Ann Surg Treat Res.
2018 Jan;94(1):26-35. 10.4174/astr.2018.94.1.26.
Long-term outcomes after Natural Orifice Specimen Extraction versus conventional laparoscopy-assisted surgery for rectal cancer: a matched case-control study
- Affiliations
-
- 1Colorectal Cancer Center, Kyungpook National University Medical Center, Kyungpook National University School of Medicine, Daegu, Korea. kyuschoi@mail.knu.ac.kr
- 2Department of Anesthesiology and Pain Medicine, Chung-Ang University College of Medicine, Seoul, Korea.
- KMID: 2405336
- DOI: http://doi.org/10.4174/astr.2018.94.1.26
Abstract
- PURPOSE
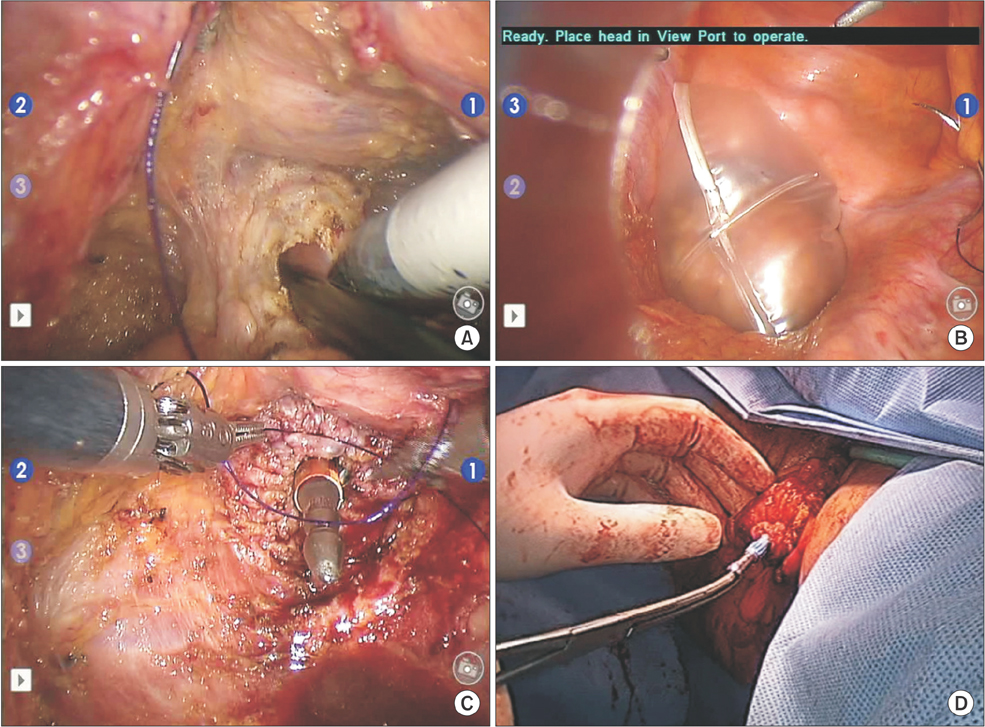
The aim of this study was to compare the long-term outcomes of total laparoscopic surgery with Natural Orifice Specimen Extraction (NOSE) with those for conventional laparoscopy (CL)-assisted surgery for treating rectal cancers.
METHODS
We reviewed the prospectively collected records of 844 patients (163 NOSE and 681 CL) who underwent curative surgery for mid- or upper rectal cancers from January 2006 to November 2012. We applied propensity score analyses and compared oncological outcomes for the NOSE and CL groups in a 1:1 matched cohort.
