Ann Surg Treat Res.
2022 Nov;103(5):290-296. 10.4174/astr.2022.103.5.290.
A propensity score-matched analysis of advanced energy devices and conventional monopolar device for colorectal cancer surgery: comparison of clinical and oncologic outcomes
- Affiliations
-
- 1Department of Surgery, Keimyung University Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea
- KMID: 2534853
- DOI: http://doi.org/10.4174/astr.2022.103.5.290
Abstract
- Purpose
The safety, efficiency, and versatility of novel surgical energy devices have been proved by recent studies. This study aims to investigate the impact of surgical energy devices on operative and oncologic outcomes of minimally invasive colorectal cancer surgery.
Methods
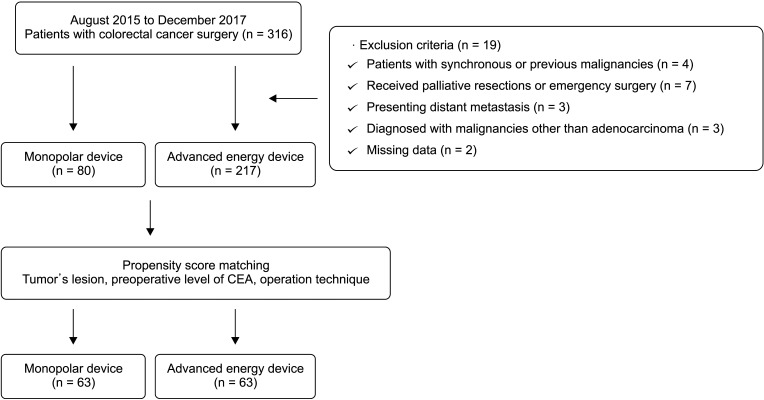
The study group included 80 patients who underwent minimally invasive colorectal cancer surgery with a conventional monopolar device and 217 patients with advanced surgical energy devices between August 2015 and December 2017. The propensity score matching for tumor lesion, preoperative level of CEA, and operation technique produced 63 matched pairs.
Results
In patient characteristics, there was no significant difference between the groups after the propensity score matching. The amount of blood loss (72 mL vs. 54 mL, P = 0.123) and conversion cases to another surgery (11.1% vs. 4.8%, P = 0.187) tended to be higher in monopolar group, while operation time and intraoperative complications were not significantly different. The short-term clinical outcomes including time to soft diet, the length of hospital stays, and the morbidity within 30 days after surgery or pathologic outcomes were comparable between the groups. During the median follow-up of 52.9 and 51.1 months in each study group, the 5-year overall survival rates of the monopolar and advanced energy groups were 84.6% and 91.6% (P = 0.276), and the 5-year disease-free survival rates were 78.0% and 84.6% (P = 0.328), respectively.
Conclusion
The use of surgical energy devices based on surgeons’ preference did not show significant impact on operative and long-term outcomes compared with conventional monopolar devices in minimally invasive colorectal cancer surgery.
Keyword
Figure
Reference
-
1. Jacobs M, Verdeja JC, Goldstein HS. Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc. 1991; 1:144–150. PMID: 1688289.2. Bae SU, Jeong WK, Baek SK. Robot-assisted colectomy for left-sided colon cancer: comparison of reduced-port and conventional multi-port robotic surgery. J Laparoendosc Adv Surg Tech A. 2017; 27:398–403. PMID: 27870592.
Article3. Jaloun HE, Lee IK, Kim MK, Sung NY, Turkistani SA, Park SM, et al. Influence of the enhanced recovery after surgery protocol on postoperative inflammation and short-term postoperative surgical outcomes after colorectal cancer surgery. Ann Coloproctol. 2020; 36:264–272. PMID: 32674557.
Article4. Colon Cancer Laparoscopic or Open Resection Study Group. Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, et al. Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol. 2009; 10:44–52. PMID: 19071061.
Article5. Juo YY, Hyder O, Haider AH, Camp M, Lidor A, Ahuja N. Is minimally invasive colon resection better than traditional approaches?: first comprehensive national examination with propensity score matching. JAMA Surg. 2014; 149:177–184. PMID: 24352653.
Article6. Oh CK, Huh JW, Lee YJ, Choi MS, Pyo DH, Lee SC, et al. Long-term oncologic outcome of postoperative complications after colorectal cancer surgery. Ann Coloproctol. 2020; 36:273–280. PMID: 32054256.
Article7. Milsom J, Trencheva K, Monette S, Pavoor R, Shukla P, Ma J, et al. Evaluation of the safety, efficacy, and versatility of a new surgical energy device (THUNDERBEAT) in comparison with Harmonic ACE, LigaSure V, and EnSeal devices in a porcine model. J Laparoendosc Adv Surg Tech A. 2012; 22:378–386. PMID: 22364404.
