J Korean Med Sci.
2024 Dec;39(47):e305. 10.3346/jkms.2024.39.e305.
Single-Dose Versus Multiple-Dose Prophylactic Antibiotics in Minimally Invasive Colorectal Surgery: A Propensity Score Matched Analysis
- Affiliations
-
- 1Department of Surgery, Seoul National University Hospital, Seoul, Korea
- 2Department of Surgery, Seoul National University College of Medicine, Seoul, Korea
- 3Cancer Research Institute, Seoul National University, Seoul, Korea
- KMID: 2562329
- DOI: http://doi.org/10.3346/jkms.2024.39.e305
Abstract
- Background
Recent guidelines about preventing surgical site infections (SSIs) recommend against the administration of prophylactic antibiotics after surgery. However, many colorectal surgeons still prefer prolonged use of prophylactic antibiotics. While minimally invasive surgery (MIS) has become the standard for colorectal cancer surgery, there were few studies about proper dose of prophylactic antibiotics in minimally invasive colorectal surgery.
Methods
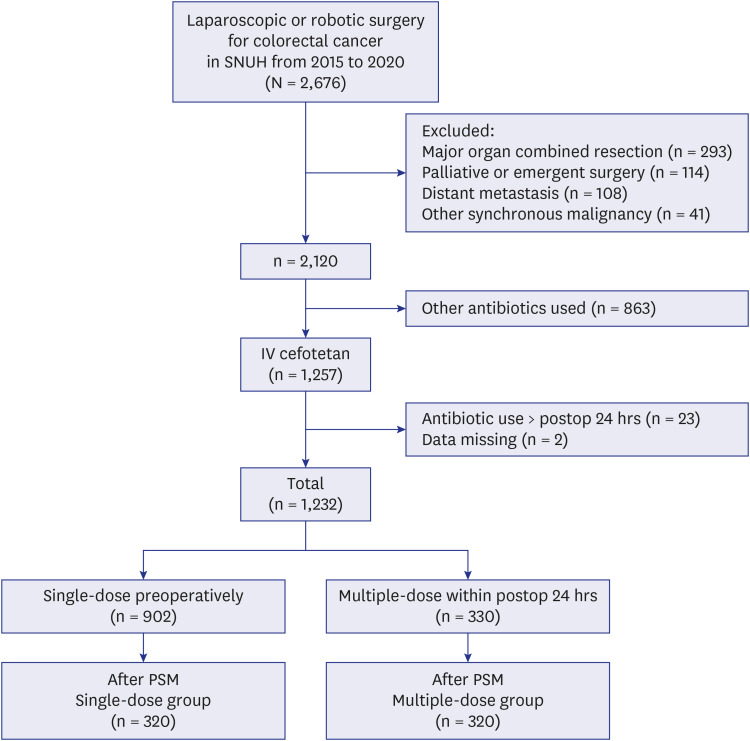
This is a retrospective study. All patients underwent elective colorectal cancer surgery using MIS. Intravenous cefotetan was administered as a prophylactic antibiotic. Two groups were classified according to the dose of prophylactic antibiotics: a group using a single dose preoperatively (single-dose group) and a group using a preoperative single dose plus additional doses within 24 hours after surgery (multiple-dose group). The SSI rates between the two groups were compared before and after propensity score matching (PSM). Risk factors of SSIs were assessed using univariate and multivariable analysis.
Results
There were 902 patients in the single-dose group and 330 patients in the multipledose group. After PSM, 320 patients were included in each group. There were no differences in baseline characteristics and surgical outcomes except the length of hospital stay. SSI rates were not different between the two groups before and after PSM (before 2.0% vs. 2.1%, P = 0.890; after 0.9% vs. 1.9%, P = 0.505). In multivariable analysis, American Society of Anesthesiologists class 3, rectal surgery, intraoperative transfusion, and larger tumor size were identified as independent factors associated with SSI incidence.
Conclusion
A single preoperative dose of prophylactic antibiotics may be sufficient to prevent SSIs in elective MIS for colorectal cancer.
