Healthc Inform Res.
2024 Oct;30(4):375-386. 10.4258/hir.2024.30.4.375.
Vaccine Logistics Management Information System at Public Health Facilities in Amhara Region, Ethiopia: A Performance Evaluation
- Affiliations
-
- 1Department of Pharmaceutics and Social Pharmacy, School of Pharmacy, Addis Ababa University, Ethiopia
- 2Logistics Department, Kyrgyz State Technical University, Bishkek, Kyrgyzstan
- 3Centre for Supply Chain Improvement, University of Derby, Derby, UK
- KMID: 2560540
- DOI: http://doi.org/10.4258/hir.2024.30.4.375
Abstract
Objectives
This study aimed to evaluate the performance of vaccine logistics management information systems at public health facilities in Amhara Region, Ethiopia.
Methods
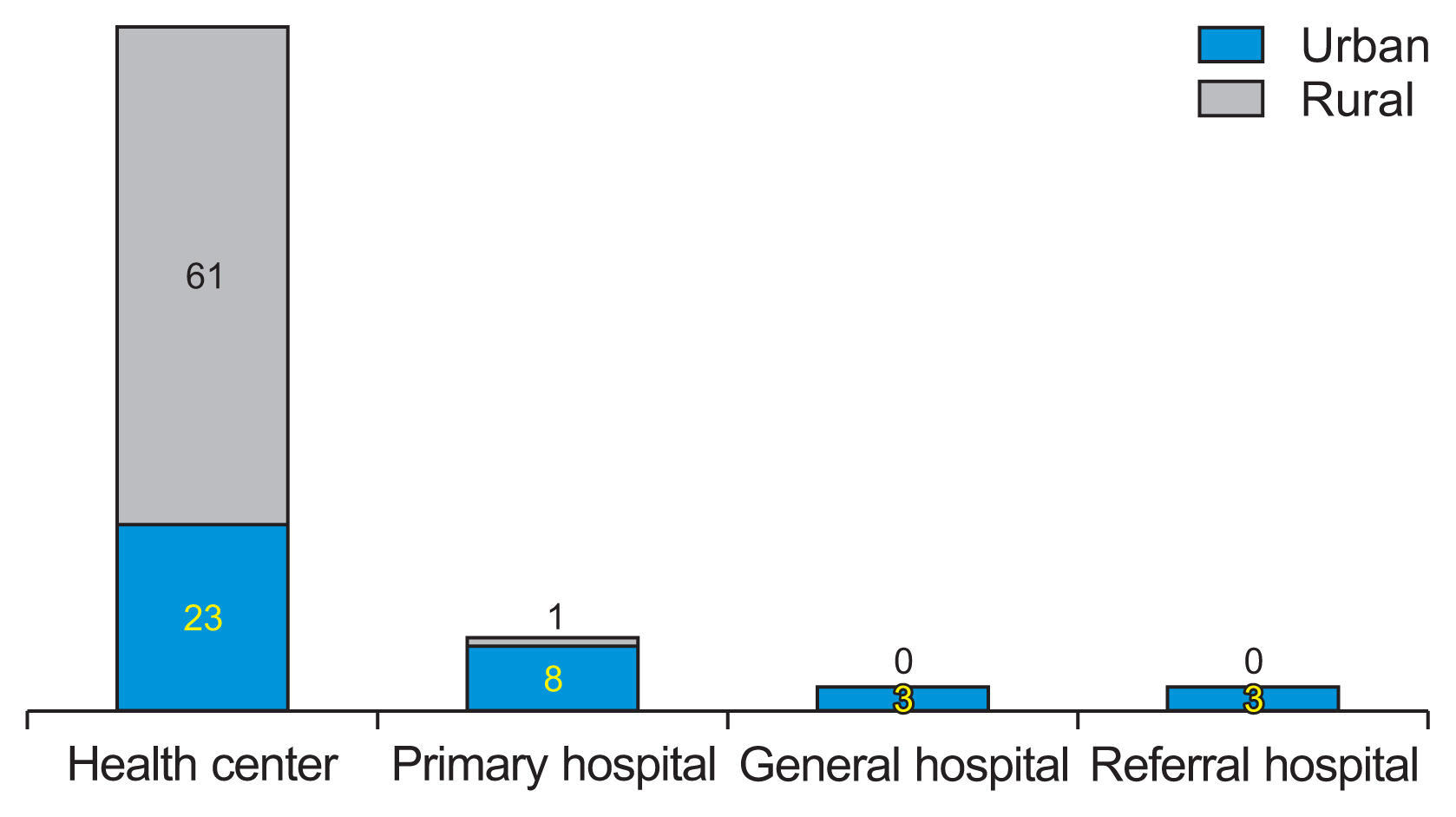
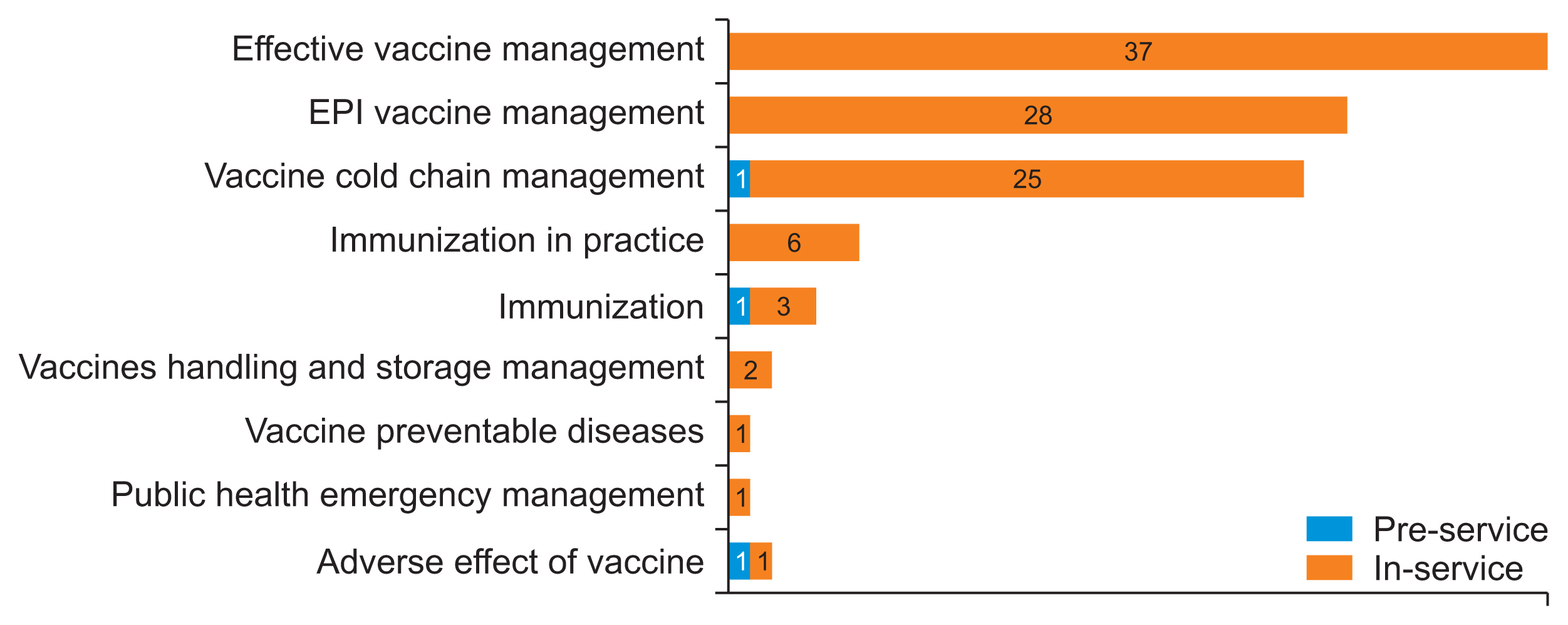
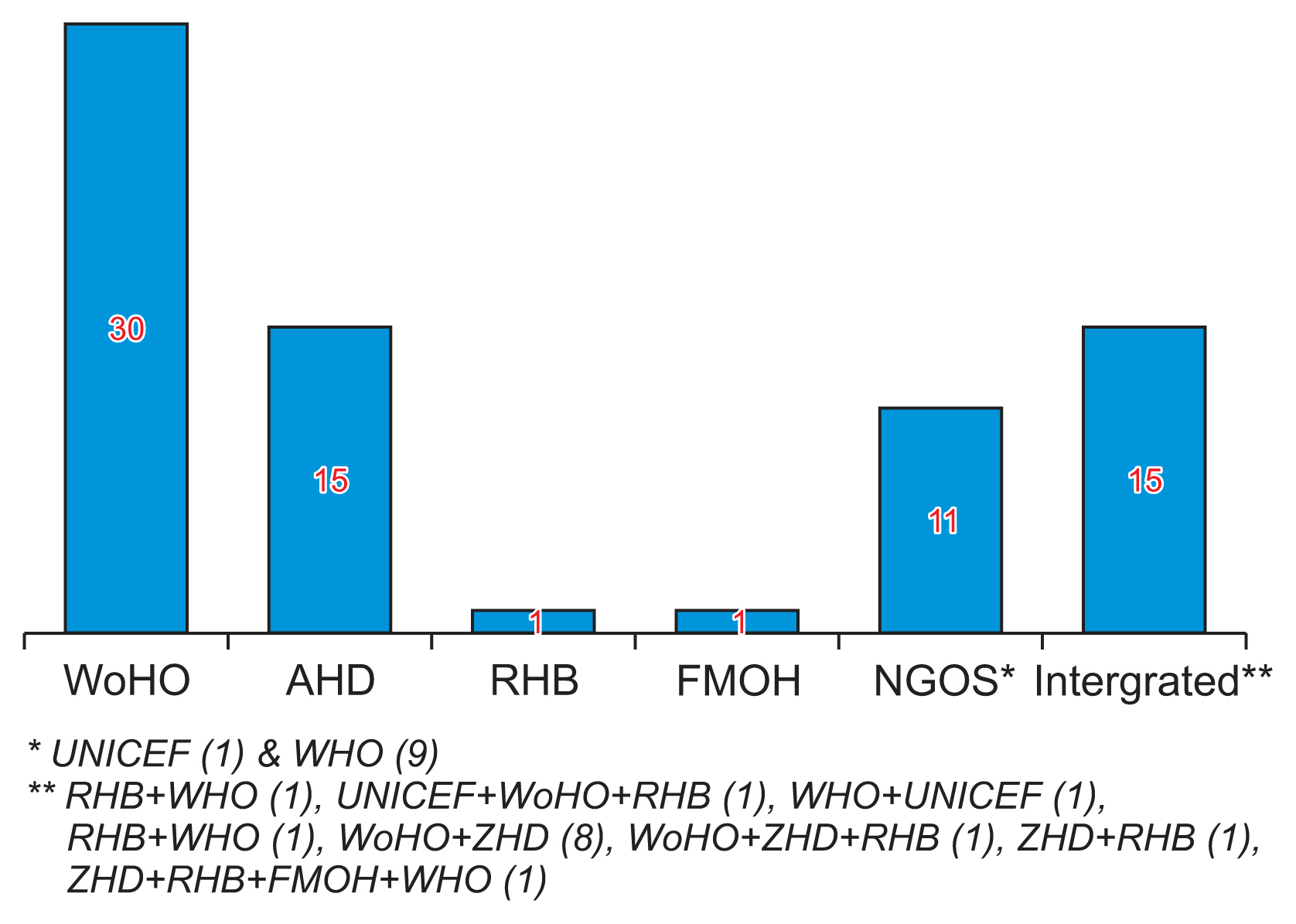
An institution-based concurrent explanatory mixed design was used at public health facilities in Amhara Region, Ethiopia. In total, 102 health facilities were selected using the multi-stage, stratified, random-sampling proportionate-to-size method. Data were collected using a structured data abstraction checklist from vaccine logistics management information system records. Additionally, experiences of Expanded Program for Immunization focal persons were gathered through interviewer-administered questionnaires.