Article8. Allaix ME, Furnée EJ, Arezzo A, Mistrangelo M, Morino M. Energy sources for laparoscopic colorectal surgery: is one better than the others? J Laparoendosc Adv Surg Tech A. 2016; 26:264–269. PMID: 26986017.
Article9. Hotta T, Takifuji K, Yokoyama S, Matsuda K, Higashiguchi T, Tominaga T, et al. Literature review of the energy sources for performing laparoscopic colorectal surgery. World J Gastrointest Surg. 2012; 4:1–8. PMID: 22347536.
Article10. Suhardja TS, Norhadi S, Ee E, Hodgkins B. Comparison of the Thunderbeat and other energy devices in laparoscopic colorectal resection: a single-center experience. J Laparoendosc Adv Surg Tech A. 2018; 28:1417–1421. PMID: 29870293.
Article11. Tou S, Malik AI, Wexner SD, Nelson RL. Energy source instruments for laparoscopic colectomy. Cochrane Database Syst Rev. 2011; (5):CD007886. PMID: 21563161.
Article12. Milsom JW, Trencheva K, Sonoda T, Nandakumar G, Shukla PJ, Lee S. A prospective trial evaluating the clinical performance of a novel surgical energy device in laparoscopic colon surgery. Surg Endosc. 2015; 29:1161–1166. PMID: 25159634.
Article13. Allaix ME, Arezzo A, Giraudo G, Arolfo S, Mistrangelo M, Morino M. The Thunderbeat and other energy devices in laparoscopic colorectal resections: analysis of outcomes and costs. J Laparoendosc Adv Surg Tech A. 2017; 27:1225–1229. PMID: 27420752.
Article14. Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S. Standardized surgery for colonic cancer: complete mesocolic excision and central ligation: technical notes and outcome. Colorectal Dis. 2009; 11:354–365. PMID: 19016817.15. Liberman M, Khereba M, Goudie E, Kazakov J, Thiffault V, Lafontaine E, et al. Pilot study of pulmonary arterial branch sealing using energy devices in an ex vivo model. J Thorac Cardiovasc Surg. 2014; 148:3219–3223. PMID: 25125207.
Article16. Seehofer D, Mogl M, Boas-Knoop S, Unger J, Schirmeier A, Chopra S, et al. Safety and efficacy of new integrated bipolar and ultrasonic scissors compared to conventional laparoscopic 5-mm sealing and cutting instruments. Surg Endosc. 2012; 26:2541–2549. PMID: 22447285.
Article17. Fagotti A, Vizzielli G, Fanfani F, Gallotta V, Rossitto C, Costantini B, et al. Randomized study comparing use of THUNDERBEAT technology vs standard electrosurgery during laparoscopic radical hysterectomy and pelvic lymphadenectomy for gynecologic cancer. J Minim Invasive Gynecol. 2014; 21:447–453. PMID: 24325899.
Article18. Akagi Y, Adachi Y, Kinugasa T, Oka Y, Mizobe T, Shirouzu K. Lymph node evaluation and survival in colorectal cancer: review of population-based, prospective studies. Anticancer Res. 2013; 33:2839–2847. PMID: 23780968.19. Nakamura Y, Hokuto D, Koyama F, Matsuo Y, Nomi T, Yoshikawa T, et al. The prognosis and recurrence pattern of right- and left-sided colon cancer in stage II, stage III, and liver metastasis after curative resection. Ann Coloproctol. 2021; 37:326–336. PMID: 32972100.
Article20. Tanaka R, Gitelis M, Meiselman D, Abar B, Zapf M, Carbray J, et al. Evaluation of vessel sealing performance among ultrasonic devices in a porcine model. Surg Innov. 2015; 22:338–343. PMID: 25851145.
Article21. Liang J, Fazio V, Lavery I, Remzi F, Hull T, Strong S, et al. Primacy of surgery for colorectal cancer. Br J Surg. 2015; 102:847–852. PMID: 25832316.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Use of Advanced Energy Devices and Fiberoptic Retractors in Single-Incision Breast-Conserving Surgery for Breast Cancer
- Spotlight on laparoscopy in the surgical resection of locally advanced rectal cancer: multicenter propensity score match study
- Current status of robotic surgery for colorectal cancer: A review
- Effectiveness of the EnSeal(TM) System in Colorectal Cancer Surgery: A Pilot Randomized Study for Comparison with LigaSure(TM)
- Long-term outcomes after Natural Orifice Specimen Extraction versus conventional laparoscopy-assisted surgery for rectal cancer: a matched case-control study