Keyword
Figure
Reference
-
1. Keenan JE, Speicher PJ, Thacker JK, Walter M, Kuchibhatla M, Mantyh CR. The preventive surgical site infection bundle in colorectal surgery: an effective approach to surgical site infection reduction and health care cost savings. JAMA Surg. 2014; 149(10):1045–1052. PMID: 25163027.2. Petrosillo N, Drapeau CM, Nicastri E, Martini L, Ippolito G, Moro ML, et al. Surgical site infections in Italian Hospitals: a prospective multicenter study. BMC Infect Dis. 2008; 8(1):34. PMID: 18328101.3. Darouiche RO, Wall MJ Jr, Itani KM, Otterson MF, Webb AL, Carrick MM, et al. Chlorhexidine-alcohol versus povidone-iodine for surgical-site antisepsis. N Engl J Med. 2010; 362(1):18–26. PMID: 20054046.4. Tanner J, Khan D, Aplin C, Ball J, Thomas M, Bankart J. Post-discharge surveillance to identify colorectal surgical site infection rates and related costs. J Hosp Infect. 2009; 72(3):243–250. PMID: 19446918.5. Bernatz JT, Safdar N, Hetzel S, Anderson PA. Antibiotic overuse is a major risk factor for clostridium difficile infection in surgical patients. Infect Control Hosp Epidemiol. 2017; 38(10):1254–1257. PMID: 28756789.6. Branch-Elliman W, O’Brien W, Strymish J, Itani K, Wyatt C, Gupta K. Association of duration and type of surgical prophylaxis with antimicrobial-associated adverse events. JAMA Surg. 2019; 154(7):590–598. PMID: 31017647.7. Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, Bolon MK, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health Syst Pharm. 2013; 70(3):195–283. PMID: 23327981.8. World Health Organization. Global Guidelines for the Prevention of Surgical Site Infection. Geneva, Switzerland: World Health Organization;2018.9. Berríos-Torres SI, Umscheid CA, Bratzler DW, Leas B, Stone EC, Kelz RR, et al. Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg. 2017; 152(8):784–791. PMID: 28467526.10. Yamauchi S, Matsuyama T, Tokunaga M, Kinugasa Y. Minimally invasive surgery for colorectal cancer. JMA J. 2021; 4(1):17–23. PMID: 33575499.11. Nelson H, Sargent DJ, Wieand HS, Fleshman J, Anvari M, Stryker SJ, et al. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004; 350(20):2050–2059. PMID: 15141043.12. Caroff DA, Chan C, Kleinman K, Calderwood MS, Wolf R, Wick EC, et al. Association of open approach vs laparoscopic approach with risk of surgical site infection after colon surgery. JAMA Netw Open. 2019; 2(10):e1913570. PMID: 31626316.13. Esemuede IO, Gabre-Kidan A, Fowler DL, Kiran RP. Risk of readmission after laparoscopic vs. open colorectal surgery. Int J Colorectal Dis. 2015; 30(11):1489–1494. PMID: 26264049.14. Wilson MZ, Hollenbeak CS, Stewart DB. Laparoscopic colectomy is associated with a lower incidence of postoperative complications than open colectomy: a propensity score-matched cohort analysis. Colorectal Dis. 2014; 16(5):382–389. PMID: 24373345.15. Kulkarni N, Arulampalam T. Laparoscopic surgery reduces the incidence of surgical site infections compared to the open approach for colorectal procedures: a meta-analysis. Tech Coloproctol. 2020; 24(10):1017–1024. PMID: 32648141.16. Kang BM, Lee KY, Park SJ, Lee SH. Mechanical bowel preparation and prophylactic antibiotic administration in colorectal surgery: a survey of the current status in Korea. Ann Coloproctol. 2013; 29(4):160–166. PMID: 24032117.17. Al-Taher M, Okamoto N, Mutter D, Stassen LPS, Marescaux J, Diana M, et al. International survey among surgeons on laparoscopic right hemicolectomy: the gap between guidelines and reality. Surg Endosc. 2022; 36(8):5840–5853. PMID: 35064320.18. Poon JT, Law WL, Wong IW, Ching PT, Wong LM, Fan JK, et al. Impact of laparoscopic colorectal resection on surgical site infection. Ann Surg. 2009; 249(1):77–81. PMID: 19106679.19. Kiran RP, El-Gazzaz GH, Vogel JD, Remzi FH. Laparoscopic approach significantly reduces surgical site infections after colorectal surgery: data from national surgical quality improvement program. J Am Coll Surg. 2010; 211(2):232–238. PMID: 20670861.20. Arkenbosch J, Miyagaki H, Kumara HM, Yan X, Cekic V, Whelan RL. Efficacy of laparoscopic-assisted approach for reversal of Hartmann’s procedure: results from the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database. Surg Endosc. 2015; 29(8):2109–2114. PMID: 25361651.21. Pasam RT, Esemuede IO, Lee-Kong SA, Kiran RP. The minimally invasive approach is associated with reduced surgical site infections in obese patients undergoing proctectomy. Tech Coloproctol. 2015; 19(12):733–743. PMID: 26415943.22. Aimaq R, Akopian G, Kaufman HS. Surgical site infection rates in laparoscopic versus open colorectal surgery. Am Surg. 2011; 77(10):1290–1294. PMID: 22127072.23. Sun H, Jiang H, Jiang ZW, Fang G, Dai ZX, Wang Z, et al. Analysis of risk factors for surgical site infection after colorectal surgery: a cross-sectional study in the east of China pre-COVID-19. Front Public Health. 