RESULTS
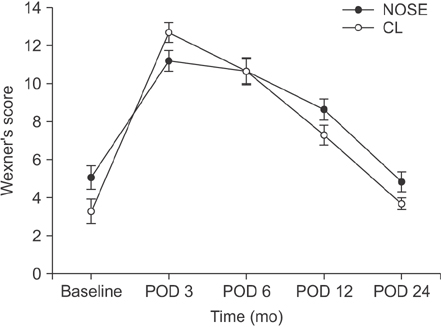
After propensity score matching, each group included 138 patients; the NOSE and CL groups did not differ significantly in terms of baseline clinical characteristics. The median follow-up was 57.7 months (interquartile range, 42.4-82.5 months). The combined 5-year local recurrence rate for all tumor stages was 4.1% (95% confidence interval [CI], 0.9%-7.4%) in the NOSE group and 3.0% (95% CI, 0%-6.3%) in the CL group (P = 0.355). The combined 5-year disease-free survival rates for all stages were 89.3% (95% CI, 84.3%-94.3%) in the NOSE group and 87.3% (95% CI, 81.8%-92.9%) in the CL group (P = 0.639). The postoperative mean fecal incontinence scores at 6, 12, and 24 months were similar between the 2 groups.
CONCLUSION
In our experience, NOSE for mid- and upper rectal cancer had acceptable long-term oncologic outcomes comparable to those of conventional minimal invasive surgery and seems to be a safe alternative to reduce access trauma.
MeSH Terms
Figure
Reference
-
1. Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, van der Pas MH, de Lange-de Klerk ES, et al. A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med. 2015; 372:1324–1332.
Article2. Jeong SY, Park JW, Nam BH, Kim S, Kang SB, Lim SB, et al. Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol. 2014; 15:767–774.
Article3. Park JS, Choi GS, Jun SH, Park SY, Kim HJ. Long-term outcomes after laparoscopic surgery versus open surgery for rectal cancer: a propensity score analysis. Ann Surg Oncol. 2013; 20:2633–2640.
Article4. Singh R, Omiccioli A, Hegge S, McKinley C. Does the extraction-site location in laparoscopic colorectal surgery have an impact on incisional hernia rates? Surg Endosc. 2008; 22:2596–2600.
Article5. Winslow ER, Fleshman JW, Birnbaum EH, Brunt LM. Wound complications of laparoscopic vs open colectomy. Surg Endosc. 2002; 16:1420–1425.
Article6. Romy S, Eisenring MC, Bettschart V, Petignat C, Francioli P, Troillet N. Laparoscope use and surgical site infections in digestive surgery. Ann Surg. 2008; 247:627–632.
Article7. Rolanda C, Lima E, Pego JM, Henriques-Coelho T, Silva D, Moreira I, et al. Third-generation cholecystectomy by natural orifices: transgastric and transvesical combined approach (with video). Gastrointest Endosc. 2007; 65:111–117.
Article8. Zorron R, Filgueiras M, Maggioni LC, Pombo L, Lopes Carvalho G, Lacerda Oliveira A. NOTES. Transvaginal cholecystectomy: report of the first case. Surg Innov. 2007; 14:279–283.
Article9. Wolthuis AM, Fieuws S, Van Den Bosch A, de Buck van Overstraeten A, D'Hoore A. Randomized clinical trial of laparoscopic colectomy with or without natural-orifice specimen extraction. Br J Surg. 2015; 102:630–637.
Article10. Leroy J, Costantino F, Cahill RA, D'Agostino J, Morales A, Mutter D, et al. Laparoscopic resection with transanal specimen extraction for sigmoid diverticulitis. Br J Surg. 2011; 98:1327–1334.
Article11. Park JS, Choi GS, Lim KH, Jang YS, Kim HJ, Park SY, et al. Clinical outcome of laparoscopic right hemicolectomy with transvaginal resection, anastomosis, and retrieval of specimen. Dis Colon Rectum. 2010; 53:1473–1479.12. Awad Z. Laparoscopic total colectomy with transvaginal extraction of the colon and ileorectal anastomosis. Ann Surg Oncol. 2014; 21:3029.
Article13. Melich G, Jeong DH, Hur H, Baik SH, Faria J, Kim NK, et al. Laparoscopic right hemicolectomy with complete mesocolic excision provides acceptable perioperative outcomes but is lengthy--analysis of learning curves for a novice minimally invasive surgeon. Can J Surg. 2014; 57:331–336.14. Park JS, Choi GS, Kim HJ, Park SY, Jun SH. Natural orifice specimen extraction versus conventional laparoscopically assisted right hemicolectomy. Br J Surg. 2011; 98:710–715.