Results
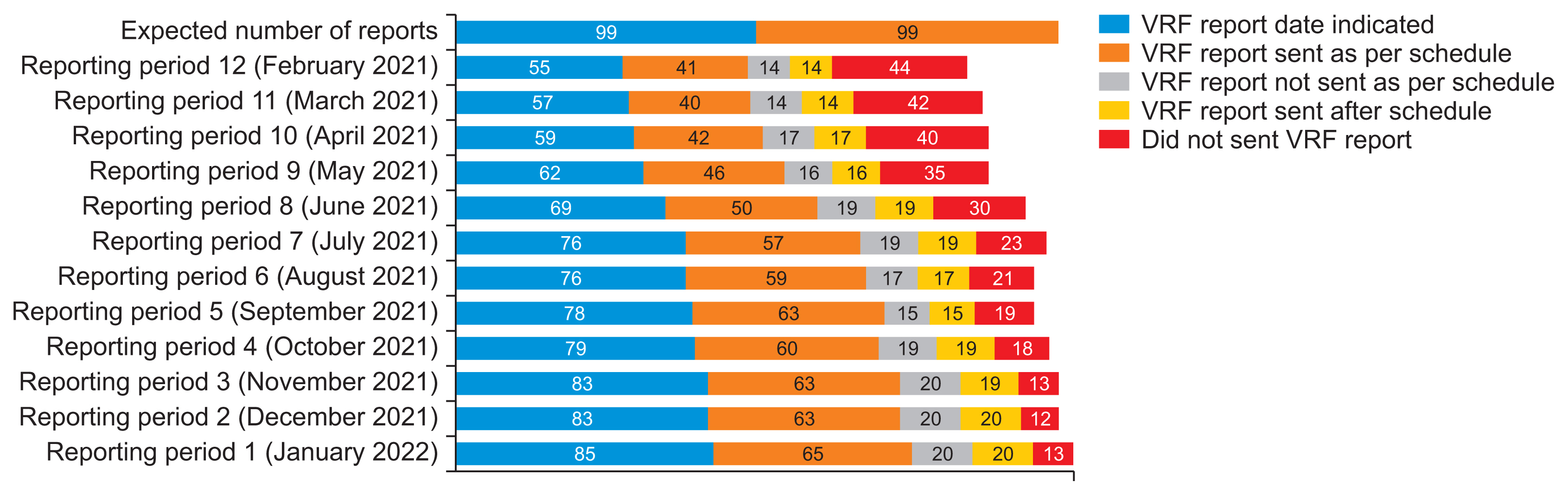
Among the 102 health facilities surveyed, 99 (97.1%) provided vaccination services during the study period. On the day of the visit, the average availability and utilization rates of 15 vaccine logistics management information system forms were 44.1% and 40.5%, respectively. The mean inventory accuracy for tracer vaccines stood at 58.3% ± 45.1%. The overall average accuracy percentages for urban and rural vaccine request form reports were 73.4% and 69.6%, respectively.
Conclusions
The performance of vaccine logistics management information systems in these public health facilities was suboptimal. Key issues identified include inconsistent use of recording forms, shortages of reporting forms, lack of digitalization, poor data quality, and a shortage of qualified staff. These findings underscore the urgent need for standardization of the vaccine logistics management information system and enhancement of data quality.
Figure
Reference
-
References
1. Stevens H, Huys I. Innovative approaches to increase access to medicines in developing countries. Front Med (Lausanne). 2017; 4:218. https://doi.org/10.3389/fmed.2017.00218.
Article2. Dowling JM, Yap CF. Communicable diseases in developing countries: stopping the global epidemics of HIV/AIDS, tuberculosis, malaria and diarrhea. London, UK: Springer;2014. https://doi.org/10.1057/9781137354785.
Article3. World Health Organization. Global status report on noncommunicable diseases 2010. Geneva, Switzerland: World Health Organization;2011.4. Remy V, Zollner Y, Heckmann U. Vaccination: the cornerstone of an efficient healthcare system. J Mark Access Health Policy. 2015; 3:https://doi.org/10.3402/jmahp.v3.27041.5. World Health Organization. Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies. Geneva, Switzerland: World Health Organization;2010. https://iris.who.int/handle/10665/258734.6. ‘t Hoen EF, Veraldi J, Toebes B, Hogerzeil HV. Medicine procurement and the use of flexibilities in the Agreement on Trade-Related Aspects of Intellectual Property Rights, 2001–2016. Bull World Health Organ. 2018; 96(3):185–93. https://doi.org/10.2471/BLT.17.199364.