2023; 11:1204337. PMID: 37637824.24. Fujita S, Saito N, Yamada T, Takii Y, Kondo K, Ohue M, et al. Randomized, multicenter trial of antibiotic prophylaxis in elective colorectal surgery: single dose vs 3 doses of a second-generation cephalosporin without metronidazole and oral antibiotics. Arch Surg. 2007; 142(7):657–661. PMID: 17638804.25. Jones RN. Cefmetazole (CS-1170), a “new” cephamycin with a decade of clinical experience. Diagn Microbiol Infect Dis. 1989; 12(5):367–379. PMID: 2692950.26. Martin C, Thomachot L, Albanese J. Clinical pharmacokinetics of cefotetan. Clin Pharmacokinet. 1994; 26(4):248–258. PMID: 8013159.27. Yamamoto S, Fujita S, Ishiguro S, Akasu T, Moriya Y. Wound infection after a laparoscopic resection for colorectal cancer. Surg Today. 2008; 38(7):618–622. PMID: 18612786.28. Suzuki T, Sadahiro S, Maeda Y, Tanaka A, Okada K, Kamijo A. Optimal duration of prophylactic antibiotic administration for elective colon cancer surgery: a randomized, clinical trial. Surgery. 2011; 149(2):171–178. PMID: 20655559.29. Bratzler DW, Houck PM; American Academy of Orthopaedic Surgeons; American Association of Critical Care Nurses; American Association of Nurse Anesthetists, et al. Surgical Infection Prevention Guidelines Writers Workgroup. Antimicrobial prophylaxis for surgery: an advisory statement from the National Surgical Infection Prevention Project. Clin Infect Dis. 2004; 38(12):1706–1715. PMID: 15227616.30. Jeong WK, Park JW, Lim SB, Choi HS, Jeong SY. Cefotetan versus conventional triple antibiotic prophylaxis in elective colorectal cancer surgery. J Korean Med Sci. 2010; 25(3):429–434. PMID: 20191043.31. Anderson DJ, Podgorny K, Berríos-Torres SI, Bratzler DW, Dellinger EP, Greene L, et al. Strategies to prevent surgical site infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014; 35(6):605–627. PMID: 24799638.32. Nelson RL, Gladman E, Barbateskovic M. Antimicrobial prophylaxis for colorectal surgery. Cochrane Database Syst Rev. 2014; 2014(5):CD001181. PMID: 24817514.33. Xu Z, Qu H, Gong Z, Kanani G, Zhang F, Ren Y, et al. Risk factors for surgical site infection in patients undergoing colorectal surgery: a meta-analysis of observational studies. PLoS One. 2021; 16(10):e0259107. PMID: 34710197.34. Gomila A, Carratalà J, Camprubí D, Shaw E, Badia JM, Cruz A, et al. Risk factors and outcomes of organ-space surgical site infections after elective colon and rectal surgery. Antimicrob Resist Infect Control. 2017; 6(1):40. PMID: 28439408.35. Konishi T, Watanabe T, Kishimoto J, Nagawa H. Elective colon and rectal surgery differ in risk factors for wound infection: results of prospective surveillance. Ann Surg. 2006; 244(5):758–763. PMID: 17060769.36. Degrate L, Garancini M, Misani M, Poli S, Nobili C, Romano F, et al. Right colon, left colon, and rectal surgeries are not similar for surgical site infection development. Analysis of 277 elective and urgent colorectal resections. Int J Colorectal Dis. 2011; 26(1):61–69. PMID: 20922541.37. Nasser H, Ivanics T, Leonard-Murali S, Stefanou A. Risk factors for surgical site infection after laparoscopic colectomy: an NSQIP database analysis. J Surg Res. 2020; 249:25–33. PMID: 31918327.38. Xu Z, Qu H, Kanani G, Guo Z, Ren Y, Chen X. Update on risk factors of surgical site infection in colorectal cancer: a systematic review and meta-analysis. Int J Colorectal Dis. 2020; 35(12):2147–2156. PMID: 32748113.39. Waltz PK, Zuckerbraun BS. Surgical site infections and associated operative characteristics. Surg Infect (Larchmt). 2017; 18(4):447–450. PMID: 28448197.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A propensity score-matched analysis of advanced energy devices and conventional monopolar device for colorectal cancer surgery: comparison of clinical and oncologic outcomes
- Minimally invasive surgery for colorectal cancer, a look back to look forward: a personal history
- Comparative Study of Single-dose Prophylactic Antibiotics after Cord Clamping Vs. Multi-dose Postoperative Antibiotics in Operative Complications after Elective Cesarean Section
- Open Versus Minimally Invasive Spine Surgery Remains a Global Question – A Commentary on “Open Versus Minimally Invasive Spine Surgery in the Treatment of Single-Level Degenerative Lumbar Spondylolisthesis: An AO Spine Global Cross-Sectional Study”
- Feasibility of No Prophylactic Antibiotics Use in Patients Undergoing Total Laparoscopic Distal Gastrectomy for Gastric Carcinoma: a Propensity Score-Matched Case-Control Study