Article15. Park JS, Choi GS, Lim KH, Jang YS, Jun SH. Robotic-assisted versus laparoscopic surgery for low rectal cancer: case-matched analysis of short-term outcomes. Ann Surg Oncol. 2010; 17:3195–3202.
Article16. Choi GS, Park IJ, Kang BM, Lim KH, Jun SH. A novel approach of robotic-assisted anterior resection with transanal or transvaginal retrieval of the specimen for colorectal cancer. Surg Endosc. 2009; 23:2831–2835.
Article17. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213.18. Jorge JM, Wexner SD. Etiology and management of fecal incontinence. Dis Colon Rectum. 1993; 36:77–97.
Article19. Leung AL, Cheung HY, Fok BK, Chung CC, Li MK, Tang CN. Prospective randomized trial of hybrid NOTES colectomy versus conventional laparoscopic colectomy for left-sided colonic tumors. World J Surg. 2013; 37:2678–2682.
Article20. Awad ZT, Griffin R. Laparoscopic right hemicolectomy: a comparison of natural orifice versus transabdominal specimen extraction. Surg Endosc. 2014; 28:2871–2876.
Article21. Xingmao Z, Haitao Z, Jianwei L, Huirong H, Junjie H, Zhixiang Z. Totally laparoscopic resection with natural orifice specimen extraction (NOSE) has more advantages comparing with laparoscopic-assisted resection for selected patients with sigmoid colon or rectal cancer. Int J Colorectal Dis. 2014; 29:1119–1124.
Article22. Ma B, Huang XZ, Gao P, Zhao JH, Song YX, Sun JX, et al. Laparoscopic resection with natural orifice specimen extraction versus conventional laparoscopy for colorectal disease: a meta-analysis. Int J Colorectal Dis. 2015; 30:1479–1488.
Article23. Costantino FA, Diana M, Wall J, Leroy J, Mutter D, Marescaux J. Prospective evaluation of peritoneal fluid contamination following transabdominal vs. transanal specimen extraction in laparoscopic left-sided colorectal resections. Surg Endosc. 2012; 26:1495–1500.
Article24. Uccella S, Cromi A, Bogani G, Casarin J, Serati M, Ghezzi F. Transvaginal specimen extraction at laparoscopy without concomitant hysterectomy: our experience and systematic review of the literature. J Minim Invasive Gynecol. 2013; 20:583–590.
Article25. Gill IS, Cherullo EE, Meraney AM, Borsuk F, Murphy DP, Falcone T. Vaginal extraction of the intact specimen following laparoscopic radical nephrectomy. J Urol. 2002; 167:238–241.
Article26. Mofid H, Emmermann A, Alm M, Zornig C. Transvaginal specimen removal after laparoscopic distal pancreatic resection. Langenbecks Arch Surg. 2013; 398:1001–1005.
Article27. Vereczkei A, Illenyi L, Arany A, Szabo Z, Toth L, Horváth OP. Transvaginal extraction of the laparoscopically removed spleen. Surg Endosc. 2003; 17:157.
Article28. Park YH, Kim KT, Bae JB, Kim HH. Transvaginal and transrectal natural orifice translumenal endoscopic surgery nephrectomy in a porcine survival model: comparison with conventional laparoscopic nephrectomy. J Endourol. 2015; 29:351–356.
Article29. D'Hoore A, Wolthuis AM. Laparoscopic low anterior resection and transanal pull-through for low rectal cancer: a Natural Orifice Specimen Extraction (NOSE) technique. Colorectal Dis. 2011; 13:Suppl 7. 28–31.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Natural Orifice Specimen Extraction (NOSE) with SingleStapling Anastomosis for Left Colon Cancer
- Simultaneous laparoscopic liver metastasectomy and intersphincteric resection for neuroendocrine tumor of the rectum by natural orifice specimen extraction surgery
- Laparoscopic Gastrectomy and Transvaginal Specimen Extraction in a Morbidly Obese Patient with Gastric Cancer
- Robotic Versus Laparoscopic Surgery for Rectal Cancer after Preoperative Chemoradiotherapy: Case-Matched Study of Short-Term Outcomes
- Comparison of Long-term Survival for Laparoscopic-assisted Surgery and Open Surgery for Right Colon Cancer: A Case-Control Study