Article7. Roth L, Bempong D, Babigumira JB, Banoo S, Cooke E, Jeffreys D, et al. Expanding global access to essential medicines: investment priorities for sustainably strengthening medical product regulatory systems. Global Health. 2018; 14(1):102. https://doi.org/10.1186/s12992-018-0421-2.
Article8. Yadav P. Health product supply chains in developing countries: diagnosis of the root causes of underperformance and an agenda for reform. Health Syst Reform. 2015; 1(2):142–54. https://doi.org/10.4161/23288604.2014.968005.
Article9. United States Agency for International Development. The logistics handbook: a practical guide for the supply chain management of health commodities [Internet]. Arlington (VA): John Snow Inc;2010. [cited at 2024 Oct 1]. Available from: https://pdf.usaid.gov/pdf_docs/pnaeb974.pdf.10. Federal Ministry of Health. Ethiopia national expanded program on immunization: comprehensive multi-year plan 2016–2020 [Internet]. Addis Ababa, Ethiopia: Federal Ministry of Health;2015. [cited at 2024 Oct 1]. Available from: http://repository.iifphc.org/handle/123456789/1368.11. World Health Organization. Essential programme on immunization [Internet]. Geneva, Switzerland: World Health Organization;2021. [cited at 2024 Oct 1]. Available from: https://www.who.int/teams/immunization-vaccines-and-biologicals/essential-programme-on-immunization.12. NHS England. Policy and procedure for maintaining the vaccine cold chain [Internet]. London, UK: NHS;2015. [cited at 2024 Oct 1]. Available from: https://www.england.nhs.uk/mids-east/wp-content/uploads/sites/7/2015/07/cold-chain.pdf.13. Gavi; The Global Fund. Qualified software solutions for logistics management information systems (LMIS) [Internet]. Geneva, Switzerland: Gavi;2019. [cited at 2024 Oct 1]. Available from: https://openlmis.org/wp-content/uploads/2020/04/LMIS-Selection-Guidance_2020_eng.pdf.14. John Snow Inc. Logistics management and information system [Internet]. Arlington (VA): John Snow Inc;2017. [cited at 2024 Oct 1]. Available from: https://supplychainhandbook.jsi.com/wp-content/uploads/2017/01/JSI_Supply_Chain_Manager's_Hand-book_Chpt.3_Final.pdf.15. Federal Ministry of Health. Annual Performance Report 2012 EFY 2019/2020) [Internet]. Addis Ababa, Ethiopia: Federal Ministry of Health;2020. [cited at 2024 Oct 1]. Available from: https://www.scribd.com/document/518384802/Annual-Performance-Report-2012-2019-2020.16. Mabirizi D, Phulu B, Churfo W, Mwinga S, Mazibuko G, Sagwa E, et al. Implementing an integrated pharmaceutical management information system for antiretrovirals and other medicines: lessons from Namibia. Glob Health Sci Pract. 2018; 6(4):723–35. https://doi.org/10.9745/GHSP-D-18-00157.
Article17. John Snow Inc. An unfinished journey: vaccine supply chain transformation in Ethiopia [Internet]. Arlington (VA): John Snow Inc;2019. [cited at 2024 Oct 1]. Available from: https://www.jsi.com/resource/an-unfinished-journey-vaccine-supply-chain-transformation-in-ethiopia/.18. Argaw MD, Desta BF, Tsegaye ZT, Mitiku AD, Atsa AA, Tefera BB, et al. Immunization data quality and decision making in pertussis outbreak management in southern Ethiopia: a cross sectional study. Arch Public Health. 2022; 80(1):49. https://doi.org/10.1186/s13690-022-00805-6.
