sleep apnea and comorbidities: a dangerous liaison. Multidiscip Respir Med. 2019; 14:8.
Article7. Doumit J, Prasad B. Sleep apnea in type 2 diabetes. Diabetes Spectr. 2016; 29(1):14–9.
Article8. Thareja S, Mandapalli R, Shaik F, Rajeev Pillai A, Palaniswamy G, Sahu S, et al. Impact of obstructive sleep apnea on cardiovascular health: a systematic review. Cureus. 2024; 16(10):e71940.
Article9. Gleeson M, McNicholas WT. Bidirectional relationships of comorbidity with obstructive sleep apnoea. Eur Respir Rev. 2022; 31(164):210256.
Article10. Pardo-Manrique V, Ibarra-Enríquez CD, Serrano CD, Sanabria F, Fernandez-Trujillo L. Asthma and obstructive sleep apnea: unveiling correlations and treatable traits for comprehensive care. Chron Respir Dis. 2024; 21.
Article11. Lv R, Liu X, Zhang Y, Dong N, Wang X, He Y, et al. Pathophysiological mechanisms and therapeutic approaches in obstructive sleep apnea syndrome. Signal Transduct Target Ther. 2023; 8(1):218.
Article12. Gozal D, Ham SA, Mokhlesi B. Sleep apnea and cancer: analysis of a nationwide population sample. Sleep. 2016; 39(8):1493–500.
Article13. Chang JL, Goldberg AN, Alt JA, Mohammed A, Ashbrook L, Auckley D, et al. International consensus statement on obstructive sleep apnea. Int Forum Allergy Rhinol. 2023; 13(7):1061–482.14. Choi JH, Lee JY, Lim YC, Kim JK, Han KD, Cho JH. Association between obstructive sleep apnea and thyroid cancer incidence: a national health insurance data study. Eur Arch Otorhinolaryngol. 2021; 278(11):4569–74.
Article15. Yap DWT, Tan NKW, Tan BKJ, Teo YH, Tan VKM, See A, et al. The association of obstructive sleep apnea with breast cancer incidence and mortality: a systematic review and meta-analysis. J Breast Cancer. 2022; 25(3):149–63.
Article16. Choi JH, Lee JY, Han KD, Lim YC, Cho JH. Association between obstructive sleep apnoea and breast cancer: The Korean National Health Insurance Service Data 2007-2014. Sci Rep. 2019; 9:19044.
Article17. Cho J, Jo S. Association of obstructive sleep apnea with risk of lung cancer: a nationwide cohort study in Korea. Sci Rep. 2024; 14:12394.
Article18. Park MJ, Han KD, Cho JH, Choi JH. Incidence disparities of obstructive sleep apnea-associated lung cancer by gender; Korean National Health Insurance data analysis. Front Oncol. 2023; 13:1214279.
Article19. Chen CY, Hu JM, Shen CJ, Chou YC, Tian YF, Chen YC, et al. Increased incidence of colorectal cancer with obstructive sleep apnea: a nationwide population-based cohort study. Sleep Med. 2020; 66:15–20.
Article20. Cho JH, Lim YC, Han KD, Lee JY, Choi JH. The incidence of malignant brain tumors is increased in patients with obstructive sleep apnea: a national health insurance survey. PLoS One. 2020; 15(11):e0241598.
Article21. Lee EJ, Han KD, Kim SY, Suh JD, Kim JK, Cho JH. Increased incidence of leukemia in patients with obstructive sleep apnea: results from the national insurance claim data 2007-2014. Sleep Med. 2022; 96:113–18.
Article22. Yoon DW, So D, Min S, Kim J, Lee M, Khalmuratova R, et al. Accelerated tumor growth under intermittent hypoxia is associated with hypoxia-inducible factor-1-dependent adaptive responses to hypoxia. Oncotarget. 2017; 8(37):61592–603.
Article23. Moriondo G, Soccio P, Minoves M, Scioscia G, Tondo P, Foschino Barbaro MP, et al. Intermittent hypoxia mediates cancer development and progression through HIF-1 and miRNA regulation. Arch Bronconeumol. 2023; 59(10):629–37. English, Spanish.
Article24. Lin J, Wang H, Chen X, Han L, Huang Z, Lyu G, et al. Obstructive sleep apnoea is independently associated with non-alcoholic fatty pancreatic disease. Scand J Gastroenterol. 2024; 59(11):1252–8.
Article25. Mirrakhimov AE. Nonalcoholic fatty pancreatic disease and cardiometabolic risk: is there is a place for obstructive sleep apnea? Cardiovasc Diabetol. 2014; 13:29.
Article26. Dal Molin M, Brant A, Blackford AL, Griffin JF, Shindo K, Barkley T, et al. Obstructive sleep apnea and pathological characteristics of resected pancreatic ductal adenocarcinoma. PLoS One. 2016; 11(10):e0164195.
Article27. Yan W, Zhou J, Jiang M, Kong Y, Qin H, Qi Y, et al. Obstructive sleep apnea and 19 gastrointestinal diseases: a Mendelian randomization study. Front Psychiatry. 2024; 15:1256116.
Article28. National Cancer Information Center. Cancer Statistics by Age Groups [Internet]. Goyang: National Cancer Information Center;2022. [cited 2025 Jan 21]. Available from: https://www.cancer.go.kr/lay1/S1T639C642/contents.do.29. Wu D, Zhao Z, Chen C, Lu G, Wang C, Gao S, et al. Impact of obstructive sleep apnea on cancer risk: a systematic review and meta-analysis. Sleep Breath. 2023; 27(3):843–52.
Article30. Gandhi S, de la Fuente J, Murad MH, Majumder S. Chronic pancreatitis is a risk factor for pancreatic cancer, and incidence increases with duration of disease: a systematic review and meta-analysis. Clin Transl Gastroenterol. 2022; 13(3):e00463.
Article31. Zhang Z, Jiang C, Yin B, Wang H, Zong J, Yang T, et al. Investigating the causal links between obstructive sleep apnea and gastrointestinal diseases mediated by metabolic syndrome through mendelian randomization. Sci Rep. 2024; 14:26247.
Article32. Shoucair S, Pu N, Habib JR, Thompson E, Shubert C, Burkhart RA, et al. Obstructive sleep apnea predicts pathologic response to neoadjuvant therapy in resected pancreatic ductal adenocarcinoma. MedComm (2020). 2022; 3(4):e184.
Article33. Roy S, Glaser S, Chakraborty S. Inflammation and progression of cholangiocarcinoma: role of angiogenic and lymphangiogenic mechanisms. Front Med (Lausanne). 2019; 6:293.
Article34. Tyson GL, El-Serag HB. Risk factors for cholangiocarcinoma. Hepatology. 2011; 54(1):173–84.
Article35. Alshahri TM, Abounozha S. Best evidence topic: does the presence of a large gallstone carry a higher risk of gallbladder cancer? Ann Med Surg (Lond). 2020; 61:93–96.
Article36. Nogueira L, Freedman ND, Engels EA, Warren JL, Castro F, Koshiol J. Gallstones, cholecystectomy, and risk of digestive system cancers. Am J Epidemiol. 2014; 179(6):731–9.
Article37. Loosen S, Krieg S, Krieg A, Leyh C, Luedde T, Vetter C, et al. Are sleep disorders associated with the risk of gastrointestinal cancer?—A case-control study. J Cancer Res Clin Oncol. 2023; 149(13):11369–78.
Article38. Gu C, Younas H, Jun JC. Sleep apnea: an overlooked cause of lipotoxicity? Med Hypotheses. 2017; 108:161–5.
Article