Article19. Gebretnsae H, Hadgu T, Ayele B, Gebre-Egziabher E, Woldu M, Tilahun M, et al. Knowledge of vaccine handlers and status of cold chain and vaccine management in primary health care facilities of Tigray region, Northern Ethiopia: institutional based cross-sectional study. PLoS One. 2022; 17(6):e0269183. https://doi.org/10.1371/journal.pone.0269183.
Article20. Kefiyalew B, Abay S, Mamo W, Abate B, Chanyalew MA, Ayalew Y, et al. Assessment of immunization data management practices, facilitators, and barriers to immunization data quality in the health facilities of Tach Gayint district, Northwest Ethiopia. Ethiop J Health Dev. 2021; 35(3):28–38.21. Madebo TH, Gezie LD, Teklu A, Mekonnen ZA, Shahabuddin A, Tilahun B. Immunization data quality and factors influencing data generation, handling and use in Wogera District, Northern Ethiopia, 2020. Ethiop J Health Dev. 2021; 35(3):56–64.22. Nsubuga F, Luzze H, Ampeire I, Kasasa S, Toliva OB, Riolexus AA. Factors that affect immunization data quality in Kabarole District, Uganda. PLoS One. 2018; 13(9):e0203747. https://doi.org/10.1371/journal.pone.0203747.
Article23. United States Agency for International Development. Logistics Indicators Assessment Tool (LIAT) [Internet]. Arlington (VA): John Snow Inc;2008. [cited at 2024 Oct 1]. Available from: https://pdf.usaid.gov/pdf_docs/Pnadm798.pdf.24. Alemu T, Jemal A, Gashe F, Suleman S, Sudhakar S, Fekadu G. Integrated pharmaceutical logistics system implementation in selected health facilities of Ethiopia: the case of four WOLLEGA ZONES. Res Social Adm Pharm. 2021; 17(5):956–68. https://doi.org/10.1016/j.sapharm.2020.07.026.
Article25. Lopes JM, Morales CC, Alvarado M, Melo VA, Paiva LB, Dias EM, et al. Optimization methods for large-scale vaccine supply chains: a rapid review. Ann Oper Res. 2022; 316(1):699–721. https://doi.org/10.1007/s10479-022-04720-5.
Article26. Ethiopian Pharmaceuticals Supply Service (EPSS). Standard Operating Procedures (SOP) manual for the integrated pharmaceuticals logistics system in health facilities of Ethiopia [Internet]. Addis Ababa, Ethiopia: EPSS;2015. [cited at 2024 Oct 1]. Available form: https://epss.gov.et/download/standard-operating-procedures/.27. Tefera BB, Yihunie W, Bekele A. Integrated pharmaceutical logistics system implementation in Chagni primary hospital and Injibara general hospital, Awi Zone, Ethiopia. J Multidiscip Healthc. 2021; 14:1673–82. https://doi.org/10.2147/JMDH.S316595.
Article28. Rowe AK. Potential of integrated continuous surveys and quality management to support monitoring, evaluation, and the scale-up of health interventions in developing countries. Am J Trop Med Hyg. 2009; 80(6):971–9.
Article29. Fritz J, Herrick T, Gilbert SS. Estimation of health impact from digitalizing last-mile Logistics Management Information Systems (LMIS) in Ethiopia, Tanzania, and Mozambique: a Lives Saved Tool (LiST) model analysis. PLoS One. 2021; 16(10):e0258354. https://doi.org/10.1371/journal.pone.0258354.
Article30. Gilbert SS, Bulula N, Yohana E, Thompson J, Beylerian E, Werner L, et al. The impact of an integrated electronic immunization registry and logistics management information system (EIR-eLMIS) on vaccine availability in three regions in Tanzania: a pre-post and time-series analysis. Vaccine. 2020; 38(3):562–9. https://doi.org/10.1016/j.vaccine.2019.10.059.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Levels of adherence and factors associated with adherence to option B+ prevention of mother-to-child transmission among pregnant and lactating mothers in selected government health facilities of South Wollo Zone, Amhara Region, northeast Ethiopia, 2016
- The Study on Performance Evaluation and Improvement of the Information System for the Disabled
- Prevalence of goiter and associated factors among schoolchildren in northeast Ethiopia
- The Effect of Hospital SCM on Logistics Performance
- Management of vaccine safety in Korea